Abstract
Introduction
Robot-assisted surgery is often performed by experienced laparoscopic surgeons. However, this technique requires a different set of technical skills and surgeons are expected to alternate between these approaches. The aim of this study is to investigate the crossover effects when switching between laparoscopic and robot-assisted surgery.
Methods
An international multicentre crossover study was conducted. Trainees with distinctly different levels of experience were divided into three groups (novice, intermediate, expert). Each trainee performed six trials of a standardized suturing task using a laparoscopic box trainer and six trials using the da Vinci surgical robot. Both systems were equipped with the ForceSense system, measuring five force-based parameters for objective assessment of tissue handling skills. Statistical comparison was done between the sixth and seventh trial to identify transition effects. Unexpected changes in parameter outcomes after the seventh trial were further investigated.
Results
A total of 720 trials, performed by 60 participants, were analysed. The expert group increased their tissue handling forces with 46% (maximum impulse 11.5 N/s to 16.8 N/s, p = 0.05), when switching from robot-assisted surgery to laparoscopy. When switching from laparoscopy to robot-assisted surgery, intermediates and experts significantly decreased in motion efficiency (time (sec), resp. 68 vs. 100, p = 0.05, and 44 vs. 84, p = 0.05). Further investigation between the seventh and ninth trial showed that the intermediate group increased their force exertion with 78% (5.1 N vs. 9.1 N, p = 0.04), when switching to robot-assisted surgery.
Conclusion
The crossover effects in technical skills between laparoscopic and robot-assisted surgery are highly depended on the prior experience with laparoscopic surgery. Where experts can alternate between approaches without impairment of technical skills, novices and intermediates should be aware of decay in efficiency of movement and tissue handling skills that could impact patient safety. Therefore, additional simulation training is advised to prevent from undesired events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Robot-assisted surgery (RAS) is increasingly being performed [1,2,3]. Consequently, surgeons are expected to master a different spectrum of technical skills. While laparoscopy surgery (LS) is still frequently being performed, it occurs that surgeons switch between approaches in the operating room (OR) with short periods of time in between. Utilizing a robotic system does impact the posture of the surgeon leading to different muscle stress locations and differences in fatigue progression [4, 5]. Moreover, RAS gives a different touch and feel of the instruments, the tissues and its environment due to the absence of tactile and haptic feedback [6,7,8].
Implementation of RAS depends on hospital resources and the opportunity to train in a simulated environment, without compromising patient safety [9,10,11,12,13,14]. Whether technical skills are mastered before entering the OR depends on training time and individual assessment and feedback during training [15, 16]. Currently, research seems to focus on identifying the ideal learning curve its plateau, and, moreover, on how to assess whether this stage is entered for different kind of technical skills [17, 18]. Previous studies showed that laparoscopic skills, such as efficient use of instruments and safe tissue handling, can be objectively assessed in simulation training using performance parameters [19,20,21,22]. However, little is known about the transferability of these tissue handling skills when surgeons switch between LS and RAS [23, 24].
The aim of this study is to investigate the crossover effects when switching between approaches. It was hypothesized that intermediates, in the middle of the learning curve and subject to LS simulation training, tend to focus on efficiency of movement (i.e., speed and time), rather than tissue handling parameters (i.e., force exertion), resulting in high force-parameter outcomes [22, 25,26,27,28]. Also, based on the intuitiveness attributed to RAS, it was hypothesized that switching from RAS to LS will result in increased tissue handling forces, especially in the less experienced groups.
Methods
Study design
This international, multicentre, prospective, crossover study was conducted at the Heidelberg University Hospital (Germany, Heidelberg), the Amsterdam University Medical Centers (The Netherlands, Amsterdam) and the Amsterdam Skills Centre for Health Sciences (Amsterdam, The Netherlands).
Participants
Participants were classified and divided into three groups based on their prior experience: novices consisting of junior residents (< 10 laparoscopic procedures, 0 robotic-assisted surgery procedures and no exposure to the system), intermediates consisting of senior residents and young surgeons (< 200 laparoscopic procedures, 0 robotic-assisted surgery procedures, 25 robotic knots) and experts consisting of attendees/robot experts (> 200 laparoscopic procedures, > 15 robotic-assisted surgery procedures as console surgeon, and > 50 robotic knots).
Systems and hardware
Both the da Vinci Xi Surgical System (Intuitive Surgical Inc., Sunnyvale, California USA) at the OR and a the Szabo-Berci-Sackier laparoscopic box trainer (Karl Storz, Tuttlingen, Germany) were equipped with the validated ForceSense measurement system (MediShield B.V., Delft, the Netherlands) [19, 22, 29, 30]. This system recorded raw time, 3D motion, and 3D force data from the two Trendo trocar sensors and the ForceTRAP sensor, respectively, mounted in the lid of the box trainer and bottom plate. This system recorded performance parameters that have been proven to represent efficient instrument use and tissue handling skills [19, 22]. Implementing this system facilitated objective assessment of tool-tissue interaction and instrument handling skills [29, 30]. After implementation, this system recorded the following parameters each trial: total time required to finish the task, a set of maximum and mean interaction forces and the force volume during tissue manipulation (Table 1). After each trial, the data and a video log of the performed task were stored in an online database (ForceSense.NET, MediShield, Delft, The Netherlands). The participants used two needle drivers (BBraun Aesculap, Melsungen, Germany) with a Novosyn HR26 needle and a 70 cm 3/0 thread for needle driving, suturing and knot tying. For each trial a separate surgical suture was used, equating to twelve surgical sutures for each participant.
Protocol
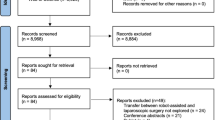
The participants were assigned in two groups, one group which started with the robotic trials (RL group novices, intermediates and experts) and one group which started with the laparoscopic trials (LR group novices, intermediates and experts). Group assignment was not fully randomized as it was influenced by the availability of the robotic and laparoscopic training systems and logistics. All trainees received a brief verbal instruction on the da Vinci Surgical System. After group assignment, each trainee performed twelve trials of a standardized minimally invasive suturing task (three-throw square knot). For the LR group, the first six trials were performed using the laparoscopic box trainer, followed by six trials using the da Vinci Surgical System (Intuitive Surgical Inc., Sunnyvale, California USA). Vice versa for the RL group (Fig. 1). Each trial of the task was measured and stored in the online database separately. The local ethics committee at Heidelberg University approved the study protocol before inclusion of the trainees.
Statistical analyses
Data were analysed using IBM SPSS statistics 26 (SPSS Inc., Chicago, Illinois USA). Descriptive statistics and frequency measurements were performed to determine the means, standard deviation and normal distribution of the data. The Shapiro–Wilk test was performed and the data were not normally distributed. GraphPad (Prism 9.0.0, San Diego, California USA) was used to visualize boxplots. Statistical comparison was done between the sixth and seventh trial to identify transition effects when subjects move from laparoscopy to robotic surgery or vice versa. Post hoc power analysis (power (1−β) of 0.80, two sided and a test significance level (α) of 0.05) was performed. An outcome with a p ≤ 0.05 was considered as statistically significant.
Results
A total of 720 trials, performed by 60 participants, were included for analyses (20 novices, 20 intermediates, 20 experts). One participant in the novice group was left dominant. There were 19 females included (6 novices, 10 intermediates, 3 expert).
Training effect
In the RL group (N = 33), novices reduced their maximum force (7.4 N vs 4.5 N, p = 0.01), maximum impulse (25.6 N/s vs 14.4 N/s, p = 0.01) and force volume (2.0 N vs 1.5 N, p = 0.01) between the first and the sixth RAS trials. The experts reduced their total completion time (110 s vs 76 s, p = 0.01) and maximum impulse (16 N/s vs 11 N/s, p = 0.05) in the RAS trials, and significantly improved all parameters in the LS trials (no. seven to twelve). A decrease in maximum forces (4.4 N to 3.1 N, p = 0.04), and maximum impulse from (16.8 to 9.8 N, p = 0.02) was observed. The intermediates had a reduced total completion time (91 s vs 80 s, p = 0.02) after the LS trials. In the LR group (N = 27), the novices (205 s vs 134 s, p = 0.01) and experts (82 s vs 44 s, p = 0.03) improved their total completion time. A detailed overview is provided in the supplemental files.
Crossover effect
Table 2 shows, that when switching from RAS to LS (trial six and seven), there was no significant change in any of the parameter outcomes, except for maximum impulse (Figs. 2, 3, 4). The expert group increased their maximum impulse with 46% (11.5 N/s to 16.8 N/s, p = 0.05) (Fig. 5). When switching from LS to RAS, the total time was increased for intermediates (68.7 s vs. 100.2 s, p = 0.05) and for experts (44.2 s vs. 84.5 s, p = 0.05). However, an significant decrease in MaxForce of 8.5% was observed in the expert group (3.9 N vs. 3.6 N, p = 0.01). The comparison of the seventh and ninth laparoscopic and robotic suturing trials, provided in Table 3, shows that the max force levels of both the intermediates and novice group start to increase after the seventh trial (Fig. 6). A 78% increase inforce exertion is was observed between the 7th and 9th trial for the intermediates (5.1 N vs. 9.1 N, p = 0.04).
Discussion
This study shows the changes in technical skill and tissue handling behaviour when switching between RAS and LS, according to objective force-based parameters. An increase in applied forces, representing decay in tissue handling skills, is observed in the less experienced groups when switching from LS to RAS. Where an increase in maximum force-parameters (Figs. 3, 6) indicates force-interaction errors, the increase in mean non zero force-parameter indicates a structural high load of the tissue during tasks that require constant traction [19, 22]. When switching from the RAS to LS, the max impulse outcomes increases (Fig. 5), indicating that the energy transmitted from the instrument to the tissue increases drastically [22]. If these parameter increases during suturing, cutting or dissecting, the risk on tissue damage or rupture also increases [31]. Moreover, excessive force application to the tissues can cause serious complications, even leading to bowel perforation and sepsis [32, 33]. An ex vivo experimental study using force measurements showed that the average acceptable force varied between 1.25 and 11.43 N, depended on the type of tissue [31]. Also, grasping forces can cause unwanted serosal thickness and histopathological changes that lead to think about force-based safety thresholds [32, 34]. These results are in line with another crossover study by Omar Hassan et al. [33], were novices had similar learning curves for RAS and LS, with limited crossover effect between approaches. Besides, like our results, this study also reported increased excessive forces in the RAS trials, compared to LS trials.
The influence of laparoscopic experience on the robotic performance has been marginally reported in previous studies. In 2018, Pimentel et al. [35], conducted a study comparing novices and experts performing tasks on a virtual reality simulator. There was no significant difference in any of the objective metrics between the differently experienced groups and there was no evidence regarding the transferability of laparoscopic skills to robotic-assisted surgery. Similarly, in 2012, Kilic et al. [36, 37] compared two groups with different experience in laparoscopy. The groups performed a knot tying task in a LS and RAS setting and the total completion time was the only objective metric. The more experienced trainees had a significant difference in the total completion time during the RAS trials. However, despite the difference in prior laparoscopic experience, this difference was not visible in the LS trials.
The present results show that intermediates and novices perform better at the end of their learning curve when starting with RAS, compared to groups that started with LS. These changes in technical skills are likely related to the difference in controls of both systems and should be considered when training skills. From human–machine interaction studies, it is observed that a change in interface requires the operator to switch from a more automated modus, to a more complex neuro control part of the brain that require more active thinking, which may cause problems with execution of the tasks [36,37,38]. The novices and experts experienced less decay of tissue handling skills (MaxForce) when switching from LS to RS, compared to intermediates. The variation in task time in trial seven to nine (Table 3), compared to trial four to six (Fig. 2), indicates that more novices and intermediates had difficulties with efficient suturing performance after changing from RAS to LS. However, when switching from LS to RAS, novices and intermediate outcomes are comparable between techniques, but expert data shows that task time increased for many surgeons. These outcomes can be explained by a lack of haptic feedback in RAS, compared to conventional LS.
Likewise LS, the adaptation of RAS and the implementation of it in hospitals is usually initiated by experienced surgeons. We know that even expert surgeons can apply significantly higher force during LS, compared to open surgery [39]. This is caused by the loss of tactile and haptic feedback. Although RAS has the advantage in accuracy and more precise handling of instruments, the sensory feedback mechanism are further diminished [6,7,8], which results in dangerously high force application on the tissues. Haptic force feedback during training has the potential to limit the applied intracorporeal forces, with a decrease up to 44% [8]. This could also potentially be explained by the fact that novices have not developed the neural network and spatiotemporal abilities, such as dealing with long instruments and the fulcrum effect, needed for safe minimally invasive surgery. Intermediates (senior residents and young surgeons) are potentially disadvantaged by the acquired laparoscopic skills during residency, while transitioning to RAS. Similar to our results, a recent study on robotic bowel anastomosis, showed lower anastomosis quality and lower Global Evaluative Assessment of Robotic Skills (GEARS) scores after laparoscopic experience, compared to only open surgery experience [40].
Shortly after the introduction of simulation training for LS, assessment forms like Objective Structured Assessment of Technical Skills (OSATS) haven been used to determine technical competency. These forms have been a reliable tool for the qualitative assessment of a procedural performance for over two decades, but are money and time consuming, as the trainees are usually assessed by senior surgeons. With rapid technological innovations, this type of procedural assessment was then followed by systems that recorded motion analysis parameters. Unfortunately, these forms and measures of time and motion efficiency (i.e., instrument handling), provide limited quantitative information on the effect that these instruments have on the tissue. GEARS might be suitable to detect improvement of basic skills over time in inexperience trainees [41, 42]. However, there is no association between laparoscopic experience and robotic-assisted suturing performance, according to OSATS scores, and there is evidence that assessment forms are not be suitable for the assessment of robotic technical skills and to differentiate between levels of expertise [43, 44]. This was confirmed by other recent studies, were novices were assessed during RAS skills training [45, 46]. The GEARS increased self-awareness, but did not influence the acquisition of technical skill among trainees, and no correlation was found between technical skill and operative performance. This shows that besides technical skills, also cognitive skills, intraoperative strategies and decision making should be trained before commencing RAS in the OR.
In contrast, during a study on robotic inguinal hernia repair, objective robot generated performance metrics have been shown to be accurate and more reliable than self-awareness or even faculty surgeons assessment [47]. This was also concluded by our previous work regarding the use of objective force-based parameters to assess technical skills during laparoscopic skills training [29, 30, 48]. Following force-based assessment tools for LS, validity evidence for objective assessment tools for RAS in accumulating [15, 16, 49,50,51,52]. A recent construct validation study by our group confirmed the potential for force-based parameters in assessment of tissue handling skills in RAS training [51]. Those results, along with the present results, underline the importance of quantitative objective force-based assessment of tissue-tool interaction and tissue manipulation skills. These parameters can now be utilized not only for personalized assessment and feedback during training, but also serve as benchmarks for group training and for proficiency-based training.
Strengths and limitations
In this multicenter study, conducted at renowned academic training centers for training in minimally invasive surgery, a large cohort with 60 participants of three different experience levels performed a standardized surgical knot tying task improving the scientific value of the results. Technical skill was assessed by the recently for RAS validated ForceSense system that, in constrast to time parameter and GEARS, can objectively assess the forces applied to the tissue [51]. Using a standardized suturing and knot tying as task adds validity to the experiments as this task is representative for the assessment and validation of laparoscopic and general surgical skill [53, 54]. Furthermore, the use of a real DaVinci system, real instruments with haptic feedback, and a realistic suturing task, simulated a setting which increased the generalizability and suggest the transferability of these outcomes to the operating room. Although it added value to the generalisability of the results, this study is limited by variability and the heterogeneity of the subgroups. If inclusion criteria were more strict, these data could also be used to identify learning curve effects between groups. As is clear from the results and from the literature review, during the interpretation of these data, one should consider in which context the data have been acquired. For example, the level of experience, the complexity of the tasks and de construct validity of the assessment tool that is used. Furthermore, no motion parameters that represent instrument handling skills were included in this study. As the DVR system of Davinci and ForceSense system use different assessment parameters. Therefore following studies should solve this issue or allow the use of robotic instruments inside the ForceSense system, by increasing its diameter.
Conclusion
The crossover effects in technical skills between laparoscopic and robot-assisted surgery are highly depended on the prior experience with laparoscopic surgery. Experts can alternate between approaches without impairment of technical skills. Less experienced surgeons showed decreased efficiency of motion when switching from robotic to laparoscopic surgery, and high tissue handling forces when switching from laparoscopic to robotic surgery. Additional simulation training is advised for these trainees to prevent from undesired events.
References
Jung M, Morel P, Buehler L, Buchs NC, Hagen ME (2015) Robotic general surgery: current practice, evidence, and perspective, Langenbeck’s. Arch Surg 400:283–292. https://doi.org/10.1007/s00423-015-1278-y
Lane T (2018) A short history of robotic surgery. Ann R Coll Surg Engl 100:5–7. https://doi.org/10.1308/rcsann.supp1.5
George EI, Brand TC, LaPorta A, Marescaux J, Satava RM (2018) Origins of robotic surgery: from skepticism to standard of care. J Soc Laparoendosc Surg. https://doi.org/10.4293/JSLS.2018.00039
Armijo PR, Huang CK, High R, Leon M, Siu KC, Oleynikov D (2019) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc 33(7):2323–2331. https://doi.org/10.1007/s00464-018-6515-3
Rodrigues Armijo P, Huang CK, Carlson T, Oleynikov D, Siu KC (2020) Ergonomics analysis for subjective and objective fatigue between laparoscopic and robotic surgical skills practice among surgeons. Surg Innov 27(1):81–87. https://doi.org/10.1177/1553350619887861
El Rassi I, El Rassi JM (2020) A review of haptic feedback in tele-operated robotic surgery. J Med Eng Technol 44(5):247–254. https://doi.org/10.1080/03091902.2020.177239
van der Meijden OA, Schijven MP (2009) The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surg Endosc 23(6):1180–1190. https://doi.org/10.1007/s00464-008-0298-x
Miller J, Braun M, Bilz J, Matich S, Neupert C, Kunert W, Kirschniak A (2021) Impact of haptic feedback on applied intracorporeal forces using a novel surgical robotic system-a randomized cross-over study with novices in an experimental setup. Surg Endosc 35(7):3554–3563. https://doi.org/10.1007/s00464-020-07818-8
Gkegkes ID, Mamais IA, Iavazzo C (2017) Robotics in general surgery: a systematic cost assessment. J Minim Access Surg 13:243–255. https://doi.org/10.4103/0972-9941.195565
Liberman D, Trinh QD, Jeldres C, Zorn KC (2012) Is robotic surgery cost-effective: yes. Curr Opin Urol 22:61–65. https://doi.org/10.1097/MOU.0b013e32834d543f
Childers CP, Maggard-Gibbons M (2018) Estimation of the acquisition and operating costs for robotic surgery. J Am Med Assoc 320:835–836. https://doi.org/10.1001/jama.2018.9219
Tedesco G, Faggiano FC, Leo E, Derrico P, Ritrovato M (2016) A comparative cost analysis of robotic-assisted surgery versus laparoscopic surgery and open surgery: the necessity of investing knowledgeably. Surg Endosc 30:5044–5051. https://doi.org/10.1007/s00464-016-4852-7
Sridhar AN, Briggs TP, Kelly JD, Nathan S (2017) Training in robotic surgery—an overview. Curr Urol Rep. https://doi.org/10.1007/s11934-017-0710-y
Brinkman W, de Angst I, Schreuder H, Schout B, Draaisma W, Verweij L, Hendrikx A, van der Poel H (2017) Current training on the basics of robotic surgery in the Netherlands: time for a multidisciplinary approach? Surg Endosc 31:281–287. https://doi.org/10.1007/s00464-016-4970-2
Kutana S, Bitner DP, Addison P, Chung PJ, Talamini MA, Filicori F (2022) Objective assessment of robotic surgical skills: review of literature and future directions. Surg Endosc 36(6):3698–3707. https://doi.org/10.1007/s00464-022-09134-9
Goldenberg MG, Lee JY, Kwong JCC, Grantcharov TP, Costello A (2018) Implementing assessments of robot-assisted technical skill in urological education: a systematic review and synthesis of the validity evidence. BJU Int 122(3):501–519. https://doi.org/10.1111/bju.14219
Kassite I, Bejan-Angoulvant T, Lardy H, Binet A (2019) A systematic review of the learning curve in robotic surgery: range and heterogeneity. Surg Endosc 33:353–365. https://doi.org/10.1007/s00464-018-6473-9
Mazzon G, Sridhar A, Busuttil G, Thompson J, Nathan S, Briggs T, Kelly J, Shaw G (2017) Learning curves for robotic surgery: a review of the recent literature. Curr Urol Rep 18:1–6. https://doi.org/10.1007/s11934-017-0738-z
Horeman T, Dankelman J, Jansen FW, Van Den Dobbelsteen JJ (2014) Assessment of laparoscopic skills based on force and motion parameters. IEEE Trans Biomed Eng 61:805–813. https://doi.org/10.1109/TBME.2013.2290052
Jones D, Jaffer A, Nodeh AA, Biyani CS, Culmer P (2018) Analysis of mechanical forces used during laparoscopic training procedures. J Endourol 32:529–533. https://doi.org/10.1089/end.2017.0894
Agha RA, Fowler AJ (2015) The role and validity of surgical simulation. Int Surg 100:350–357. https://doi.org/10.9738/INTSURG-D-14-00004.1
Horeman T, Rodrigues SP, Willem Jansen F, Dankelman J, Van Den Dobbelsteen JJ (2012) Force parameters for skills assessment in laparoscopy. IEEE Trans Haptics 5:312–322. https://doi.org/10.1109/TOH.2011.60
Kowalewski KF, Schmidt MW, Proctor T, Pohl M, Wennberg E, Karadza E, Romero P, Kenngott HG, Müller-Stich BP, Nickel F (2018) Skills in minimally invasive and open surgery show limited transferability to robotic surgery: results from a prospective study. Surg Endosc 32:1656–1667. https://doi.org/10.1007/s00464-018-6109-0
Schmidt MW, Köppinger KF, Fan C, Kowalewski KF, Schmidt LP, Vey J, Proctor T, Probst P, Bintintan VV, Müller-Stich BP, Nickel F (2021) Virtual reality simulation in robot-assisted surgery: meta-analysis of skill transfer and predictability of skill. BJS Open 5:066. https://doi.org/10.1093/bjsopen/zraa066
Sánchez R, Rodríguez O, Rosciano J, Vegas L, Bond V, Rojas A, Sanchez-Ismayel A (2016) Robotic surgery training: construct validity of Global Evaluative Assessment of Robotic Skills (GEARS). J Robot Surg 10:227–231. https://doi.org/10.1007/s11701-016-0572-1
Finnegan KT, Meraney AM, Staff I, Shichman SJ (2012) Laparoscopy and robotics da Vinci skills simulator construct validation study: correlation of prior robotic experience with overall score and time score simulator performance. Urology. https://doi.org/10.1016/j.urology.2012.02.059
Panait L, Shetty S, Shewokis PA, Sanchez JA (2014) Do laparoscopic skills transfer to robotic surgery? J Surg Res 187:53–58. https://doi.org/10.1016/j.jss.2013.10.014
Thomaier L, Orlando M, Abernethy M, Paka C, Chen CCG (2017) Laparoscopic and robotic skills are transferable in a simulation setting: a randomized controlled trial. Surg Endosc 31:3279–3285. https://doi.org/10.1007/s00464-016-5359-y
Hardon SF, Horeman T, Bonjer HJ, Meijerink WJHJ (2018) Force-based learning curve tracking in fundamental laparoscopic skills training. Surg Endosc 32:3609–3621. https://doi.org/10.1007/s00464-018-6090-7
Hardon SF, van Gastel LA, Horeman T, Daams F (2021) Assessment of technical skills based on learning curve analyses in laparoscopic surgery training. Surgery 170(3):831–840. https://doi.org/10.1016/j.surg.2021.04.024
Hassan SO, Dudhia J, Syed LH, Patel K, Farshidpour M, Cunningham SC, Kowdley GC (2015) Conventional laparoscopic vs robotic training: which is better for naive users? A randomized prospective crossover study. J Surg Educ 72(4):592–599. https://doi.org/10.1016/j.jsurg.2014.12.008
Khan AF, MacDonald MK, Streutker C, Rowsell C, Drake J, Grantcharov T (2021) Tissue stress from laparoscopic grasper use and bowel injury in humans: establishing intraoperative force boundaries. BMJ Surg Interv Health Technol 3(1):e000084. https://doi.org/10.1136/bmjsit-2021-000084
Rodrigues SP, Horeman T, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2012) Suturing intraabdominal organs: when do we cause tissue damage? Surg Endosc 26(4):1005–1009. https://doi.org/10.1007/s00464-011-1986-5
Khan AF, Macdonald MK, Streutker C, Rowsell C, Drake J, Grantcharov T (2019) Defining the relationship between compressive stress and tissue trauma during laparoscopic surgery using human large intestine. IEEE J Transl Eng Health Med 7:3300108. https://doi.org/10.1109/JTEHM.2019.2919029
Pimentel M, Cabral RD, Costa MM, Neto BS, Cavazzola LT (2018) Does previous laparoscopic experience influence basic robotic surgical skills? J Surg Educ 75:1075–1081. https://doi.org/10.1016/j.jsurg.2017.11.005
Kilic GS, Walsh TM, Borahay M, Zeybek B, Wen M, Breitkopf D (2012) Effect of residents’ previous laparoscopic surgery experience on initial robotic suturing experience. ISRN Obstet Gynecol 2012:1–4. https://doi.org/10.5402/2012/569456
Rasmussen J (1982) Human errors—a taxonomy for describing human malfunction in industrial installations. J Occup Accid 4(2–4):311–333. https://doi.org/10.1016/0376-6349(82)90041-4
Friedrich M, Vollrath M (2021) Human-machine interface design for monitoring safety risks associated with operating small unmanned aircraft systems in urban areas. Aerospace 8(3):71. https://doi.org/10.3390/aerospace8030071
Rodrigues SP, Horeman T, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2015) Tying different knots: what forces do we use? Surg Endosc 29(7):1982–1989. https://doi.org/10.1007/s00464-014-3898-7
Sundelin MO, Paltved C, Kingo PS, Kjölhede H, Jensen JB (2022) The transferability of laparoscopic and open surgical skills to robotic surgery. Adv Simul 7(1):26. https://doi.org/10.1186/s41077-022-00223-2
Gerull W, Zihni A, Awad M (2020) Operative performance outcomes of a simulator-based robotic surgical skills curriculum. Surg Endosc 34(10):4543–4548. https://doi.org/10.1007/s00464-019-07243-6
Laca JA, Kocielnik R, Nguyen JH, You J, Tsang R, Wong EY, Shtulman A, Anandkumar A, Hung AJ (2022) Using real-time feedback to improve surgical performance on a robotic tissue dissection task. Eur Urol Open Sci 46:15–21. https://doi.org/10.1016/j.euros.2022.09.015
Møller SG, Dohrn N, Brisling SK, Larsen JCR, Klein M (2020) Laparoscopic versus robotic-assisted suturing performance among novice surgeons: a blinded, cross-over study. Surg Laparosc Endosc Percutaneous Techn 30(2):117–122. https://doi.org/10.1097/SLE.0000000000000766
Bitner DP, Kutana S, Carsky K, Addison P, DeChario SP, Antonacci A, Mikhail D, Yatco E, Chung PJ, Filicori F (2023) The surgical learning curve: does robotic technical skill explain differences in operative performance? J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2022.0439
Mills JT, Hougen HY, Bitner D, Krupski TL, Schenkman NS (2017) Does robotic surgical simulator performance correlate with surgical skill? J Surg Educ 74(6):1052–1056. https://doi.org/10.1016/j.jsurg.2017.05.011
Brown JD, Kuchenbecker KJ (2023) Effects of automated skill assessment on robotic surgery training. Int J Med Robot Comput Assist Surg 19(2):e2492. https://doi.org/10.1002/rcs.2492
Quinn KM, Chen X, Runge LT, Pieper H, Renton D, Meara M, Collins C, Griffiths C, Husain S (2022) The robot doesn’t lie: real-life validation of robotic performance metrics. Surg Endosc. https://doi.org/10.1007/s00464-022-09707-8
Rahimi AM, Hardon SF, Uluç E, Bonjer HJ, Daams F (2023) Prediction of laparoscopic skills: objective learning curve analysis. Surg Endosc 37(1):282–289. https://doi.org/10.1007/s00464-022-09473-7
Hardon SF, Kooijmans A, Horeman R, van der Elst M, Bloemendaal ALA, Horeman T (2022) Validation of the portable virtual reality training system for robotic surgery (PoLaRS): a randomized controlled trial. Surg Endosc 36(7):5282–5292. https://doi.org/10.1007/s00464-021-08906-z
Willuth E, Hardon SF, Lang F, Haney CM, Felinska EA, Kowalewski KF, Müller-Stich BP, Horeman T, Nickel F (2022) Robotic-assisted cholecystectomy is superior to laparoscopic cholecystectomy in the initial training for surgical novices in an ex vivo porcine model: a randomized crossover study. Surg Endosc 36(2):1064–1079. https://doi.org/10.1007/s00464-021-08373-6
Rahimi AM, Hardon SF, Willuth E, Lang F, Haney CM, Felinska EA, Kowalewski KF, Müller-Stich BP, Horeman T, Nickel F, Daams F (2023) Force-based assessment of tissue handling skills in simulation training for robot-assisted surgery. Surg Endosc. https://doi.org/10.1007/s00464-023-09905-y
Turbati MS, Goldblatt MI, Gould JC, Higgins RM (2023) Robotic simulation: validation and qualitative assessment of a general surgery resident training curriculum. Surg Endosc 37(3):2304–2315. https://doi.org/10.1007/s00464-022-09558-3
Emken JL, Mcdougall EM, Clayman RV (2004) Training and assessment of laparoscopic skills. J Soc Laparoendosc Surg 8:195–199
Mori T, Hatano N, Maruyama S, Atomi Y (1998) Significance of “hands-on training” in laparoscopic surgery. Surg Endosc 12:256–260. https://doi.org/10.1007/s004649900646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Tim Horeman is founder and shareholder of the TU-Delft MedTech startup Medishield Delft BV. Felix Nickel reports receiving travel support and support for training courses by Johnson and Johnson, Medtronic, Intuitive Surgical, Cambridge Medical Robotics, and Karl Storz as well as consultancy fees by Karl Storz. Sem F. Hardon, E. Willuth, A. Masie Rahimi, F. Lang, Caelan M. Haney, Eleni A. Felinska, Karl-Friedrich Kowalewski, Beat P. Müller-Stich, Donald L. van der Peet, Freek Daams, F. Nickel and Tim Horeman report no financial ties or conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hardon, S.F., Willuth, E., Rahimi, A.M. et al. Crossover-effects in technical skills between laparoscopy and robot-assisted surgery. Surg Endosc 37, 6015–6024 (2023). https://doi.org/10.1007/s00464-023-10045-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10045-6