Abstract
Background
Minimally invasive techniques have increasingly been adopted for liver resection. This study aimed to compare the perioperative outcomes of robot-assisted liver resection (RALR) with laparoscopic liver resection (LLR) for liver cavernous hemangioma and to evaluate the treatment feasibility and safety.
Methods
A retrospective study of prospectively collected data was conducted on consecutive patients who underwent RALR (n = 43) and LLR (n = 244) for liver cavernous hemangioma between February 2015 and June 2021 at our institution. Patient demographics, tumor characteristics, and intraoperative and postoperative outcomes were analyzed and compared using propensity score matching.
Results
The postoperative hospital stay was significantly shorter (P = 0.016) in the RALR group. There were no significant differences between the two groups in overall operative time, intraoperative blood loss, blood transfusion rates, conversion to open surgery or complication rates. There was no perioperative mortality. Multivariate analysis showed that hemangiomas located in posterosuperior liver segments and those in close proximity to major vascular structures were independent predictors of increased intraoperative blood loss (P = 0.013 and P = 0.001, respectively). For patients with hemangioma in close proximity to major vascular structures, there were no significant differences in perioperative outcomes between the two groups, with the exception that intraoperative blood loss in the RALR group was significantly less than that in the LLR group (350 ml vs. 450 ml, P = 0.044).
Conclusions
Both RALR and LLR were safe and feasible for treating liver hemangioma in well-selected patients. For patients with liver hemangioma in close proximity to major vascular structures, RALR was better than conventional laparoscopic surgery in reducing intraoperative blood loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Liver cavernous hemangioma is the most common benign liver lesion with an estimated prevalence of 5–20% [1]. These lesions occur most frequently in adult women, and are usually detected between the third and fifth decades of life [2]. Liver hemangioma is usually asymptomatic, and is incidentally diagnosed on imaging studies. Once diagnosed, the majority of these lesions do not require any clinical intervention. Observation of asymptomatic lesions using routine follow-up and imaging is usually adequate [3, 4].
Surgical resection is the only curative treatment. Indications for surgery include the presence of progressive symptoms, spontaneous or traumatic rupture, rapidly enlarging lesions, Kasabach–Merritt syndrome and an unclear diagnosis [5]. Traditional open liver resection for hemangioma requires a long subcostal incision followed by a long postoperative recovery and a high complication rate [6, 7]. Moreover, massive intraoperative hemorrhage remains a major challenge during liver resection or enucleation for hemangiomas [8,9,10].
Minimally invasive surgery has currently been widely adopted by liver surgeons to treat benign and malignant liver lesions. When compared to open liver resection, minimally invasive resection offers many advantages including decreased intraoperative blood loss, minimized postoperative pain, lower overall morbidity, shorter hospital stay and quicker recovery [11, 12]. In past decades, laparoscopic hepatectomy has gradually been accepted to be safe and feasible, and in selected patients, it is a preferable treatment over open liver resection [13]. However, several inherent limitations have hindered its wide acceptance by liver surgeons, including the limited degree of motion of laparoscopic instruments, the two-dimensional visual field, tremor amplification and poor ergonomics [14]. The introduction of surgical robot has overcome many of the shortcomings of traditional laparoscopic surgery [15] by providing high definition three-dimensional visualization, EndoWrist instruments with 7 degrees of freedom of motion, and tremor filtration. Cohort studies on robot-assisted and/or laparoscopic liver resection for hemangioma have been reported, but most of these studies are small case series or case reports [16,17,18,19,20]. To our knowledge, there have been no studies directly comparing robot-assisted liver resection (RALR) versus laparoscopic liver resection (LLR) for liver hemangiomas.
In this single-center retrospective study, perioperative outcomes of RALR were compared with those of LLR to determine whether robot-assisted surgery was superior to traditional laparoscopic surgery for liver hemangiomas.
Methods
Patients
Consecutive patients who underwent minimally invasive liver resection for liver hemangioma at the Hepatic Surgery Center, Tongji Hospital of Huazhong University of Science and Technology, Wuhan, China from February 2015 to June 2021 were included in this study. Based on the minimally invasive surgical technique used, patients were divided into the robot-assisted liver resection group (RALR) and the laparoscopic liver resection group (LLR). The indications for surgery included the presence of progressive abdominal symptoms related to hemangiomas such as upper abdominal discomfort or pain, rapid growth in size and uncertainty of malignancy. Patient information retrieved from the electronic medical records included: patient demographics, preoperative laboratory tests, characteristics of the liver hemangioma, surgery-related variables, postoperative complications, mortality and postsurgical hospital stay. This study was approved by the Institutional Review Board of the hospital and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki.
Preoperative evaluation
Preoperative evaluation consisted of a routine panel of blood tests, ultrasonography and contrast-enhanced computed tomography (CT). Magnetic resonance imaging (MRI) was performed if the diagnosis was unclear. For giant hemangiomas adjacent to major vascular structures, three-dimensional reconstruction of the liver vasculature was undertaken. Decisions on surgical treatment for liver hemangioma were made in multidisciplinary meetings attended by liver surgeons, sonographers, radiologists, oncologists, gastroenterologists, and pathologists. The choice between robotic-assisted and laparoscopic techniques was made by the patient and the surgeon. Informed consent was obtained from all patients for the operation and for the data to be used in clinical research.
Surgical techniques
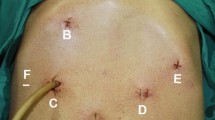
The robotic-assisted and laparoscopic liver resection techniques used at our institution have been described in previous reports [21, 22]. All procedures were performed by experienced hepatobiliary surgeons who had passed through the learning curves of RALR and LLR. Briefly, the patient was placed in a reversed Trendelenburg position. The semileft lateral decubitus position was employed when the hemangioma was located in the right posterior section or liver segments 6, 7 and 8. The da Vinci S Surgical System (Intuitive Surgical Inc., Sunnyvale, CA) was used for robot-assisted procedures. Five trocars were used: a 12-mm camera port, 2 or 3 working 8-mm robotic ports, and 1 or 2 assistant ports for intraoperative ultrasound, suction, operative instruments and endovascular staplers. The robotic cart was docked at the patient’s head. For laparoscopic surgery, 5 ports (5–12 mm) were placed according to the location of the hemangioma, with trocars distributed around the lesion in a fan-shaped pattern. CO2 pneumoperitoneum was established and maintained at 12–14 mmHg. Intraoperative ultrasound (Aloka, Inc., Tokyo, Japan) was routinely performed to identify the relationship between the liver hemangioma and the major blood vessels.
The feeding artery to the liver hemangioma was identified early and controlled with a bull-dog clamp. A urinary catheter was used to encircle the liver pedicle to perform Pringle’s maneuver before liver parenchymal transection. Central venous pressure was controlled below 5 mmHg during liver parenchymal transection. Enucleation was carried out using the technique described previously [23]. For laparoscopic liver resection or enucleation, parenchymal transection was performed by using a harmonic scalpel (Ethicon, Cincinnati, OH, USA). For robot-assisted procedures, a harmonic scalpel was used for transections along straight planes, while the Kelly clamp crushing technique using the endowristed Maryland bipolar forceps (Intuitive Surgical, Sunnyvale, CA, USA) was used for hemangiomas in close proximity to major vascular structures that required a curved transection plane. Divided small diameter vessels were bipolar electrocoagulated, while larger vessels and bile ducts were transected after clamping with Hem-o-loks (Weck Surgical Instruments, Teleflex Medical, Durham, NC, USA) or with Endoscopic Rotating Multiple Clips (Ethicon Endo-Surgery). Laparoscopic linear staplers (EndoGIA, Ethicon Endo-Surgery, Cincinnati, OH, USA) were used to transect the major vascular structures.
After the liver hemangioma was resected, any residual bleeding sites were controlled with suture ligation or electrocautery. The raw surface of the liver was checked for bile leaks. The specimen was inserted into a plastic bag and extracted through a suprapubic transverse incision. A silicone drain was applied to the raw liver transection plane.
Definitions
The types of hepatectomy were defined according to the Brisbane 2000 terminology [24]. Major hepatectomy was defined as resection of three or more Couinaud liver segments, while minor hepatectomy was defined as resection of fewer than 3 segments [25]. Enucleation was defined as removal of a hemangioma without any loss of adjacent normal hepatic parenchyma. Segments 1, 4a, 7, and 8 were defined as posterosuperior (PS) segments, whereas segments 2, 3, 4b, 5, and 6 were defined as anterolateral segments. Close proximity to major vascular structures was defined as proximity to the porta hepatis, major hepatic veins, or inferior vena cava (IVC). The severity of postoperative complications was graded according to the Clavien‒Dindo classification [26]. Postoperative liver failure and bile leakage were defined according to the International Study Group of Liver Surgery (ISGLS) criteria [27, 28]. Postoperative mortality was defined as death within 90 days of surgery.
Statistical analysis
Continuous variables are expressed as the median (range). Categorical variables are expressed as numbers with percentages. Statistical analysis was performed using Student’s t test for continuous variables and the chi-squared or Fisher exact test for categorical variables. The Mann–Whitney U test was used for nonparametric variables. Multivariate logistic regression analyses were performed to identify independent variables associated with increased blood loss. The cutoff level of blood loss was set at the predictive value for red cell transfusion using receiver operating characteristics (ROC) analysis. To reduce confounding effects from heterogeneities between the two groups, propensity score matching (PSM) was performed using a 1:2 ratio based on the nearest neighbor matching method without replacement. Independent variables entered into the propensity model included age, sex, BMI, history of previous upper abdominal operation, size of the largest lesion, the lesion location and its relationship with major blood vessels. Differences were considered significant at P values of < 0.05. Statistical analyses were performed using SPSS 22.0 software for Windows.
Results
Patient and hemangioma characteristics
During the study period, 287 patients with liver hemangiomas underwent minimally invasive liver resection. There were 43 RALR and 244 LLR. The demographics and preoperative characteristics of the patients are summarized in Table 1. There were 196 female and 91 male patients, with a median age of 48 years (range, 24–66). Fifty-six of the 287 patients were asymptomatic. The most common symptoms were upper abdominal discomfort (n = 76), right or left quadrant abdominal pain (n = 79) and abdominal mass (n = 1). The other important indication for surgery was rapid growth (n = 75). The median hemangioma size was 8.6 (range, 5–25) cm. One hundred ninety-two (66.9%) patients had a single hemangioma and 95 (33.1%) patients had multiple hemangiomas. The lesions were located in the right hemilivers in 88 (30.7%) patients, left hemilivers in 170 (59.2%) patients and bilateral hemilivers in 29 (10.1%) patients. Eighty-seven patients had their hemangiomas in the posterosuperior segments, whereas 200 patients had hemangiomas in the anteroperipheral segments. In 107 patients, the liver hemangioma was in close proximity to the major hepatic veins or the inferior vena cava, and in 23 patients, it was in proximity to the porta hepatis.
Perioperative outcomes
There were no significant differences in the patient demographics and preoperative characteristics between the RALR and LLR groups, except that the RALR group had significantly higher proportions of solitary lesion (P = 0.028) and lesions in close proximity to major vascular structures (P = 0.016) than the laparoscopic group (Table 1). After propensity score matching, these imbalances between groups were eliminated.
The data about the surgical procedures, and intraoperative and postoperative outcomes are outlined in Table 2. There were no significant differences between the two groups in the extent or types of liver resection, blood transfusion rates and postoperative laboratory results. The operative time was significantly longer in the RALR group (270 min versus 210 min; P = 0.002), whereas the median blood loss was comparable between groups (200 mL versus 200 mL; P = 0.579). In the propensity-matched cohorts, there were no significant differences in inflow occlusion time, blood loss, blood transfusion rates or postoperative laboratory results between groups. There was a trend toward a longer operative time in RALR than LLR (270 min vs. 240 min, P = 0.062).
Of the 43 patients in the RALR group, only 2 (4.7%) required conversion to open surgery. Although the conversion rate in the LLR group was higher, the difference did not reach significance (8.6% vs. 4.7%, P = 0.564). The reasons for conversion to open surgery included intraoperative bleeding in 19 patients, severe adhesions in 3 patients, and hemodynamic instability after Pringle’s maneuver in 1 patient. After propensity score matching, the conversion rate in LLR was still higher, but it again failed to reach a significant difference (10.5% vs. 4.7%, P = 0.265).
The complication rate was 11.6% (5 of 43 patients) in the RALR group, and 18.9% (46 of 244 patients) in the LLR group (P = 0.253). All 5 complications in the RALR group were grade I. Four patients (1.6%) in the LLR group developed grade III complications. The most common complication was pleural effusion, which occurred in 4 (9.3%) patients in the RALR group and 37(15.2%) patients in the LLR group. There was no perioperative mortality in either group. The postoperative hospital stay was significantly shorter in the RALR group than in the LLR group (P = 0.035). After propensity score matching, the complication rates showed no significant difference between groups (11.6% in RALR vs. 23.3% in LLR, P = 0.115). Patients who underwent RALR had a significantly shorter postsurgical hospital stay than patients who underwent LLR (P = 0.016).
Factors associated with increased intraoperative blood loss
The mean and median blood losses were 324.5 mL and 200 (range, 200–2500) mL, respectively. ROC analysis showed that the predictive value of blood loss in patients who received red cell transfusion was 550 ml. On univariate analysis, increased blood loss was significantly correlated with hemangiomas located in posterosuperior segments, in close proximity to major vascular structures, lesions > 10 cm, lesions in right/bilateral hemilivers, major liver resection, Pringle’s maneuver, conversion to open surgery, complication rate, operation time and postoperative hospital stay (Table 3). On multivariate analysis, hemangiomas located in posterosuperior segments and in close proximity to major vascular structures were independent predictors of increased intraoperative blood loss (P = 0.013 and P = 0.001, respectively; Table 4).
RALR versus LLR for patients with hemangioma in close proximity to major vascular structures
For patients with hemangioma in close proximity to major vascular structures, the RALR and LLR groups were comparable in patient demographics and hemangioma characteristics. There were no significant differences in operative time, Pringle’s maneuver, conversion rate, complication rate or postoperative hospital stay. The intraoperative blood loss in the RALR group was significantly less than that in the LLR group (350 ml vs. 500 ml, P = 0.018) with significantly fewer patients requiring blood transfusion in the RALR group (11.1% vs. 30.1%, P = 0.046).
After propensity score matching, the two groups showed no significant difference in baseline characteristics. No significant differences were observed in Pringle’s maneuver, blood transfusion, conversion rate, complication rate or postoperative hospital stay between groups. Although the RALR group required a longer operative time (330 min vs. 300 min), the difference did not reach significance (P = 0.06). Compared to the LLR group, the RALR group had significantly less intraoperative blood loss (350 ml vs. 450 ml, P = 0.044) (Table 5).
Discussion
Cavernous hemangioma represents the most common benign lesion of the liver [1]. Most hemangiomas do not require any treatment, as the natural history of liver hemangioma is generally uncomplicated. Surgery should only be considered for patients with complicated or symptomatic lesions, or when malignancy cannot be excluded [5, 7]. Surgical treatment is the only effective treatment for liver hemangiomas. Although minimally invasive liver resection has been increasingly adopted for many benign or malignant liver lesions [29], there has been no consensus on whether RALR can provide better treatment outcomes than conventional LLR.
Shin et al. [30] reported that laparoscopic liver resection for liver hemangioma produced better perioperative outcomes than open surgery. A recently reported study using PSM analysis showed similar findings [31]. However, other studies revealed no significant differences in operative time, estimated blood loss, or major morbidity and mortality rates between laparoscopic and open surgery [32, 33]. A small study comparing the perioperative outcomes of robot-assisted, laparoscopic and open hemihepatectomy for giant hemangiomas over 10 cm [34] showed robotic hemihepatectomy to be associated with significantly less intraoperative blood loss and a shorter operative time and postoperative hospital stay than laparoscopic surgery.
The results of our study showed that both robot-assisted and laparoscopic liver resection were feasible, safe and effective in treating large to giant hemangiomas. There were no significant differences in blood loss, conversion or postoperative overall morbidity rates between RALR and LLR. However, RALR had a longer operative time but a shorter postsurgical hospital stay. These findings are consistent with the results obtained in a previous study and a recent meta-analyses [35, 36]. As robot-assisted liver resection has only recently been adopted by liver surgeons, the learning curve can be an important factor contributing to the differences in operation time reported by different surgeons. Tsung et al. [37] showed the operation time was significantly decreased as experience with robotic technology accumulated. Furthermore, in robotic surgery, extra time is required for changing instruments, and docking and undocking the robotic system as stated by the International Consensus Statement on robotic hepatectomy in 2018 [12].
Liver hemangioma is a benign disease. Enucleation is the preferred surgical treatment as it avoids unnecessary loss of healthy liver parenchyma [38,39,40]. The identification of a plane between the pseudocapsule of a hemangioma and liver parenchyma is the most challenging part of the procedure. Delicate detachment of the lesion from the pseudocapsule carries a risk of bleeding, especially when the hemangioma is adjacent to major vascular structures. Our study showed robotic surgery to have a significant advantage in reducing intraoperative blood loss over traditional laparoscopic surgery for patients with hemangioma in close proximity to major vascular structures. Possible reasons include the following: First, the robotic surgery system provides a stable and three-dimensional view with magnification of the field of operation. The high-quality images allow surgeons to detect the plane between the hemangioma and normal liver parenchyma and to identify the blood vessels supplying the hemangioma more easily. Second, the robotic surgery system is particularly applicable to liver parenchymal transection through a curved parenchymal plane. The combination of the EndoWristed Maryland bipolar forceps and a harmonic scalpel facilitates enucleation of liver hemangioma. Third, the EndoWristed technology with seven degrees of freedom allows rapid and precise suturing of vascular branches coming from the major vascular structures to the hemangioma.
When hepatic hemangiomas are located in posterosuperior liver segments, the difficulty and risks of surgery increase exponentially [41]. With the accumulation of experience, improvements in surgical skills and the development of new instruments, resection of posterosuperior segments using minimally invasive techniques has been shown currently to be feasible and safe [42, 43]. Whether robotic surgery used in the resection of posterosuperior segments can provide better perioperative outcomes than LLR is still controversial [44,45,46,47].
Surgical treatment for large liver hemangiomas carries a significant risk of massive intraoperative bleeding. The Memorial Sloan Kettering Cancer Center reported 52 patients who underwent open liver resection or enucleation for giant liver hemangioma of > 10 cm. Ten (19.2%) patients experienced blood loss of ≥ 1 L, and the median blood loss was 400 mL (range 17–10,000 mL) [8]. In our study, 116 (40.4%) patients had a giant liver hemangioma greater than 10 cm in diameter. The median blood loss was only 200 ml (range 50–2500 mL), which was significantly lower than that reported for open liver resection [38, 48, 49]. Our results also showed that the size, location, and the relationship of liver hemangiomas to major blood vessels were associated with intraoperative blood loss. These results are consistent with the results reported by other authors [50, 51].
A recent systematic review on robotic liver resections that included 31 studies and 1148 patients showed the overall complication and conversion rates to be 17.6% and 5.9% respectively [52]. Our study showed a nonsignificant difference in the overall postoperative complication rates between the robotic and laparoscopic groups (11.6% vs. 23.3%). However, all the Clavien‒Dindo grade II and III complications occurred in the laparoscopic group, a result possibly related to the increased surgical precision of using the robot which also shortened the postoperative hospital stay. In a retrospective analysis of the 2016–2018 Nationwide Readmissions Database by Aziz et al. [53], the robotic group showed a significantly lower complication rate than the laparoscopic or open group. A recent meta-analysis comparing robotic versus laparoscopic hepatectomy for HCC demonstrated that the rate of major complications was significantly lower in RALR than in LLR [54].
The rate of conversion to open surgery has been used as an indicator of technical feasibility [55]. Stiles et al. [55] reported a conversion rate of 19.1% for 1062 minimally invasive hepatectomies that were entered into the ACS‐NSQIP database from 2014 to 2015. This high conversion rate is probably attributed to the inclusion of inexperienced and small‐volume centers. The low conversion rate of 8% in our study was mainly related to all of the operations being performed by hepatobiliary surgeons with substantial experience in minimally invasive surgery working in a high-volume liver center. Our results showed that RALR had a tendency for a lower conversion rate than LLR (4.7% vs. 10.5%). Although no significant differences in the conversion rates have been reported between RALR and LLR [37, 56], a recent systematic review and two international multicenter retrospective analyses showed a significant reduction of conversion in RALR when compared with LLR [57,58,59]. Similar results were also reported by Fagenson et al. by using the NSQIP database [60].
There are several limitations of the study. First, this is a single-center retrospective comparative study with its inherent defects. The PSM method was employed to reduce any potential biases that may exist between the two groups. Second, perioperative outcomes are primarily dependent on the experience of the operating surgeons. To reduce this confounding factor, the operations in this study were performed by several surgeons who were experienced in open, robotic and laparoscopic hepatectomies. Third, there was a small sample size on patients who underwent RALR, thus lowering the statistical power. The potential type 2 errors due to the small sample size could not be obviated. However, to our knowledge, this study is the largest study directly comparing laparoscopic with robotic liver resection for hemangiomas ever reported in the medical literature. In the future, well-designed multicenter randomized studies comparing RALR with LLR for liver hemangioma are warranted.
In conclusion, this study showed that both RALR and LLR were safe and feasible in well-selected patients. RALR resulted in a longer operative time but a shorter postsurgical hospital stay. There were no significant differences in blood loss, conversion rate or postoperative overall morbidity rates between the two techniques. Hemangiomas located in posterosuperior liver segments and in close proximity to major vascular structures were independent predictors of increased intraoperative blood loss. For patients with liver hemangioma in close proximity to major vascular structures, robotic-assisted liver resection was better than laparoscopic liver resection.
References
Reddy KR, Kligerman S, Levi J, Livingstone A, Molina E, Franceschi D, Badalamenti S, Jeffers L, Tzakis A, Schiff ER (2001) Benign and solid tumors of the liver: relationship to sex, age, size of tumors, and outcome. Am Surg 67:173–178
Mergo PJ, Ros PR (1998) Benign lesions of the liver. Radiol Clin North Am 36:319–331
Okano H, Shiraki K, Inoue H, Ito T, Yamanaka T, Deguchi M, Sugimoto K, Sakai T, Ohmori S, Murata K, Takase K, Nakano T (2001) Natural course of cavernous hepatic hemangioma. Oncol Rep 8:411–414
Pietrabissa A, Giulianotti P, Campatelli A, Di Candio G, Farina F, Signori S, Mosca F (1996) Management and follow-up of 78 giant haemangiomas of the liver. Br J Surg 83:915–918
Pulvirenti E, Toro A, Di Carlo I (2010) An update on indications for treatment of solid hepatic neoplasms in noncirrhotic liver. Future Oncol 6:1243–1250
Lerner SM, Hiatt JR, Salamandra J, Chen PW, Farmer DG, Ghobrial RM, Busuttil RW (2004) Giant cavernous liver hemangiomas: effect of operative approach on outcome. Arch Surg 139:818–821
Farges O, Daradkeh S, Bismuth H (1995) Cavernous hemangiomas of the liver: are there any indications for resection? World J Surg 19:19–24
Yoon SS, Charny CK, Fong Y, Jarnagin WR, Schwartz LH, Blumgart LH, DeMatteo RP (2003) Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg 197:392–402
Giuliante F, Ardito F, Vellone M, Giordano M, Ranucci G, Piccoli M, Giovannini I, Chiarla C, Nuzzo G (2011) Reappraisal of surgical indications and approach for liver hemangioma: single-center experience on 74 patients. Am J Surg 201:741–748
Zhang W, Huang ZY, Ke CS, Wu C, Zhang ZW, Zhang BX, Chen YF, Zhang WG, Zhu P, Chen XP (2015) Surgical treatment of giant liver hemangioma larger than 10 cm: a single center’s experience with 86 patients. Medicine (Baltimore) 94:e1420
Gavriilidis P, Roberts KJ, Aldrighetti L, Sutcliffe RP (2020) A comparison between robotic, laparoscopic and open hepatectomy: a systematic review and network meta-analysis. Eur J Surg Oncol 46:1214–1224
Liu R, Wakabayashi G, Kim HJ, Choi GH, Yiengpruksawan A, Fong Y, He J, Boggi U, Troisi RI, Efanov M, Azoulay D, Panaro F, Pessaux P, Wang XY, Zhu JY, Zhang SG, Sun CD, Wu Z, Tao KS, Yang KH, Fan J, Chen XP (2019) International consensus statement on robotic hepatectomy surgery in 2018. World J Gastroenterol 25:1432–1444
Schmelzle M, Krenzien F, Schöning W, Pratschke J (2020) Laparoscopic liver resection: indications, limitations, and economic aspects. Langenbecks Arch Surg 405:725–735
Kitisin K, Packiam V, Bartlett DL, Tsung A (2011) A current update on the evolution of robotic liver surgery. Minerva Chir 66:281–293
Muaddi H, Hafid ME, Choi WJ, Lillie E, de Mestral C, Nathens A, Stukel TA, Karanicolas PJ (2021) Clinical outcomes of robotic surgery compared to conventional surgical approaches (laparoscopic or open): a systematic overview of reviews. Ann Surg 273:467–473
Okumura Y, Noda T, Eguchi H, Hanaki T, Iwagami Y, Akita H, Asaoka T, Gotoh K, Kobayashi S, Umeshita K, Mori M, Doki Y (2019) Pure laparoscopic liver resection for giant liver hemangioma with extrahepatic growth based on preoperative 3-dimensional simulation: a case report. Surg Case Rep 5:51
Kim IS, Kwon CH (2014) Feasibility of laparoscopic liver resection for giant hemangioma of greater than 6 cm in diameter. Korean J Hepatobiliary Pancreat Surg 18:118–121
Veerankutty FH, Rather SA, Yeldho V, Zacharia BM, Tu SA, Venugopal B (2019) Totally laparoscopic resection of an extremely giant hepatic hemangioma. Surg J (N Y) 5:e110–e112
Giulianotti PC, Addeo P, Bianco FM (2011) Robotic right hepatectomy for giant hemangioma in a Jehovah’s witness. J Hepatobiliary Pancreat Sci 18:112–118
Giulianotti PC, Bustos R, Valle V, Aguiluz G, Pavelko Y, Fernandes E (2019) Robot-assisted enucleation of gigantic liver hemangiomas: case series of 3 patients. Int J Surg Case Rep 60:244–248
Zhu P, Liao W, Ding ZY, Chen L, Zhang WG, Zhang BX, Chen XP (2019) Learning curve in robot-assisted laparoscopic liver resection. J Gastrointest Surg 23:1778–1787
Zhang W, Wang J, Li C, Zhang Z, Dirie NI, Dong H, Xiang S, Zhang W, Zhang Z, Zhang B, Chen X (2017) Infrahepatic inferior vena cava clamping with pringle maneuvers for laparoscopic extracapsular enucleation of giant liver hemangiomas. Surg Endosc 31:3628–3636
Baer HU, Dennison AR, Mouton W, Stain SC, Zimmermann A, Blumgart LH (1992) Enucleation of giant hemangiomas of the liver. Technical and pathologic aspects of a neglected procedure. Ann Surg 216:673–676
The Terminology Committee of the IHPBA (2000) The Brisbane 2000 terminology of hepatic anatomy and resections. HPB 2:333–339
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the international study group of liver surgery. Surgery 149:680–688
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Büchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the international study group of liver surgery (ISGLS). Surgery 149:713–724
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250:831–841
Shin Y, Rhu J, Choi GS, Kim JM, Joh JW, Kwon CHD (2020) Feasibility of laparoscopic liver resection for liver cavernous hemangioma: a single-institutional comparative study. Ann Hepatobiliary Pancreat Surg 24:137–143
Liu Q, Liu F, Ding J, Wei Y, Li B (2019) Surgical outcomes and quality of life between laparoscopic and open approach for hepatic hemangioma: a propensity score matching analysis. Medicine (Baltimore) 98:14485
Xie QS, Chen ZX, Zhao YJ, Gu H, Geng XP, Liu FB (2021) Outcomes of surgery for giant hepatic hemangioma. BMC Surg 21(1):186
Yu HB, Dong YD, Wang LC, Tian GJ, Mu SM, Cao Y, Peng YN, Lou CY, Liu P, Li DY (2015) Laparoscopic versus open resection for liver cavernous hemangioma: a single center of 2-year experience. Surg Laparosc Endosc Percutaneous Tech 25:e145-147
Hu M, Chen K, Zhang X, Li C, Song D, Liu R (2020) Robotic, laparoscopic or open hemihepatectomy for giant liver haemangiomas over 10 cm in diameter. BMC Surg 20:93
Montalti R, Berardi G, Patriti A, Vivarelli M, Troisi RI (2015) Outcomes of robotic vs laparoscopic hepatectomy: a systematic review and meta-analysis. World J Gastroenterol 21:8441–8451
Hu Y, Guo K, Xu J, Xia T, Wang T, Liu N, Fu Y (2021) Robotic versus laparoscopic hepatectomy for malignancy: a systematic review and meta-analysis. Asian J Surg 44:615–628
Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL (2014) Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 259:549–555
Gedaly R, Pomposelli JJ, Pomfret EA, Lewis WD, Jenkins RL (1999) Cavernous hemangioma of the liver: anatomic resection vs enucleation. Arch Surg 134:407–411
Hamaloglu E, Altun H, Ozdemir A, Ozenc A (2005) Giant liver hemangioma: therapy by enucleation or liver resection. World J Surg 29:890–893
Singh RK, Kapoor S, Sahni P, Chattopadhyay TK (2007) Giant haemangioma of the liver: is enucleation better than resection? Ann R Coll Surg Engl 89:490–493
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK, Jang JY, Choi H, Jang JS, Kwon SU (2016) Comparison of laparoscopic liver resection for hepatocellular carcinoma located in the posterosuperior segments or anterolateral segments: a case-matched analysis. Surgery 160:1219–1226
Zheng H, Huang SG, Qin SM, Xiang F (2019) Comparison of laparoscopic versus open liver resection for lesions located in posterosuperior segments: a meta-analysis of short-term and oncological outcomes. Surg Endosc 33:3910–3918
Hajibandeh S, Hajibandeh S, Dave M, Tarazi M, Satyadas T (2020) Laparoscopic versus open liver resection for tumors in the posterosuperior segments: a systematic review and meta-analysis. Surg Laparosc Endosc Percutaneous Tech 30:93–105
Tranchart H, Ceribelli C, Ferretti S, Dagher I, Patriti A (2014) Traditional versus robot-assisted full laparoscopic partial hepatectomy: a matched-pair comparative study. World J Surg 38:2904–2909
Casciola L, Patriti A, Ceccarelli G, Bartoli A, Ceribelli C, Spaziani A (2011) Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc 25:3815–3824
Montalti R, Scuderi V, Patriti A, Vivarelli M, Troisi RI (2016) Robotic versus laparoscopic resections of posterosuperior segments of the liver: a propensity score-matched comparison. Surg Endosc 30:1004–1013
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38
Fu XH, Lai EC, Yao XP, Chu KJ, Cheng SQ, Shen F, Wu MC, Lau WY (2009) Enucleation of liver hemangiomas: is there a difference in surgical outcomes for centrally or peripherally located lesions? Am J Surg 198:184–187
Ho HY, Wu TH, Yu MC, Lee WC, Chao TC, Chen MF (2012) Surgical management of giant hepatic hemangiomas: complications and review of the literature. Chang Gung Med J 35:70–78
Jinhuan Y, Gang D, Binyao S, Huan M, Bin J (2020) Is laparoscopic hepatectomy suitable for giant hepatic hemangioma larger than 10 cm in diameter? Surg Endosc 34(3):1224–1230
Ulas M, Ozer I, Bostancil EB, Karaman K, Dalgic T, Polatl E, Ercan M, Ozogul YB, Akoglul M (2014) Giant hemangiomas: effects of size and type of surgical procedure on postoperative outcome. Hepatogastroenterology 61:1297–1301
Tsilimigras DI, Moris D, Vagios S, Merath K, Pawlik TM (2018) Safety and oncologic outcomes of robotic liver resections: a systematic review. J Surg Oncol 117:1517–1530
Aziz H, Wang JC, Genyk Y, Sheikh MR (2022) Comprehensive analysis of laparoscopic, robotic, and open hepatectomy outcomes using the nationwide readmissions database. J Robot Surg 16:401–407
Murtha-Lemekhova A, Fuchs J, Hoffmann K (2022) Innovation for the sake of innovation? How does robotic hepatectomy compare to laparoscopic or open resection for HCC-A systematic review and meta-analysis. Cancers (Basel) 14:3359
Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY, Dickson PV (2017) Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford) 19:957–965
Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U (2014) Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc 28:2973–2979
Gheza F, Esposito S, Gruessner S, Mangano A, Fernandes E, Giulianotti PC (2019) Reasons for open conversion in robotic liver surgery: a systematic review with pooled analysis of more than 1000 patients. Int J Med Robot 15(2):e1976
Chong CC, Fuks D, Lee KF, Zhao JJ, Choi GH, Sucandy I, Chiow AKH, Marino MV, Gastaca M, Wang X, Lee JH, Efanov M, Kingham TP, D’Hondt M, Troisi RI, Choi SH, Sutcliffe RP, Chan CY, Lai ECH, Park JO, Di Benedetto F, Rotellar F, Sugioka A, Coelho FF, Ferrero A, Long TCD, Lim C, Scatton O, Liu Q, Schmelzle M, Pratschke J, Cheung TT, Liu R, Han HS, Tang CN, Goh BKP, International Robotic and Laparoscopic Liver Resection study group investigators (2022) Propensity score-matched analysis comparing robotic and laparoscopic right and extended right hepatectomy. JAMA Surg 157:436–444
Sucandy I, Rayman S, Lai EC, Tang CN, Chong Y, Efanov M, Fuks D, Choi GH, Chong CC, Chiow AKH, Marino MV, Prieto M, Lee JH, Kingham TP, D'Hondt M, Troisi RI, Choi SH, Sutcliffe RP, Cheung TT, Rotellar F, Park JO, Scatton O, Han HS, Pratschke J, Wang X, Liu R, Goh BKP; International Robotic, Laparoscopic Liver Resection Study Group Investigators (2022) Robotic versus laparoscopic left and extended left hepatectomy: an international multicenter study propensity score-matched analysis. Ann Surg Oncol 29(13):8398–8406
Fagenson AM, Gleeson EM, Pitt HA, Lau KN (2021) Minimally invasive hepatectomy in North America: laparoscopic versus robotic. J Gastrointest Surg 25:85–93
Funding
This work is supported by the National Natural Science Foundation of China (No. 81860117).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Drs. Wei Zhang, Junjie Liu, Zunyi Zhang, Yuwei Wang, Shuai Xiang, Lin Chen, Peng Zhu, Wanguang Zhang, Chang Shu, Wan Yee Lau, Bixiang Zhang and Xiaoping Chen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, W., Liu, J., Zhang, Z. et al. Perioperative outcomes of robot-assisted versus laparoscopic liver resection for cavernous hemangioma: a propensity score matching study. Surg Endosc 37, 4505–4516 (2023). https://doi.org/10.1007/s00464-022-09834-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09834-2