Abstract
Background and Objectives
Laparoscopic liver resection for lesions adjacent to major vasculature can be challenging, and many would consider it a contraindication. Recently, however, laparoscopic liver surgeons have been pushing boundaries and approached some of these lesions laparoscopically. We assessed feasibility, safety and oncological efficiency of this laparoscopic approach for these lesions.
Methods
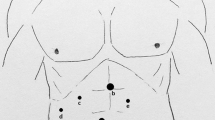
This is a monocenter study (2003–2013) describing technique and outcomes of laparoscopic liver resection for lesions adjacent to major vasculature: <2 cm from the portal vein (main trunk and first division), hepatic arteries or inferior vena cava.
Results
Thirty-seven patients underwent laparoscopic liver resection (LLR) for a lesion adjacent to major vasculature. Twenty-four (65 %) resections were for malignant disease and 92 % R0 resections. Conversion occurred in three patients (8 %). Mean operative time was 313 min (standard deviation (SD) ± 101) and intraoperative blood loss 400 ml (IQR 213-700). Clavien-Dindo complications > II occurred in two cases (5 %), with no mortality. Lesions at <1 cm were larger (7.2 cm (2.7–14) vs. 3 cm (2.5–5), p = 0.03) and operation time was longer (344 ± 94 vs. 262 ± 92 min, p = 0.01) than lesions at 1–2 cm from major vasculature.
Conclusions
Lesions <2 cm from major hepatic vasculature do not represent an absolute contraindication for LLR when performed by experienced laparoscopic liver surgeons in selected patients.

Similar content being viewed by others
References
Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, Descottes B, Valleix D, Lachachi F, Bertrand C, Mansvelt B, Hubens G, Saey JP, Schockmel R. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg 2002;236:90-97.
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-830.
Philips P, Farmer RW, Scoggins CR, McMasters KM, Martin RC 2nd. Caudate lobe resections: a single-center experience and evaluation of factors predictive of outcomes. World J Surg Oncol 2013;11:220.
Cho JY, Han HS, Yoon YS, Shin SH. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 2008;144:32-38.
Dulucq JL, Wintringer P, Stabilini C, Mahajna A. Isolated laparoscopic resection of the hepatic caudate lobe: surgical technique and a report of 2 cases. Surg Laparosc Endosc Percutan Tech 2006;16:32-35.
Yoon YS, Han HS, Cho JY, Ahn KS. Total laparoscopic liver resection for hepatocellular carcinoma located in all segments of the liver. Surg Endosc 2010;24:1630-1637.
Han HS, Cho JY, Yoon YS. Techniques for performing laparoscopic liver resection in various hepatic locations. J Hepatobiliary Pancreat Surg 2009;16:427-432.
Cho JY, Han HS, Yoon YS, Shin SH. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc 2008;22:2344-2349.
Ai JH, Li JW, Chen J, Bie P, Wang SG, Zheng SG. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5-10 cm. PLoS One 2013;8:1-7.
Abu Hilal M, Di Fabio F, Abu Salameh M, Pearce NW. Oncological efficiency analysis of laparoscopic liver resection for primary and metastatic cancer: a single-center UK experience. Arch Surg 2012;147:42-48.
Abu Hilal M, Pearce NW. Laparoscopic left lateral liver sectionectomy: a safe, efficient, reproducible technique. Dig Surg 2008;25:305-308.
Pearce NW, Di Fabio F, Teng MJ, et al. Laparoscopic right hepatectomy: a challenging, but feasible, safe and efficient procedure. Am J Surg 2011;202:e52-e58.
Yoon YS, Han HS, Cho JY, Kim JH, Kwon Y. Laparoscopic liver resection for centrally located tumors close to the hilum, major hepatic veins, or inferior vena cava. Surgery 2013;153:502-509.
Ikai I, Arii S, Kojiro M, Ichida T, Makuuchi M, Matsuyama Y, Nakanuma Y, Okita K, Omata M, Takayasu K, Yamaoka Y. Re-evaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a Japanese nationwide survey. Cancer 2004;101:796-802.
Torzilli G, Montorsi M, Del Fabbro D, Palmisano A, Donadon M, Makuuchi M. Ultrasonographically guided surgical approach to liver tumours involving the hepatic veins close to the caval confluence. Br J Surg 2006;93:1238-1246.
Nara S, Shimada K, Sakamoto Y, Esaki M, Kishi Y, Kosuge T, Ojima H. Prognostic impact of marginal resection for patients with solitary hepatocellular carcinoma: evidence from 570 hepatectomies. Surgery 2012;151:526-536.
Abu Hilal M, Underwood T, Zuccaro M, Primrose J, Pearce N. Short- and medium-term results of totally laparoscopic resection for colorectal liver metastases. Br J Surg 2010;97:927-933.
Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection - 2,804 patients. Ann Surg 2009;250:831-841.
Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. World J Surg. 2011;35:1478-1486.
Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg 2013;257:205-213.
Abu Hilal M, Di Fabio F, Syed S, Wiltshire R, Dimovska E, Turner D, Primrose JN, Pearce NW. Assessment of the financial implications for laparoscopic liver surgery: a single-centre UK cost analysis for minor and major hepatectomy. Surg Endosc 2013;27:2542-2550.
Abu Hilal M, Di Fabio F, Teng MJ, Lykoudis P, Primrose JN, Pearce NW. Single-centre comparative study of laparoscopic versus open right hepatectomy. J Gastrointest Surg 2011;15:818-823.
Conflict of Interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hilal, M.A., van der Poel, M.J., Samim, M. et al. Laparoscopic Liver Resection for Lesions Adjacent to Major Vasculature: Feasibility, Safety and Oncological Efficiency. J Gastrointest Surg 19, 692–698 (2015). https://doi.org/10.1007/s11605-014-2739-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2739-2