Abstract
Background
At least 25 metabolic/bariatric procedures have been proposed globally, 5 formally endorsed. A newer procedure, sleeve gastrectomy with transit bipartition (SG + TB), appears to markedly reduce weight and improve metabolic syndrome while being relatively simple technically and protective of long-term nutritional stability. We aimed to investigate SG + TB effectiveness and safety.
Methods
In a single-center retrospective analysis of prospectively collected data, SG + TB patients were followed through 12 months. Primary outcomes were changes in weight [body mass index (BMI), total weight loss (TWL)], metabolic parameters [HbA1C, LDL cholesterol, triglycerides (TG), hypertension], and nutritional status. Repeated-measures analysis of variance (ANOVA) was used to assess changes in weight and metabolic parameters at 1, 3, 6, 9, and 12 months after surgery.
Results
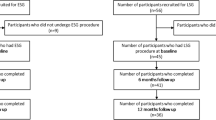
Between 2015 and 2019, 883 patients (mean age 51.8 yrs, BMI 34.1 ± 5.0 kg/m2) underwent SG + TB. Mean operative time was 124 ± 25.4 min; hospitalization, 4.0 ± 2.5 days.
ANOVA indicated significant reductions in weight and metabolic parameters (p < 0.005). In 646 patients with complete weight data at 12 months, mean BMI was reduced to 27.2 ± 3.4 kg/m2 (p < 0.001), TWL 19.8 ± 6.0%. HbA1C was normalized in 83.3% of SG + TB patients; hyperlipidemia, hypertension, and hypertriglyceridemia were significantly reduced (p < 0.001). Also, there was a significant reduction in the proportion of patients outside normal nutritional reference ranges. The overall complication rate was 10.2%. There was no mortality.
Conclusion
In a series of 833 lower-BMI patients who underwent SG + TB and were followed through 12 months (73.2% follow-up), significant weight loss, comorbidity reduction, and nutritional stability were attained with few major complications and no mortality.




Similar content being viewed by others
References
World Health Organization (WHO) (2020) Fact sheet: obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. 2020; Accessed 19 November 2020.
Tobias DK, Hu FB (2018) The association between BMI and mortality: implications for obesity prevention. Lancet: Diabetes Endocrinol 6(12):916–7
Centers for Disease Control and Prevention (2020) Healthy weight, nutrition, and physical activity. Available at: https://www.cdc.gov/healthyweight/index.html; Accessed 22 November 2020.
Sudlow A, le Roux CW, Pournaras DJ (2020) The metabolic benefits of different bariatric operations: what procedure to choose? Endocr Connect 9(2):R28–R35
Bhandari M, Fobi MAL, Buchwald JN, and the BMSS Working Group (2019) Standardization of bariatric metabolic procedures:world consensus meeting statement. Obes Surg. https://doi.org/10.1007/s11695-019-04032-x
Santoro S, Malzoni CE, Velhote MCP (2006) Digestive adaptation with intestinal reserve: a neuroendocrine-based procedure for morbid obesity. Obes Surg 16:1371–1379
Topart P, Becouarn G, Finel JB (2020) Is transit bipartition a better alternative to biliopancreatic diversion with duodenal switch for superobesity? Comparison of the early results of both procedures. Surg Obes Relat Dis 16:497–502
Topart PA, Becouarn G (2015) Revision and reversal after biliopancreatic diversion for excessive side effects or ineffective weight loss: a review of the current literature on indications and procedures. Surg Obes Relat Dis 11(4):965–972
Santoro S, Castro LC, Velhote MC, Malzoni CE, Klajner S, Castro LP et al (2012) Sleeve gastrectomy with transit bipartition: a potent intervention for metabolic syndrome and obesity. Ann Surg 256(1):104–110
Azevedo FR, Santoro S, Correa-Giannella ML, Toyoshima MT, Giannella-Neto D, Calderaro D et al (2018) A prospective randomized controlled trial of the metabolic effects of sleeve gastrectomy with transit bipartition. Obes Surg 28(10):3012–19
Topart P, Becouarn G, Finel JB (2020) Comparison of 2-year results of Roux-en-Y gastric bypass and transit bipartition with sleeve gastrectomy for superobesity. Obes Surg 30(9):3402–07
Rubino F, Nathan DM, Eckel RH et al (2016) Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 39:861–877
American Diabetes Association (2017) Obesity management for the treatment of type 2 diabetes. Diabetes Care 40:S57–S63
Celik A, Pouwels S, Karaca FC, Cagiltay E, Ugale S, Etikan I et al (2017) Time to glycemic control—an observational study of 3 different operations. Obes Surg 27:694–702
Cagiltay E, Celik A, Dixon J, Pouwels S, Santoro S, Gupta A, Ugale S, Abdul-Ghani M (2020) Effects of different metabolic states and surgical models on glucose metabolism and secretion of ileal L-cell peptides: Results from the HIPER-1 study. Diabetic Med 37:697–704
Kim H-Y (2013) Statistical notes for clinical researchers: assessing normal distribution using skewness and kurtosis. Restor Dent Endod 38:52–54
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and over-weight: a systematic review and meta-analysis. BMC Public Health 9:88
Aminian A, Chang J, Brethauer SA, Kim JJ, for the American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2018) ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30–35 kg/m2). Surg Obes Relat Dis 14(8):1071–1087
Whitlock G, Lewington S, Sherlicker P et al (2009) Prospective studies collaboration. Body-mass index and cause- specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet 373(9669):1083–96
Rodrigues MR, Santo MA, Favero GM, Vieira EC, Artoni RF, Nogaroto V et al (2015) Metabolic surgery and intestinal gene expression: digestive tract and diabetes evolution considerations. World J Gastroenterol 21(22):6990–98
Yormaz S, Yılmaz H, Ece I et al (2018) Laparoscopic ileal interposition with diverted sleeve gastrectomy versus laparoscopic transit bipartition with sleeve gastrectomy for better glycemic outcomes in T2DM patients. Obes Surg 28:77–86
Karaca FC (2020) Effects of sleeve gastrectomy with transit bipartition on glycemic variables, lipid profile, liver enzymes, and nutritional status in type 2 diabetes mellitus patients. Obes Surg 30:1437–1445
Rao W-S, Shan C-X, Zhang W, Jiang D-Z, Qui M (2015) A meta-analysis of short-term outcomes of patients with type 2 diabetes mellitus and BMI ≤ 35 kg/m2 undergoing Roux-en-Y gastric bypass. World J Surg 39(1):223–30
Acknowledgements
We thank J. N. Buchwald, Medwrite Medical Communications, and T. W. McGlennon, McGlennon MotiMetrics, Maiden Rock, WI, USA who received a grant for assistance with statistical analysis and manuscript development.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Halit Eren Taskin, MD has no conflicts of interest or financial ties to disclose. Dr. Muzaffer Al, MD has no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures of the study are compliant with the ethical standards of Near East University Faculty of Medicine, Department of Surgery, Nicosia, Turkey. The Institutional Review Board of Buyak Anadolu Hospital approved the study (#261020-04).
Informed consent
Informed consent was obtained from all study participants.
Human and animal rights
The study was performed in accord with the ethical standards of the 1964 Declaration of Helsinki and subsequent amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al, M., Taskin, H.E. Sleeve gastrectomy with transit bipartition in a series of 883 patients with mild obesity: early effectiveness and safety outcomes. Surg Endosc 36, 2631–2642 (2022). https://doi.org/10.1007/s00464-021-08769-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08769-4