Abstract
Background
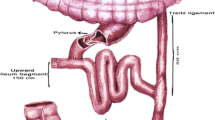
Sleeve gastrectomy with transit bipartition (SG + TB) surgery is an effective treatment modality for the patients with type 2 diabetes mellitus (T2DM). Here, we aimed to present the 1-year follow-up data of our patients with T2DM who underwent SG + TB.
Methods
We evaluated the follow-up results of 45 patients and evaluated the remission status of T2DM. Additionally, biochemical variables including lipid status, liver function and nutritional status were presented.
Results
A total of 40 T2DM remissions occurred among the 45 patients (88.8%). The complete remission was present in 35 of the patients at the end of the postoperative first year. The lipid profile markers improved following the first postoperative month. The levels of the liver enzyme alanine aminotransferase (ALT) decreased after the first postoperative month, while aspartate aminotransferase (AST) levels did not alter significantly during the follow-up period. We did not observe a change regarding albumin and vitamin B12 levels following the surgery.
Conclusion
SG + TB is a convenient and therapeutic method for the treatment of T2DM, along with the improvement in lipid profile and liver enzyme levels.
Similar content being viewed by others
References
WHO. Global report on diabetes. 2006. Available at: https://www.who.int/diabetes/global-report/en/. Accessed on 21/08/2019
Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world - a growing challenge. N Engl J Med. 2007;356:213–5. https://doi.org/10.1056/NEJMp068177.
Rubino F, Nathan DM, Eckel RH, et al. Cummings DE; delegates of the 2nd diabetes surgery summit. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care. 2016;39(6):861–77. https://doi.org/10.2337/dc16-0236.
Santoro S, Malzoni CE, Velhote MCP, et al. Digestive adaptation with intestinal reserve: a neuroendocrine-based procedure for morbid obesity. Obes Surg. 2006;16(10):1371–9. https://doi.org/10.1381/096089206778663841.
Santoro S, Castro LC, Velhote MC, et al. Sleeve gastrectomy with transit bipartition: a potent intervention for metabolic syndrome and obesity. Ann Surg. 2012 Jul;256(1):104–10. https://doi.org/10.1097/SLA.0b013e31825370c0.
Aminian A, Brethauer SA, Andalib A, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266(4):650–7. https://doi.org/10.1097/SLA.0000000000002407.
Ghio B, Jiménez A, Corcelles R, et al. Midterm effects of bariatric surgery in patients with insulin-treated type 2 diabetes. Surg Obes Relat Dis. 2016;13:2004. https://doi.org/10.1016/j.soard.2016.12.030.
Santoro S. From bariatric to pure metabolic surgery: new concepts on the rise. Ann Surg. 2015;262:79–80.
Yormaz S, Yılmaz H, Ece I, et al. Laparoscopic Ileal interposition with diverted sleeve gastrectomy versus laparoscopic transit bipartition with sleeve gastrectomy for better glycemic outcomes in T2DM patients. Obes Surg. 2018;28(1):77–86. https://doi.org/10.1007/s11695-017-2803-6.
American Diabetes Association. Standards of medical care in diabetes-2012. Diabetes Care. 2012;35(Suppl 1):S11–63. https://doi.org/10.2337/dc12-s011.
Renquist K, Jeng G, Mason EE, et al. Calculating Follow-up Rates. Obes Surg. 1992;2:361–7. https://doi.org/10.1381/096089292765559963.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5. https://doi.org/10.2337/dc09-9036.
Matsuzaka T, Shimano H. Molecular mechanisms involved in hepatic steatosis and insulin resistance. J Diabetes Investig. 2011;2(3):170–5. https://doi.org/10.1111/j.2040-1124.2011.00111.x.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51. https://doi.org/10.1056/NEJMoa1600869.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76. https://doi.org/10.1056/NEJMoa1200225.
Dixon JB, le Roux CW, Rubino F, et al. Bariatric surgery for type 2 diabetes. Lancet. 2012;379(9833):2300–11. https://doi.org/10.1016/S0140-6736(12)60401-2.
Azevedo FR, Santoro S, Correa-Giannella ML, et al. Caramelli B.a prospective randomized controlled trial of the metabolic effects of sleeve gastrectomy with transit bipartition. Obes Surg. 2018;28(10):3012–9. https://doi.org/10.1007/s11695-018-3239-3.
Golomb I, Ben David M, Glass A, et al. Long-term metabolic effects of laparoscopic sleeve gastrectomy. JAMA Surg. 2015;150(11):1051–7. https://doi.org/10.1001/jamasurg.2015.2202.
Kashyap SR, Bhatt DL, Wolski K, et al. Metabolic effects of bariatric surgery in patients with moderate obesity and type 2 diabetes: analysis of a randomized control trial comparing surgery with intensive medical treatment. Diabetes Care. 2013 Aug;36(8):2175–82. https://doi.org/10.2337/dc12-1596.
Celik A, Ugale S. Functional restriction and a new balance between proximal and distal gut: the tools of the real metabolic surgery. Obes Surg. 2014;24(10):1742–3. https://doi.org/10.1007/s11695-014-1368-x.
Lee WJ, Almulaifi AM, Tsou JJ, et al. Duodenal–jejunal bypass with sleeve gastrectomy versus the sleeve gastrectomy procedure alone: the role of duodenal exclusion. Surg Obes Relat Dis. 2015;11(4):765–70. https://doi.org/10.1016/j.soard.2014.12.017.
Chao SH, Lin CL, Lee WJ, et al. Proximal Jejunal bypass improves the outcome of gastric clip in patients with obesity and type 2 diabetes mellitus. Obes Surg. 2019;29(4):1148–53. https://doi.org/10.1007/s11695-018-3607-z.
Lin S, Guan W, Yang N, et al. Short-term outcomes of sleeve gastrectomy plus jejunojejunal bypass: a retrospective comparative study with sleeve gastrectomy and Roux-en-Y gastric bypass in Chinese patients with BMI ≥ 35 kg/m2. Obes Surg. 2019;29(4):1352–9. https://doi.org/10.1007/s11695-018-03688-1.
Andrès E, Serraj K, Zhu J, et al. The pathophysiology of elevated vitamin B12 in clinical practice. QJM Int J Med. 2013;106(6):505–15. https://doi.org/10.1093/qjmed/hct051.
Aminian A, Chang J, Brethauer SA, et al. ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30-35 kg/m2). Surg Obes Relat Dis. 2018;14(8):1071–87. https://doi.org/10.1016/j.soard.2018.05.025.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author does not have any conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(MP4 105517 kb)
Rights and permissions
About this article
Cite this article
Karaca, F.C. Effects of Sleeve Gastrectomy with Transit Bipartition on Glycemic Variables, Lipid Profile, Liver Enzymes, and Nutritional Status in Type 2 Diabetes Mellitus Patients. OBES SURG 30, 1437–1445 (2020). https://doi.org/10.1007/s11695-019-04326-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04326-0