Abstract
Objective
In this study, we evaluated the short-term outcomes following three-dimensional (3D) or two-dimensional (2D) laparoscopic surgery for patients with gastric cancer.
Background
There is a lack of prospective evidence regarding the safety and efficacy of 3D versus 2D laparoscopic surgery for patients with gastric cancer. Therefore, we conducted a phase III single-center, prospective, randomized, controlled trial to compare 3D and 2D laparoscopic surgery for patients with gastric cancer.
Methods
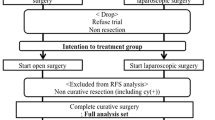
We compared operation time, intraoperative blood loss, number of lymph node dissections, morbidity, and mortality between the 3D and 2D groups following laparoscopic surgery for gastric cancer. The study is registered at ClinicalTrials.gov with ID number NCT02327481.
Results
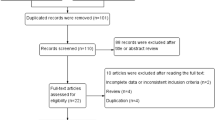
A total of 228 patients were randomized (3D group 115 cases; 2D group 113 cases) between January 1, 2015 and September 1, 2015. Seven patients who underwent exploratory operations were excluded. Finally, a total of 221 patients were analyzed (3D group 109 cases, 2D group 112 cases). There were no significant differences between the two groups regarding the clinical pathological characteristics, operating time (3D vs. 2D, 184 ± 36 vs. 178 ± 37 min, P = 0.288), number of lymph node dissections (36 ± 14 vs. 37 ± 13, P = 0.698), time to first ambulation (2.27 ± 1.60 vs. 2.04 ± 0.84, P = 0.18), flatus (3.89 ± 1.49 vs. 3.69 ± 1.12, P = 0.255), liquid diet (4.88 ± 1.88 vs. 4.79 ± 1.57, P = 0.684), or duration of postoperative hospital stay (12.52 ± 4.83 vs. 12.63 ± 7.32, P = 0.903). The postoperative complication rates of the 3D and 2D groups were 18.3 and 16.1%, respectively, P = 0.723. No patients died during the postoperative hospital stay. However, the intraoperative blood loss in the 3D group was significantly lower than the 2D group (58 ± 75 vs. 78 ± 72 ml, P = 0.047).
Conclusion
There was no significant difference in operation time and number of lymph node harvested between the 3D and 2D groups; however, 3D laparoscopic surgery may reduce the intraoperative blood loss compared to 2D procedure. Therefore, we conclude that this trial is safe and is thus ongoing.

Similar content being viewed by others
References
Kitano S, Iso Y, Moriyama M et al (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Nicolau S, Soler L, Mutter D et al (2011) Augmented reality in laparoscopic surgical oncology. Surg Oncol 20:189–201
Sinha R, Sundaram M, Raje S et al (2013) 3D laparoscopy: technique and initial experience in 451 cases. Gynecol Surg 10:123–128
Aykan S, Singhal P, Nguyen DP et al (2014) Perioperative, pathologic, and early continence outcomes comparing three-dimensional and two-dimensional display systems for laparoscopic radical prostatectomy—a retrospective, single-surgeon study. J Endourol 28:539–543
Storz P, Buess GF, Kunert W et al (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26:1454–1460
Blavier A, Gaudissart Q, Cadière GB et al (2007) Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 194:115–121
Chiu CJ, Lobo Prabhu K, Tan-Tam CC et al (2015) Using three-dimensional laparoscopy as a novel training tool for novice trainees compared with two-dimensional laparoscopy. Am J Surg 209:824.el–827.el (discussion 827)
Velayutham V, Fuks D, Nomi T et al (2016) 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc 30:147–153
Currò G, La Malfa G, Caizzone A et al (2015) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery: a single-Surgeon Prospective Randomized Comparative Study. Obes Surg 25:2120–2124
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14(2):113–123
Huang C-M, Zheng CH (eds) (2015) Laparoscopic gastrectomy for gastric cancer. Springer, Berlin
Dindo D, Demartines N, Clavien PA et al (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Lee JH, Park DJ, Kim HH et al (2012) Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien–Dindo classification. Surg Endosc 26:1287–1295
Smith R, Day A, Rockall T et al (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26:1522–1527
Chan AC, Chung SC, Yim AP et al (1997) Comparison of two-dimensional versus three-dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Hanna GB, Shimi SM, Cuschieri A et al (1998) Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251
Mueller MD, Camartin C, Dreher E, Hänggi W et al (1999) Three-dimensional laparoscopy. Gadget or progress? A randomized trial on the efficacy of three-dimensional laparoscopy. Surg Endosc 13:469–472
Zhou J, Xu HJ, Liang CZ et al (2015) A comparative study of distinct ocular symptoms after performing laparoscopic surgical tasks using a three-dimensional surgical imaging system and a conventional two-dimensional surgical imaging system. J Endourol 29:816–820
Alaraimi B, El Bakbak W, Sarker S et al (2014) A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) versus two-dimensional (2D) laparoscopy. World J Surg 38:2746–2752
Usta TA, Ozkaynak A, Kovalak E et al (2015) An assessment of the new generation three-dimensional high definition laparoscopic vision system on surgical skills: a randomized prospective study. Surg Endosc 29:2305–2313
Sahu D, Mathew MJ, Reddy PK (2014) 3D laparoscopy—help or hype; initial experience of A tertiary Health Centre. J Clin Diagn Res 8:NC01–NC03
Sun CC, Chiu AW, Chen KK et al (2000) Assessment of a three-dimensional operating system with skill tests in a pelvic trainer. Urol Int 64:154–158
Wagner OJ, Hagen M, Kurmann A et al (2012) Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 26:2961–2968
Hasson HM, Jason H (2007) Information retention and skill acquisition after CME meetings. Laparosc Today 6:4–6
Mizuno A, Kanda M, Kobayashi D et al (2016) Adverse effects of intraoperative blood loss on long-term outcomes after curative gastrectomy of patients with stage II/III gastric cancer. Dig Surg 33:121–128
Acknowledgements
The authors are thankful to Fujian Medical University Union Hospital for their management of our gastric cancer patient database.
Funding
The study was sponsored by the National Key Clinical Specialty Discipline Construction Program of China (No. [2012]649) and the Key Projects of Science and Technology Plan of Fujian Province (No. 2014Y0025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jun Lu, Chao-Hui Zheng, Chang-Ming Huang designed the study; Hua-Long Zheng, Ping Li, Jian-Wei Xie, Jia-Bin Wang, Jian-Xian Lin collected the data. All the authors participated in interpreting the data, drafting the article, critically revising the paper for content, and providing final approval of the version submitted for publication. All the authors have seen, approved, and are completely familiar with the contents of the manuscript. All the authors are responsible for the accuracy of the manuscript, including the statistical calculations. No author has any financial conflicts of interest.
Rights and permissions
About this article
Cite this article
Lu, J., Zheng, CH., Zheng, HL. et al. Randomized, controlled trial comparing clinical outcomes of 3D and 2D laparoscopic surgery for gastric cancer: an interim report. Surg Endosc 31, 2939–2945 (2017). https://doi.org/10.1007/s00464-016-5310-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5310-2