Abstract
Background
Two-dimensional (2D) view is known to cause practical difficulties for surgeons in conventional laparoscopy. Our goal was to evaluate whether the new-generation, Three-Dimensional Laparoscopic Vision System (3D LVS) provides greater benefit in terms of execution time and error number during the performance of surgical tasks.
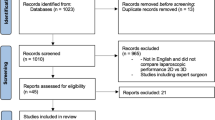
Methods
This study tests the hypothesis that the use of the new generation 3D LVS can significantly improve technical ability on complex laparoscopic tasks in an experimental model. Twenty-four participants (8 experienced, 8 minimally experienced, and 8 inexperienced) were evaluated for 10 different tasks in terms of total execution time and error number. The 4-point lickert scale was used for subjective assessment of the two imaging modalities.
Results
All tasks were completed by all participants. Statistically significant difference was determined between 3D and 2D systems in the tasks of bead transfer and drop, suturing, and pick-and-place in the inexperienced group; in the task of passing through two circles with the needle in the minimally experienced group; and in the tasks of bead transfer and drop, suturing and passing through two circles with the needle in the experienced group. Three-dimensional imaging was preferred over 2D in 6 of the 10 subjective criteria questions on 4-point lickert scale.
Conclusions
The majority of the tasks were completed in a shorter time using 3D LVS compared to 2D LVS. The subjective Likert-scale ratings from each group also demonstrated a clear preference for 3D LVS. New 3D LVS has the potential to improve the learning curve, and reduce the operating time and error rate during the performances of laparoscopic surgeons. Our results suggest that the new-generation 3D HD LVS will be helpful for surgeons in laparoscopy (Clinical Trial ID: NCT01799577, Protocol ID: BEHGynobs-4).


Similar content being viewed by others
References
Bhayani SB, Andriole GL (2005) Three-dimensional (3D) vision: does it improve laparoscopic skills? An assessment of a 3D head-mounted visualization system. Rev Urol 7:211–214
Chan AC, Chung SC, Yim AP et al (1997) Comparison of two-dimensional versus three-dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Byrn JC, Schluender S, Divino CM et al (2007) Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System. Am J Surg 193:519–522
Ohuchida K, Kenmotsu H, Yamamoto A, Sawada K, Hayami T, Morooka K, Hoshino H, Uemura M, Konishi K, Yoshida D, Maeda T, Ieiri S, Tanoue K, Tanaka M, Hashizume M (2009) The effect of CyberDome, a novel three-dimensional dome-shaped display system, on laparoscopic procedures. Int J Comput Assist Radiol Surg 4(2):125–132
Becker H, Melzer A, Schurr MO, Buess G (1993) 3D video techniques in endoscopic surgery. Endosc Surg Allied Technol 1(40–46):2
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, Greco F, Carvalho-Dias E, Mota P, Nogueira C, Pinho P, Mirone V, Correia-Pinto J, Rassweiler J, Lima E (2013) Three-dimensional versus standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82(6):1444–1450
Patel HRH, Ribal MJ, Arya M, Nauth-Misir R, Joseph JV (2007) Is it worth revisiting laparoscopic three-dimensional visualization? a validated assessment original research article. Urology 70(1):47–49
Birkett DH, Josephs LG, Este-McDonald J (1994) A new 3D laparoscope in gastrointestinal surgery. Surg Endosc 8:1448–1451
van Bergen P, Kunert W, Schurr MO et al (1996) Comparative study of endoscopic 2D and 3D imaging systems. Langenbecks Arch Chir Suppl Kongressbd 113:634–637
Taffinder N, Smith SG, Huber J et al (1999) The effect of a second generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13:1087–1092
Sun CC, Chiu AW, Chen KK et al (2000) Assessment of a three-dimensional operating system with skill tests in a pelvic trainer. Urol Int 64:154–158
Buchs NC, Volonte F, Pugin F, Toso C, Morel P (2013) Three-dimensional laparoscopy: a step toward advanced surgical navigation. Surg Endosc 27:692–693
Durrani AF, Preminger GM (1994) Advanced endoscopic imaging: 3D laparoscopic endoscopy. Surg Technol Int 3:141–147
Thomsen MN, Lang RD (2004) An experimental comparison of three-dimensional and two-dimensional endoscopic systems in a model. Arthroscopy 20:419–423
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardized phantom tasks. Surg Endosc 26:1454–1460
Silvestri M, Simi M, Cavallotti C, Vatteroni M, Ferrari V, Freschi C, Valdastri P, Menciassi A, Dario P (2011) Autostereoscopic three-dimensional viewer evaluation through comparison with conventional interfaces in laparoscopic surgery. Surg Innov 18(3):223–230
Blavier A, Gaudissart Q, Cadiere GB, Nyssen AS (2007) Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 194:115–121
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study on influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251
Coren S, Ward LM (1989) Sensation and perception. Harcourt Brace Jovanovich College Publishers, Orlando, pp 17–19
Khoshabeh R, Juang J, Talamini MA, Nguyen TQ (2012) Multiview glasses-free 3D laparoscopy. IEEE Trans Biomed Eng 59(10):2859–2865
Gofrit ON, Mikhail AA, Zorn KC, Zagaja GP, Steinberg GD, Shalhav AL (2008) Surgeons’ perceptions and injuries during and after urologic laparoscopic surgery. Urology 71:404–407
Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, Benway BM (2012) 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A 22(9):865–870
Crosthwaite G, Chung T, Dunkley P, Shimi S, Cuschieri A (1995) Comparison of direct vision and electronic two- and three-dimensional display systems on surgical task efficiency in endoscopic surgery. Br J Surg 82:849–851
Rabin J (1995) Two eyes are better than one: binocular enhancement in the contrast domain. Ophthalmic Physiol Opt 15:45–48
Pietrabissa A, Scarcello E, Mosca F (1994) Three-dimensional versus two-dimensional video system for the trained endoscopic surgeon and the beginner. End Surg 2:315–317
Cagenello R, Arditi A (1993) Binocular enhancement of visual acuity. J Opt Soc Am A 10:1841–1848
Jones DB, Brewer JD, Soper NJ (1996) The influence of three-dimensional video systems on laparoscopic surgery. Surg Laparosc Endosc 6:191–197
Yohannes P, Rotariu P, Pinto P et al (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60:39–45
Danis J (1996) Theoretical basis for camera control in teleoperating. Surg Endosc 10:804–808
Mueller MD, Camartin C, Dreher E et al (1999) Three-dimensional laparoscopy: gadget or progress? A randomized trial on the efficacy of three-dimensional laparoscopy. Surg Endosc 13:469–472
Ramanathan R, Salamanca JIM, Mandhani A, Leung RA, Rao SR, Berryhill R, Tewari A (2009) Does three-dimensional (3D) visualization improve the quality of assistance during robotic radical prostatectomy? World J Urol 27:95–99
Kong SH, Oh BM, Yoon H, Ahn HS, Lee HJ, Chung SG, Shiraishi N, Kitano S, Yang HK (2010) Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 24(5):1132–1143
Bilgen K, Ustun M, Karakahya M, Isik S, Sengul S, Cetinkunar S, Kucukpinar TH (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23(2):180–183
Wagner OJ, Hagen M, Kurmann A, Horgan S, Candinas D, Vorburger SA (2012) Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 26(10):2961–2968
Acknowledgments
We would like to thank all participants involved in the study including Riza Kutanis, Atilla Celik, Gülcin Ercan, Baris Sana, Hüseyin Bilge, Sinan Binboga, Rumeysa Ilkar, and Elif Gür of the Department of General Surgery; Serdar Aykan of the Department of Urology; Ulviye Hanli, Hikmet Kocer, Alper Tosun, Hüseyin Dayan, Banu Güler, Eylem Odacilar, Selim Oztürk, Gülümser Ece Aksakal, Elif Cansu Gündogdu, and Merve Ozkan of the Department of Obstetrics and Gynecology, and OR nurses and staff including Sevil Topuz, Gulluhan Erbas, and Yavuz Karayilan.
Disclosures
Drs. Usta, Ozkaynak, Kovalak, Ergul, Naki and Kaya have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Usta, T.A., Ozkaynak, A., Kovalak, E. et al. An assessment of the new generation three-dimensional high definition laparoscopic vision system on surgical skills: a randomized prospective study. Surg Endosc 29, 2305–2313 (2015). https://doi.org/10.1007/s00464-014-3949-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3949-0