Abstract
This systematic review examined (i) prevalence, severity, and impact of persistent post-extubation laryngeal injury beyond hospital discharge and (ii) differences in persistent laryngeal injury between COVID-19 and non-COVID-19 populations. The review was completed following PRISMA-2020 guidelines. Four databases (PubMed, CINHAL complete, EMBASE, Web of Science) were searched (inception to March 2021). Screening, full text review and data extraction were completed by two reviewers. Primary outcomes were swallow, voice and cough and airway measures obtained after hospital discharge. Quality assessment was measured using Downs & Black Tool and Johanna Briggs Institute Checklist for Cohort Studies. Meta-analysis was not completed due to study heterogeneity. Six cohort studies were included. Total number of participants across the included studies was 436. ICU admission diagnoses included respiratory disease 46% (COVID-19 and non-COVID-19), sepsis 14%, non-sepsis-related organ dysfunction 9%, general medical 11%, general surgical 10%, trauma 2%, ENT 0.6% and other not specified by authors 7%. Outcomes were obtained between 2 and 60 months post hospital discharge. Assessment methods included endoscopic evaluation, clinician ratings and patient-reported outcomes. Persistent features of laryngeal injury identified were airway abnormalities (18.9–27%), dysphonia (13.2–60%) and dysphagia (23–33%). Persistent laryngeal injury was associated with ICU length of stay, respiratory diagnosis and tracheostomy. Study quality ranged from poor-good. This is the first systematic review to examine post-extubation laryngeal injury beyond hospital discharge. Significant gaps in the literature were identified. Given the impact on clinical and patient outcomes, large scale, well-designed research is needed to guide post-ICU service delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endotracheal tube (ETT) intubation is an essential component of intensive care management of severe respiratory disease, though the iatrogenic effects of intubation have potential for acute and chronic complications [1]. The ETT sits in a vulnerable anatomical region for laryngeal function, and as a result, injury to the larynx is a common occurrence, with an estimated prevalence of 83% immediately following extubation [1]. While many of these injuries are self-limiting, more severe injuries may persist and require intervention [2].
Laryngeal Injury
Globally, 13–20 million patients in Intensive Care Units (ICUs) are intubated, with only a small fraction of patients emerging from intubation injury free [1]. Critically ill patients may transient or prolonged intubation, and many have conditions that predispose them to laryngeal injury [3]. Laryngeal injury may manifest as dysphagia, dysphonia, vocal cord paralysis, laryngeal oedema, granuloma and airway stenosis, though this is not an exhaustive list [1, 2]. Previous systematic reviews have investigated laryngeal injury in inpatient cohorts and reported incidence rates of airway, voice and swallow impairment as 13–31%, 76% and 3–62%, respectively [4,5,6].
Long-Term Follow-Up
Despite a growing body of evidence within inpatient populations, research examining the prevalence of persistent laryngeal injury post-hospital discharge is lacking. The impact of laryngeal injury on functional recovery from critical illness represents a research gap [4,5,6,7]. Identification and management of these symptoms in the post-acute phase is clinically important, reducing complications for patients during a vulnerable time where medical setbacks may be detrimental to recovery [8,9,10].
Coronavirus Disease-19 (COVID-19)
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) resulted in a worldwide COVID-19 pandemic in March 2020. [11]. For those where COVID-19 led to severe respiratory disease, invasive ventilation via ETT was required [12]. A distinctive characteristic of those intubated as a consequence of COVID-19 was the duration of ventilator reliance, up to twenty days and beyond [13]. Duration of intubation has previously been associated with dysphagia in adults with acute lung injury [4]. Prone ventilation was used widely in the COVID-19 cohort, with patients reported to have been in prone position for up to 17 h [14]. Though limited research exists to date, Regan et al. found prone ventilation amongst factors associated with post extubation oral intake status [15].
Study Aims
-
(i)
To systematically review the literature to examine the nature, severity, prevalence, and factors associated with features of laryngeal injury persisting beyond acute hospital discharge, in patients who underwent ETT intubation during ICU admission.
-
(ii)
To examine differences in outcomes between COVID-19 and non-COVID-19 populations.
Methods
Protocol and Registration
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement was followed [16]. The study was registered on Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42020223289). Due to the COVID-19 pandemic, the registration record was automatically published and eligibility was not checked by PROSPERO prior to publication.
Information Sources and Search Strategy
Search strategy was created alongside a subject Librarian. Four databases were searched for peer-reviewed articles: PubMed, EMBASE, CINAHL and Web of Science, from inception to March 2021. Grey literature and/or preprints were excluded. Searches were completed in the English language only. The search strategy is provided in supplementary appendix A. Following the electronic search, citations were imported to the online platform Covidence [17].
Study Selection
Title and abstract screening, full text review and extraction were completed independently by two authors. Disputes were resolved by a third-party reviewer. Given the limited research in this area, all study designs were considered for inclusion. Expert opinion, letters to the editor, commentaries and editorials were excluded. Data were then extracted to Microsoft Excel for results synthesis.
Eligibility Criteria
Studies that met the following inclusion criteria were eligible: (1) adult participants ≥ 18 years old who underwent ETT intubation during ICU admission, (2) outcomes evaluated beyond acute hospital discharge. ICU is defined as full spectrum monitoring and life support for critically ill patients [18]. Persistent laryngeal injury was defined as injuries remaining beyond hospital discharge. This definition was selected rather than a specific timepoint, so as not to exclude patients who required longer admissions. Participants who had pre-existing or co-occurring conditions known to cause dysphagia (i.e. neurological conditions, head and neck cancer) were excluded.
Outcomes
A list and definition for all outcomes were prepared in line with the PRIMSA 2020 statement [16]. Outcomes were selected with a co-author on this study who was a patient and public representative.
The primary outcomes for examination were as follows:
-
1.
Instrumental voice measures (e.g. endoscopic measures of the larynx).
-
2.
Instrumental measures of swallowing (e.g. fiberoptic endoscopic evaluation of swallowing (FEES)).
-
3.
Instrumental airway evaluation (e.g. nasendoscopy).
Secondary measures were as follows:
-
1.
Perceptual or clinically derived measures (e.g. grade, roughness, breathiness, asthenia and strain (GRBAS); [19]).
-
2.
Patient-reported outcome measures (e.g. Voice Handicap Index-10 (VHI-10) [20]).
-
3.
Functional measures (e.g. Functional Oral Intake Scale (FOIS) [21]).
Data Extraction and Quality Assessment
Following full text review and consensus on articles for inclusion, articles were extracted from Covidence [17] to Microsoft Excel for analysis. One author completed data collection from the included full texts and inputted the data to Microsoft Excel.
Data Synthesis and Analysis
Primary and secondary outcomes were collected, and analysis was carried out using descriptive statistics. General characteristics of included studies, baseline characteristics, patient demographics, assessment methods of included studies and factors associated with laryngeal injury were collated. COVID-19 studies were analysed as per the secondary aim.
Assessment of Methodological Quality
Methodological quality was assessed by two authors using the Downs and Black checklist [22] and the Joanna Briggs Institute (JBI) Checklist for Cohort Studies Critical Appraisal Tool [23]. The Downs and Black Checklist was modified for the purpose of this review, as it has been successfully adapted in previous systematic reviews [24]. Criteria regarding interventions were omitted as they were not relevant to the aims of this study. The following ranges were used: excellent (18/20), good (13/20), fair (8//20) and poor (≤ 7). The JBI does not provide a range of scores that indicate the overall quality; however, higher scores are reported to represent better methodological quality [23].
Results
Study Selection
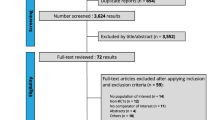
Electronic search was completed on the 1st of March 2021. In total, 127 records were identified. Following extraction, 23 duplicates were removed, and 104 records were screened. 8 studies were assessed for eligibility during full text review, with six studies eligible for inclusion. Reasons for exclusion are outlined in the PRISMA [16] diagram shown in Fig. 1.
Characteristics of Included Studies
All included studies were prospective cohort studies and were published in English. The total number of participants across the included studies was 436. The mean number of participants in each study was 73 (range 20–115). All studies reported higher percentage of male participants (mean = 65%). The mean age reported was 59 years (range 33–77 years).
Five of the included studies included ICU admission diagnoses (n = 336 participants). ICU admission diagnoses included 46% respiratory disease including COVID-19 (total n = 153: non-COVID-19 n = 92, COVID-19 n = 61), 14% sepsis (n = 48), 9% non-sepsis-related organ dysfunction (n = 30), 11% general medical diagnoses (n = 38), 10% general surgery diagnoses (n = 34), 2% trauma (n = 6), 0.6% ear nose and throat diagnosis (n = 2) and 7% other (not specified by author [27] (n = 25). Two of the six included studies reported outcomes on COVID-19 cohorts [25, 26]. No study provided the indication for intubation via ETT, grade of intubation, indication for tracheostomy or method of tracheostomy insertion. 26% of total participants were reported to have a tracheostomy during their inpatient phase (n = 116). Beyond hospital discharge, 1% of participants had a tracheostomy (n = 5).
Duration of intubation was reported by all included studies, with a mean duration of 12 days. Longer durations of intubation (mean = 30 days) were reported in the COVID-19 studies [25, 26]. When these studies were excluded, the mean duration of intubation reduced to 6 days. Duration of ICU admission was reported by three studies, with a mean duration of 12 days (range 4–22 days) [27,28,29]. Hospital length of stay was reported by one study [27]. Table 1 outlines characteristics of included studies.
Nature, Prevalence and Severity of Laryngeal Injury
Assessments used to evaluate airway, voice and swallow outcomes beyond hospital discharge included instrumental evaluation of the larynx [25, 26, 28], clinical evaluation [26, 28, 29] and patient-reported outcomes [3, 26, 27]. Outcomes were evaluated across a range of timepoints. Assessment beyond hospital discharge took place between 8 and 16 weeks in most studies [3, 25, 26, 28], with one study performing multiple follow-up assessments up to 240 weeks post hospital discharge [27].
Data were provided on n = 386 participants beyond hospital discharge. Of the included studies, four reported swallow outcomes beyond hospital discharge [25,26,27,28] and four reported voice outcomes [3, 25, 26, 29]. Two studies reported on airway, swallow and voice outcomes beyond hospital discharge [25, 26].
Airway Outcomes
Airway outcomes were evaluated using laryngoscopy [25], stroboscopy [25] and flexible nasendoscopy [26]. Both studies examined COVID-19 cohorts with a total of n = 61 participants. The prevalence of airway abnormalities reported across both studies was 18.9–27%, with unilateral vocal fold palsy most reported (7.9–40%). Other laryngeal pathologies reported included glottic stenosis (15%), subglottic stenosis (5.3–10%) and granulation tissue (10%). Severity of airway injury was not reported.
Voice Outcomes
Dysphonia was reported by four studies, with prevalence of 13.2–60% reported [3, 25, 26, 29]. Two studies used laryngoscopy [25] and one study used stroboscopy [26]. Clinician-reported outcomes were included by two studies [26, 29]. Two studies provided patient-reported outcomes [3, 26]. There was a discrepancy between clinician and patient-reported outcomes when rating the prevalence of dysphonia [26]. Severity was reported by one study [29], with 16% of patients reported as severely dysphonic and 33% moderately dysphonic.
Swallow Outcomes
Dysphagia beyond hospital discharge was reported by four studies [25,26,27,28]. Total number of participants evaluated was n = 236. Prevalence was reported as 23–33% [25,26,27,28]. One study used instrumental swallow evaluation (FEES) to report dysphagia outcomes [28], using the Penetration–Aspiration Scale (PAS) [30] to grade the severity of aspiration. The same study reported severity as 16% and oral diet restriction as 21% [28]. Patient-reported outcomes were used by two studies [25, 26].
Patient-Reported Outcome Measures
Three of the six studies included patient-reported outcome measures (PROM) [3, 26, 27]. One study [26] the VHI-10 [20] with 13.2% of patients reporting their voice as abnormal. 12.8% of patients reported symptoms of laryngopharyngeal reflux using the Reflux Symptom Index (RSI) [31]. 58% reported dysphagia on the Dysphagia Handicap Index (DHI) [32]. 30% of patients rated themselves as having an abnormal swallow on the Eating Assessment Tool-10 (EAT-10), [33]. 23% reported dysphagia using the Sydney Swallow Questionnaire (SSQ) [34].
Factors Associated with Laryngeal Injury
Three studies performed multivariable regression model analysis to determine the factors associated with prevalence of voice and swallow outcomes [27,28,29]. Respiratory diagnosis on admission to ICU [29], duration of ICU admission [27] and the presence of tracheostomy [28] are reported as factors associated with dysphonia [29] and dysphagia [27, 28]. Factors associated with airway injury were not reported. Table 2 summarises the assessment methods, prevalence and severity of laryngeal injury.
COVID-19 Patients
Two studies provided outcomes beyond hospital discharge on COVID-19 patients [25, 26]. Mean age of patients was 58 years. Age was wider ranging than non-COVID-19 cohorts (33–77 years). The mean duration of intubation reported for this cohort was 23 days, higher than the mean 6 days reported in the non-COVID-19 patients [3, 27,28,29,30,31,32,33,34,35,36,37,38,39]. One study reported that 100% of patients who underwent prone ventilation demonstrated laryngeal injury [25]. Airway abnormalities were reported as 27% [25] and 18.9% [26]. These included unilateral vocal fold immobility (40%), posterior glottic stenosis (15%), subglottic stenosis (10%), granulation tissue or edema (10%), laryngopharyngeal reflux (10%), posterior glottic diastasis (10%), muscle tension dysphonia (5%) and unrelated pre-existing conditions (15%) [25]. Rouhani et al. [26] reported unilateral vocal cord palsy in 7.9% and subglottic stenosis in 5.3%. Rouhani et al. [26] used clinical and patient-reported outcome measures to report on dysphonia and dysphagia rates. Reports of dysphonia varied from 13.2 to 53.7% [26]. Dysphagia was reported at 30% [25]. Naunheim et al. [26] reported both dysphagia and dysphonia in their outcomes but did not provide assessment methods.
Quality Assessment
Quality assessment of included studies was undertaken by two authors. The JBI Checklist [23] and the Downs and Black Checklist [22] were completed on all included studies [23]. Items responsible for lower ratings included lack of reporting of confounding factors, outcomes not measured in a valid way and insufficient duration of follow-up period. The quality of the included studies ranged from poor to good [22]. Table 3 outlines the quality assessment completed.
Discussion
Main Findings
To the authors’ knowledge, this is the first systematic review examining persistent features of laryngeal injury amongst adults who underwent endotracheal intubation, beyond hospital discharge. The prevalence of features of laryngeal injury was as follows; airway abnormalities 18.9–27%, dysphonia 13.2–60% and dysphagia 23–33% [3, 25,26,27,28,29].
Previous systematic reviews have investigated laryngeal injury in the acute phase [4,5,6,7]. While direct comparisons cannot be drawn due to the discrepancy in timepoints of assessment, previous research has reported the prevalence of laryngeal injury as 83% [4] dysphagia 41% [5] and dysphonia 73% [4]. Persistent laryngeal injury may be indicative of a more persistent impairment [2].
The cohorts across the included studies were heterogenous [25,26,27,28,29,30]. Of the studies who reported factors associated with laryngeal injury, respiratory diagnosis on admission to ICU [29], duration of ICU admission [27] and presence of tracheostomy [28] were significantly associated with dysphonia [29] and dysphagia [27, 28]. Factors associated with airway injury were not reported. This is inconsistent with previous research, which has identified the ETT size and cuff pressure [37], duration of intubation [4] and high cuff pressure impacting on the recurrent laryngeal nerve [8]. Variability in the data provided across all studies precluded statistical analysis of factors associated with persistent laryngeal injury. Future research should focus on establishing a core set of included characteristics, which would strengthen statistical analysis.
Prone ventilation was reported by the two COVID-19 studies [25, 26], though statistical analysis on the significance of this variable was not reported. Prolonged duration of mechanical ventilation has demonstrated up to 30% to muscle mass loss, and in combination with prone ventilation this may be expedited [43]. Mean duration of intubation reported in the COVID-19 cohorts was notably higher at 23 days [25, 26]. A combination of these factors may contribute to sarcopenia-related dysphagia, which has been demonstrated in elderly patients [38]. The impact of prone ventilation on laryngeal function warrants further research.
Clinical Implications
Variability in assessment methods, outcomes and timepoints of assessment reported in this systematic review add to an incomplete understanding of the long-term effects of laryngeal injury, as has been highlighted in previous research [9]. ICU represents a heterogenous cohort, and consistent reporting of patient characteristics and factors that impact laryngeal function (such as duration of intubation) are required. Variation in assessment methods and functional outcome data limit interpretation of findings. A holistic assessment of the ICU patient beyond hospital discharge, which may encompass instrumental and patient/clinician-reported outcomes is needed to develop the evidence base. Assessment across multiple timepoints will provide greater insight to the trajectory of these persistent injuries. A patient and public representative co-author on this study bring the experience of undergoing a prolonged ICU admission. They highlighted the importance of quality of life-related measures in the assessment toolkit. Additionally, the author emphasised the need to consider the patients cognitive and emotional recovery post-ICU during follow-up assessment.
Features of Laryngeal Injury-A Lasting Legacy of Critical Illness?
Only recently has attention turned to the impact of intubation on the larynx for long-term survivors of ICU admission [39]. Notably, only one study followed up patients over multiple timepoints [27]. No study reported that assessment took place as part of multidisciplinary team follow-up clinic or provided further information on the services required by the included participants. It is unlikely that persistent features of laryngeal injury exist in isolation from other post intensive care symptoms, given that more than half of all ICU patients present with new disability at 6 months post hospital discharge [40]. Understanding the trajectory of recovery and follow-up services required may further guide discussions regarding ICU follow-up and aid prognostication for this complex patient cohort.
Limitations
The authors acknowledge several limitations in this study. Searches were conducted in the English language only. No grey literature or hand searches were completed. Data needed to address the research questions were missing from the included studies. The reported prevalance and severity of the persistence of dysphagia and dysphonia in this study is largely based on patient-reported outcomes. The paucity of instrumental assessment to evaluate voice and swallow outcomes means the findings may not give a true representation of the level of impairment. The small sample size of included studies precluded statistical analysis and the heterogeneity of the studies meant meta-analysis was not possible.
Future Direction
A shift in focus towards examining the lasting effects of critical illness and improving survivor outcomes is required to fully address the long-term consequences of intensive care [41, 42]. Unfortunately, the current available evidence on airway, swallow and voice outcomes does little to address these gaps. The lack of consistent assessment methods and outcome measurement prohibits conclusions on the nature, severity and prevalence of these injuries. The need for well-designed, larger scale research is needed to provide more definitive analysis persistent features of laryngeal injury. Patient and public involvement at conception of the research design will inform the outcome measurements needed for this heterogenous population.
Conclusions
Limited evidence exists on persisting features of laryngeal injury beyond hospital discharge. This is the first systematic review to address the nature, severity and prevalence of persistent features of laryngeal injury in those who underwent endotracheal intubation during ICU admission. Significant gaps in the existing literature were identified. Persistent features of laryngeal injury reported at hospital discharge were as follows: airway abnormalities 18.9–27%, dysphonia 13.2–60% and dysphagia 23–33%. Well-designed, larger scale research is needed to determine the most appropriate assessment and management of these injuries in the post-acute phase.
References
Brodsky MB, Levy MJ, Jedlanek E, Pandian V, Blackford B, Price C, et al. Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: A systematic review. Crit Care Med. 2018;46(12):2010–7. https://doi.org/10.1097/ccm.0000000000003368.
Wallace S, McGrath BA. Laryngeal complications after tracheal intubation and tracheostomy. BJA Education. 2021. https://doi.org/10.1016/j.bjae.2021.02.005.
Shinn JR, Kimura KS, Campbell BR, Sun Lowery A, Wootten CT, Garrett CG, et al. Incidence and outcomes of acute laryngeal injury after prolonged mechanical ventilation. Crit Care Med. 2019;47(12):1699–706. https://doi.org/10.1097/ccm.0000000000004015.
Brodsky MB, Akst LM, Jedlanek E, Pandian V, Blackford B, Price C, et al. Laryngeal injury and upper airway symptoms after endotracheal intubation during surgery: A systematic review and meta-analysis. Anesth Analg. 2021;132(4):1023–32. https://doi.org/10.1213/ane.0000000000005276.
McIntyre M, Doeltgen S, Dalton N, Koppa M, Chimunda T. Post-extubation dysphagia incidence in critically ill patients: A systematic review and meta-analysis. Aust Crit Care. 2020. https://doi.org/10.1016/j.aucc.2020.05.008.
Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: A systematic review. Chest (Kojima, #211). 2010;137:665–73. https://doi.org/10.1378/chest.09-1823.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–9. https://doi.org/10.1097/CCM.0b013e318232da75.
Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: A prospective analysis of contributing factors. Laryngoscope. 2011;121(3):596–600. https://doi.org/10.1002/lary.21403.
Schefold JC, Berger D, Zürcher P, Lensch M, Perren A, Jakob SM, et al. Dysphagia in mechanically ventilated ICU patients (DYnAMICS): A prospective observational trial. Crit Care Med. 2017;45(12):2061–9. https://doi.org/10.1097/ccm.0000000000002765.
Kruser JM, Prescott HC. Dysphagia after acute respiratory distress syndrome: Another lasting legacy of critical illness. Ann Am Thoracic Soc (Kojima, #211). 2017;14:307–8. https://doi.org/10.1513/AnnalsATS.201612-1040ED.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020. https://doi.org/10.1038/s41586-020-2521-4.
Stam HJ, Stucki G, Bickenbach J. Covid-19 and post intensive care syndrome: A call for action. J Rehabil Med. 2020;52(4):jrm00044. https://doi.org/10.2340/16501977-2677.
Walter T, Zucman N, Mullaert J, et al. Extended prone positioning duration for COVID-19-related ARDS: Benefits and detriments. Crit Care. 2022;26:208. https://doi.org/10.1186/s13054-022-04081-2.
Zang X, Wang Q, Zhou H, Liu S, Xue X, Goup C-EPPS. Efficacy of early prone position for COVID-19 patients with severe hypoxia: A single-center prospective cohort study. Intens Care Med. 2020. https://doi.org/10.1007/s00134-020-06182-4.
Regan J, Walshe M, Lavan S, Horan E, Gillivan Murphy P, Healy A, et al. Post-extubation dysphagia and dysphonia amongst adults with COVID-19 in the Republic of Ireland: A prospective multi-site observational cohort study. Clin Otolaryngol. 2021. https://doi.org/10.1111/coa.13832.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021. https://doi.org/10.1016/j.ijsu.2021.105906.
Covidence systematic review software (2021). Veritas Health Innovation, Melbourne, Australia. Retrieved from: www.covidence.org
Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270–6. https://doi.org/10.1016/j.jcrc.2016.07.015.
Hirano M. Clinical examination of voice. New York: Springer Verlag; 1981.
Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549–56. https://doi.org/10.1097/00005537-200409000-00009.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20. https://doi.org/10.1016/j.apmr.2004.11.049.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Johanna Briggs Institute Critical Appraisal Tool. (2017). Checklist for Cohort Studies. Retrieved from: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Cohort_Studies2017_0.pdf
Gilheaney Ó, Zgaga L, Harpur I, Sheaf G, Kiefer L, Béchet S, Walshe M. The prevalence of oropharyngeal dysphagia in adults presenting with temporomandibular disorders associated with rheumatoid arthritis: a systematic review and meta-analysis. Dysphagia. 2017;32(5):587–600. https://doi.org/10.1007/s00455-017-9808-0.
Naunheim MR, Zhou AS, Puka E, Franco RA Jr, Carroll TL, Teng SE, et al. Laryngeal complications of COVID-19. Laryngoscope Investig Otolaryngol. 2020;5(6):1117–24. https://doi.org/10.1002/lio2.484.
Rouhani MJ, Clunie G, Thong G, Lovell L, Roe J, Ashcroft M, et al. A prospective study of voice, swallow, and airway outcomes following tracheostomy for COVID-19. Laryngoscope. 2021;131(6):E1918–25. https://doi.org/10.1002/lary.29346.
Brodsky MB, Huang M, Shanholtz C, Mendez-Tellez PA, Palmer JB, Colantuoni E, Needham DM. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors: A 5-year longitudinal study. Ann Am Thorac Soc (Kojima et al). 2017;14:376–83. https://doi.org/10.1513/AnnalsATS.201606-455OC.
Zielske J, Bohne S, Brunkhorst FM, Axer H, Guntinas-Lichius O. Acute and long-term dysphagia in critically ill patients with severe sepsis: results of a prospective controlled observational study. Eur Arch Otorhinolaryngol. 2014;271(11):3085–93. https://doi.org/10.1007/s00405-014-3148-6.
Nixon I, Ramsay S, Mackenzie K. Vocal function following discharge from intensive care. J Laryngol Otol. 2010;124(5):515–9. https://doi.org/10.1017/s0022215109992556.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8. https://doi.org/10.1007/bf00417897.
Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002;16:274–7.
Silbergleit AK, Schultz L, Jacobson BH, Beardsley T, Johnson AF. The Dysphagia handicap index: development and validation. Dysphagia. 2012;27(1):46–52. https://doi.org/10.1007/s00455-011-9336-2.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919–24. https://doi.org/10.1177/000348940811701210.
Wallace KL, Middleton S, Cook IJ. Development and validation of a self-report symptom inventory to assess the severity of oral-pharyngeal dysphagia. Gastroenterology. 2000;118(4):678–87. https://doi.org/10.1016/s0016-5085(00)70137-5.
Deary IJ, Wilson JA, Carding PN, MacKenzie K. VoiSS: A patient-derived voice symptom scale. J Psychosom Res. 2003;54(5):483–9. https://doi.org/10.1016/s0022-3999(02)00469-5.
Patterson JM, Hildreth A, McColl E, Carding PN, Hamilton D, Wilson JA. The clinical application of the 100ml water swallow test in head and neck cancer. Oral Oncol. 2011;47(3):180–4. https://doi.org/10.1016/j.oraloncology.2010.11.020.
Tadié JM, Behm E, Lecuyer L, Benhmamed R, Hans S, Brasnu D, et al. Post-intubation laryngeal injuries and extubation failure: A fiberoptic endoscopic study. Intensive Care Med. 2010;36(6):991–8. https://doi.org/10.1007/s00134-010-1847-z.
Zhao WT, Yang M, Wu HM, Yang L, Zhang XM, Huang Y. Systematic review and meta-analysis of the association between sarcopenia and dysphagia. J Nutr Health Aging. 2018;22(8):1003–9. https://doi.org/10.1007/s12603-018-1055-z.
Brodsky MB, Pandian V, Needham DM. Post-extubation dysphagia: A problem needing multidisciplinary efforts. Intensive Care Med. 2020;46(1):93–6. https://doi.org/10.1007/s00134-019-05865-x.
Higgins AM, Neto AS, Bailey M, Barrett J, Bellomo R, Cooper DJ, et al. Predictors of death and new disability after critical illness: A multicentre prospective cohort study. Intensive Care Med. 2021. https://doi.org/10.1007/s00134-021-06438-7.
Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371–9. https://doi.org/10.1097/CCM.0b013e3181fd66e5.
Zuercher P, Moret CS, Dziewas R, Schefold JC. Dysphagia in the intensive care unit: Epidemiology, mechanisms, and clinical management. Crit Care. 2019;23(1):103. https://doi.org/10.1186/s13054-019-2400-2.
Kortebein P, Symons TB, Ferrando A, Paddon-Jones D, Ronsen O, Protas E, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol Ser A. 2008;63(10):1076–81. https://doi.org/10.1093/gerona/63.10.1076.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding
Open Access funding provided by the IReL Consortium. The authors declare that they have taken no support from any organization for the submitted work. The authors also have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kelly, E., Hirschwald, J., Clemens, J. et al. Persistent Features of Laryngeal Injury Following Endotracheal Intubation: A Systematic Review. Dysphagia 38, 1333–1341 (2023). https://doi.org/10.1007/s00455-023-10559-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10559-0