Abstract
Dysphagia may present in all critically ill patients and large-scale clinical data show that e.g. post-extubation dysphagia (PED) is commonly observed in intensive care unit (ICU) patients. Recent data demonstrate that dysphagia is mostly persisting and that its presence is independently associated with adverse patient-centered clinical outcomes. Although several risk factors possibly contributing to dysphagia development were proposed, the underlying exact mechanisms in ICU patients remain incompletely understood and no current consensus exists on how to best approach ICU patients at risk.
From a clinical perspective, dysphagia is well-known to be associated with an increased risk of aspiration and aspiration-induced pneumonia, delayed resumption of oral intake/malnutrition, decreased quality of life, prolonged ICU and hospital length of stay, and increased morbidity and mortality. Moreover, the economic burden on public health care systems is high.
In light of high mortality rates associated with the presence of dysphagia and the observation that dysphagia is not systematically screened for on most ICUs, this review describes epidemiology, terminology, and potential mechanisms of dysphagia on the ICU. Furthermore, the impact of dysphagia on affected individuals, health care systems, and society is discussed in addition to current and future potential therapeutic approaches.
Similar content being viewed by others
Background
Dysphagia including post-extubation dysphagia (PED) is a concern in hospitalized patients on intensive care units (ICUs). Earlier studies, which were mostly limited by study design, patient selection, and/or limited patient numbers [1,2,3,4,5,6], reported conflicting and inconsistent results regarding the incidence of post-extubation dysphagia. In fact, incidence rates ranged from 3 to 62% [7]. Following systematic screening post-extubation, we recently published the largest prospective observational study on PED and observed that the PED incidence in unselected emergency ICU admission was 18.3% [8]. Further, PED persisted until ICU discharge in > 80% of cases and > 60% of patients with impaired deglutition on ICU remained dysphagic at hospital discharge [8]. Importantly, the presence of PED had an impact on morbidity and mortality, with an excess 90-day all-cause mortality rate of 9.2% [8].
In general medical populations, the overall burden of dysphagia on public health care system is considered high. Dysphagia-associated complications include increased risk for aspiration, aspiration-induced pneumonia [6, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], delayed resumption of oral intake/malnutrition [3, 10,11,12,13, 27, 28], decreased quality of life [21, 27], prolonged ICU and/or hospital length of stay [3, 8, 11, 14, 29], and increased morbidity and mortality [3, 6, 8, 9, 13, 27, 30,31,32,33].
Considering that post-extubation dysphagia is not routinely screened for in most ICUs [34], maybe due to limited awareness, PED appears a rather poorly recognized health care problem. Years following the latest systematic reviews on incidence and mechanisms of swallowing disorders in critically ill ICU patients [4, 7, 35], we embarked to update respective available data in the context of dysphagia epidemiology, potential mechanisms leading to dysphagia, screening approaches, and current and future treatment modalities.
Methods
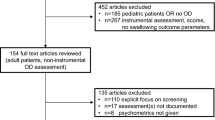
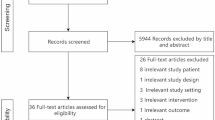
A systematic online literature search in PubMed was performed using Boolean logic combining and including the terms “dysphagia,” “swallowing dysfunction,” or “deglutition disorder” and terms reflecting “critical illness” in the titles and excluding malignancies (dysphagia[Title] OR swallowing dysfunction[Title] OR swallowing impair*[Title] OR swallowing disord*[Title] OR deglutition dysfunction[Title] OR deglutition disord* OR deglutition impair*) AND (ICU[Title] OR critical illness[Title] OR intensive care[Title] OR critical care[Title] OR critically ill[Title] OR intubation[Title] OR post-extubation[Title])NOT carcin*[Title] NOT malign*[Title] NOT cancer*[Title] NOT Tumor*[Title] NOT neopla*[Title] NOT palliat*[Title]). In total, 123 articles were included following an initial search strategy using the above stated search string. In detail, n = 103 articles were identified by the given search strategy which was followed by a search within the identified articles (identification of an additional n = 58 in-article citations). Thirty-eight articles were excluded from the final analysis (n = 12 focus on airway and/or anesthetics, n = 11 focus not on dysphagia, n = 8 pediatric and/or neonatal investigations, n = 3 not accessible, n = 2 other languages, n = 1 neuropsychiatric, n = 1 veterinarian investigation). Publications were screened for until December 2018.
Physiology of swallowing
Swallowing is a complex procedure involving more than 50 muscles, and a number of cranial nerves [36] (Fig. 1). Cortical structures involved particularly include the frontoparietal operculum, the primary sensorimotor cortex and association cortices and the anterior part of the insula. Cortico-bulbar projections then target the central pattern generators located in the dorsal medulla oblongata [37,38,39], and the solitary nucleus and nucleus ambiguous coordinate swallowing [40,41,42]. In an awake state, individuals swallow involuntarily more than once per minute. The frequency of swallowing is increasing to about > 5 times per minute during meals and decreased to about eight times per hour during sleep [43]. Four phases of swallowing can be differentiated [44]: (1) oral preparatory, (2) oral transit, (3) pharyngeal, and (4) the esophageal phase (Fig. 2). Bolus formation takes place in phase 1. In phase 2, the bolus is placed in the middle of the tongue, pushed against the hard palate and backwards to the oropharynx. When in contact with the palatoglossal arch, the swallowing reflex is triggered and the involuntary pharyngeal phase is initiated. The epipharynx is sealed and airway closure occurs in three different stages: (a) vocal cord adduction, (b) ventricular fold adduction, and (c) contact of arytenoid cartilages with the anteriorly tilted epiglottis. Importantly, active laryngeal elevation occurs which indirectly opens the upper esophageal sphincter. The bolus then enters the epiglottic valleculae and pyriforme sinuses. In the involuntary esophageal phase, peristaltic esophageal waves transport the bolus into the stomach (Fig. 2).
The swallowing network and presumed ICU-related factors for dysphagia. TBI (traumatic brain injury), stroke (ischemic/hemorrhagic), ICUAW (ICU-acquired weakness), GER (gastroesophageal reflux, CIP (critical illness polyneuropathy). Adapted from [139] with permission from the authors, copyright Heike Blum, University Hospital Münster, Germany
The four stages of swallowing (1 = oral preparatory stage, 2 = oral stage, 3–5 = pharyngeal stage, 6 = esophageal stage). Adapted from [139] with permission from the authors, copyright Heike Blum, University Hospital Münster, Germany
Pathophysiology of swallowing in critical illness
Oropharyngeal dysphagia in general can be caused by either (1) severe neurological impairment, affecting (a) the central nervous system directly (e.g., stroke, Morbus Parkinson, multiple sclerosis, or amyotrophic lateral sclerosis), (b) due to traumatic peripheral nerve damage and impaired function of the neuro-muscular junction, (c) primary neuro-muscular junction abnormalities (e.g., myasthenia gravis, Lambert-Eaton myasthenic syndrome [LEMS]), or (d) a primary muscular disease (e.g., inflammatory myopathies); (2) structural damage (e.g., trauma caused by the intubation or malignancies); (3) medication or toxic/drug side-effects; (4) presbyphagia; or (5) phagophobia [45].
In critically ill patients on the ICU, the etiology of dysphagia post-extubation appears less clear. PED is considered multifactorial with underlying mechanisms unknown, and the presence of an endotracheal tube/prolonged mechanical ventilation is considered a key risk factor for dysphagia. Six potential key mechanisms for the development of ICU-acquired swallowing disorders including PED were previously suggested [4]: (1) direct trauma caused by endotracheal and tracheostomy tubes, (2) neuromyopathy resulting in muscular weakness, (3) diminished laryngeal sensory function, (4) an impaired sensorium, reflecting a more centrally located problem, (5) gastroesophageal reflux, and (6) dyssynchronous breathing and swallowing.
In detail, direct trauma (1) seems an obvious and major mechanism in ICU-acquired swallowing dysfunction (Fig. 1). Artificial tubes of any kind, e.g., endotracheal, tracheostomy, echocardiography probes, or potentially feeding tubes, could directly cause trauma to anatomic structures. This may especially be relevant in emergency diagnostic or therapeutic interventions. Mechanical irritations of the underlying mucosal tissue may lead to focal ulceration and/or triggering of localized inflammatory processes. Scarring of the vocal cords was reported also, known as “vocal cord synechiae” [46]. Cuffed airway tubes per se prohibit normal swallowing function and active laryngeal elevation and subsequently reduce the passive opening of the upper esophageal sphincter which impedes rapid esophageal passage [45]. Two smaller studies showed contradicting results: One study [47] found no effect on penetration or aspiration by cuff status (inflated vs. deflated), but a significantly reduced score for the liquid bolus when a one-way valve was placed in comparison to in- or deflated cuff conditions (n = 14). Another study with a limited sample size (n = 7) [48] observed no significant alteration in hyoid bone movement and laryngeal excursion in cases when a tracheotomy tube was placed. Further, long-term intubation may lead to dislocation or even subluxation of arytenoid cartilages, resulting in an impaired glottis closure during swallowing [49]. Further, traumatic laryngoscopy was shown to lead to hypoglossal nerve palsy and to cause dysphagia [50,51,52,53]. Peripheral damage of the recurrent laryngeal nerve, e.g., caused by tube cuff compression (or as a complication during surgery) can result in vocal cord paresis/paralysis and may prohibit competent airway protection.
Another relevant aspect is the presence of ICU acquired weakness (ICUAW) [54]. In critically ill patients with ICUAW, general muscular weakness and muscular atrophy was reported, which may affect the swallowing apparatus [54,55,56]. ICUAW may be a consequence of “disuse” in patients receiving long-term intubation, long-term (analgo)-sedation, and/or neuromuscular blocking agents [28, 54, 57, 58]. Further, specific swallow-related muscular weakness was recently suggested in previously orally intubated acute respiratory distress syndrome patients (n = 11, median duration of intubation 14 days) after examination by videofluoroscopic swallowing study (VFSS) [59]. In addition, in ICU-acquired ventilator-induced diaphragmatic dysfunction (VIDD) [55], cough strength could be diminished leading to limited glottic clearance. Importantly, reduced local sensation appears as an additional key problem in ICU-acquired dysphagia. Either caused by direct mechanical damage, local inflammation/edema, or by critical illness polyneuropathy (CIP) [54, 56], afferent sensory pathways may be impaired leading to swallowing dysfunction [60,61,62,63]. Clinically, this may become apparent when a bolus reaches the reflex trigger zone in the palatoglossal arch but the afferent input is impaired resulting in a delayed swallow response and pre-deglutitive aspiration. However, the exact role of sensory impairment in critically ill patients appears unclear. In a recent study, no nerve conduction abnormalities were demonstrated, questioning the role of CIP in dysphagia [27].
Central (cerebral) problems in ICU-acquired swallowing disorders are mostly caused by direct damage to the central nervous system, e.g., in traumatic brain injury, stroke/hemorrhage, and/or inflammatory disorders. Contributing to this, reduced qualitative (e.g., in delirium) or quantitative level of consciousness further increases the risk for aspiration [64] and may delay therapeutic measures for dysphagia. Moreover, drug-induced effects (e.g., (analgo-) sedatives or various neurotropic medications) may affect swallowing either centrally (mostly via reduced consciousness) or peripherally (mostly at the neuro-muscular junction). In this context, another potential mechanism was suggested [4], i.e., exact coordination of laryngeal closure, apnea, and opening of the upper esophageal sphincter may be impaired. In critically ill patients, this is referred to as “dyssynchrony” between respiration and swallowing [4]. Furthermore, in critically ill patients with respiratory distress, the apnoeic period during swallowing is shortened with potential premature opening of the larynx before the bolus has passed into the esophagus [65].
Terminology of dysphagia on the ICU
Different terms are used to assess dysphagia. In the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10, WHO-Version 2016), dysphagia (R13) is listed in “Chapter XVIII: symptoms, signs and abnormal clinical and laboratory findings,” not elsewhere classified and more specified under R10–19 in “Symptoms and signs involving the digestive system and abdomen.” Dysphagia, swallowing disorder, or deglutition disorder/dysfunction are often used synonymously. In 2013, the term ICU-acquired swallowing disorder was introduced [4] suggesting multiple potential pathomechanisms in critical illness leading to acquired dysphagia in a previously dysphagia-naïve patient. International consensus on dysphagia definitions is lacking which may negatively impact on data comparability. We therefore recently proposed a delphi procedure with the aim to harmonize respective terminology [66].
Epidemiology of dysphagia on the ICU
A systematic review on the incidence of PED published in 2010 included a total of 14 studies with a total of 3520 individuals (mean of approximately 251 patients per study, median of 67) and concluded that the incidence rate ranges from 3 to 62% [7]. Study design, patient selection (e.g., assessment of patients post-aspiration), and/or limited patient numbers in respective included studies introduced a high risk of bias and showed reduced quality of evidence [1,2,3, 5, 6, 67]. In a subsequent retrospective observational cohort study, a dysphagia prevalence of up to 84% was reported [67]. A recent larger study (DYnAMICS) performed by us included 1304 medical and surgical ICU patients with potential PED risk reported an incidence rate of 12.4% (18.3% in unselected emergency admissions) after systematic screening [8]. In DYnAMICS, the incidence was likely underestimated due to exclusion of patients leaving the ICU alive with tracheostomy (no extubation/decannulation) [8].
Risk factors for dysphagia on the ICU
Risk factors for dysphagia might theoretically be inferred from the abovementioned pathomechanisms. However, studies focusing on risk factors for dysphagia following endotracheal intubation are scarce and provide conflicting results. Studies are mostly of limited sample size and either supporting or rejecting respective factors, including factors such as age [12, 19, 20, 68,69,70,71,72,73,74,75], decreased cardiac output [19, 70], intubation duration [19, 20, 22, 32, 70, 71, 73, 74], postoperative pulmonary complications [70, 74], tube feeding [19, 22, 32, 74], sepsis [6, 32, 72], transesophageal echocardiogram (TEE) [70, 71], perioperative stroke [3, 32, 69,70,71], or gastroesophageal reflux [1, 19, 76]. More consistently rejected as potential risk factors are APACHE II and SOFA scores [1, 3, 6, 9, 22, 67]; BMI [1, 6, 9]; gender [1, 6, 9, 32, 70, 75, 77, 78]; comorbidities such as arterial hypertension, kidney disease, diabetes, COPD, myocardial infarction, or heart failure [3, 19, 32, 67, 69, 70, 72], as well as smoking [32, 72]; and endotracheal tube size [3, 67, 75]. These contradicting results reflect bias due to patient selection, differing study/screening protocols, and limited patient numbers. However, despite controversial discussions, it appears that most presumed dysphagia risk factor would be duration of intubation/mechanical ventilation [1, 3, 4, 12, 32, 67, 68, 70, 78,79,80]. In addition, rather accepted risk factors [4] may include the presence of pre-existing dysphagia, local malignancy/post-surgical medical conditions affecting anatomic structures of the swallowing tract, and/or considerable quantitative/qualitative reduction of consciousness. Overall, large-scale clinical data is missing and strongly warranted in order to potentially reduce the number of patients affected by preventional measures.
Assessment of dysphagia in the critically ill
In stroke patients, early dysphagia detection minimizes the risk of aspiration [81] and systematic dysphagia screening reduces stroke-associated pneumonia rates [82]. This suggests that a systematic routine screening approach should be performed in all patients at risk without limitation to selected patient cohorts (e.g., stroke patients). Non-instrumental [66] and instrumental measures are available for timely assessment of dysphagia in the critically ill [83]. Non-instrumental assessments for dysphagia are typically performed by trained specialists (e.g., speech-language therapists, physiotherapists, or occupational therapists). The following clinical examinations were previously proposed for general populations of hospitalized (mostly non-ICU) patients: the bedside swallowing evaluation (BSE) [84], the Volume Viscosity Swallowing Test (V-VST) [85], the Mann Assessment of Swallowing Ability (MASA, K-MASA, MASA-C, MMASA) [86,87,88,89], the McGill Ingestive Swallowing Assessment (MISA, MISA-DK) [90, 91], the Gugging Swallowing Screen (GUSS) [92], the Northwestern Dysphagia Patient Check Sheet (NDPCS) [93], the Dysphagia Disorder Survey (DDS) [94], the Practical Aspiration Screening Scheme (PASS) [95], the Kuchi-Kara Taberu Index (KT Index) [96], and the Practical Assessment of Dysphagia [97] test (reviewed in [66]).
Instrumental tests, such as the flexible endoscopic evaluation of swallowing (FEES) or the VFSS, may be regarded the gold standard of dysphagia assessment in the critically ill. FEES can be performed at the ICU bed using a small flexible endoscope passing through a nostril into the epipharynx so that the oro-/ hypopharynx and the glottic area can be visualized. Using a multicolor dye technique [98], testing of different food consistencies can be performed. Further, in selected patients (depending upon availability), sensation testing can be performed using short blasts of air to the supraglottic mucous membrane for assessment of vocal cord adduction, a technique known as flexible endoscopic evaluation of swallowing with sensory testing (FEESST) [99, 100]. Apart from research, FEESST was mainly abandoned and replaced by touching the aryepiglottic area with the endoscope tip, rendering the sensation normal, absent, or reduced. In FEES, severity of penetration or aspiration is assessed using a penetration and aspiration (PAS) scale (1 indicating no penetration and 8 indicating aspiration without coughing, i.e., silent aspiration) [101]. VFSS, also referred to as “modified barium swallow,” requires patient transfer to a radiology suite, which limits feasibility in larger cohorts of critically ill patients. Although exposure to radiation may be a disadvantage, VFSS investigates the entire swallowing act, i.e., all four stages of swallowing [102, 103]. Different barium-containing food consistencies can be visualized and recorded using high-resolution imaging devices. Intra-deglutitive aspiration can be visualized. This is not possible in FEES due to a “white out”-effect caused by velum elevation. Besides providing proof for the diagnosis, effects of compensatory maneuvers and diet modifications can be studies in a real-time manner using VFSS or FEES. Further “instrumental” methods include ultrasonography [104], tissue Doppler imaging [105], high-resolution manometry [106,107,108,109,110], and oropharyngo-esophageal scintigraphy (OPES) [111]. Whereas manometry can be used to assess pharyngeal propulsion and upper esophageal sphincter performance, OPES allows detailed analysis of transit times and potential retention of a food bolus in the various anatomical areas. However, in critically ill patients post-extubation, this appears not feasible.
We recently proposed a feasible, pragmatic approach for systematic dysphagia assessment in the ICU [8]. This includes a two-step approach with systematic bedside screening for dysphagia by trained ICU nurses within few hours post-extubation, followed by an expert exam that is optimally complemented by a confirmatory FEES investigation [8].
Clinical consequences of dysphagia in the critically ill
In the critically ill, only few studies analyzed the impact of PED on patient-centered clinical outcomes. A recent retrospective study found an independent association of dysphagia with a composite endpoint of pneumonia, reintubation, or death [67]. In addition, dysphagia was associated with longer hospitalization, more discharges to a nursing home, and increased need for placement of a feeding tube [67, 77]. In a recent large prospective observational study (DYnAMICS) in a mixed population of 1304 critically ill patients with systematic bedside screening for dysphagia post-extubation, we observed an independent association of PED with 28-day and 90-day mortality after adjustment for typical confounders. An excess of 9.2% of a 90-day mortality rate was observed in patients with dysphagia [8].
In summary, the clinical consequences of dysphagia in the critically ill are important, with prolonged length of hospitalization, increased resource use, increased treatment costs, and increased mortality [8, 31, 67, 112]. Early identification of patients at risk seems warranted in an effort to minimize respective burdens.
Therapeutic considerations
Overview
The body of evidence for dysphagia treatment, especially in dysphagia-positive ICU patients, is limited. Generally, three major therapeutic pillars for dysphagia treatment are considered [113]: dietary texture modifications, postural changes/compensatory maneuvers, and interventions aiming to improve swallowing function (e.g., devices using neuromuscular stimulation).
Dietary texture modification and compensatory maneuvers
Adaptation, a term mostly used in the German-speaking literature [45], is referring to as texture modification according to the deglutition pathology and use of technical aids, e.g., prosthetics to account for velopharyngeal defects, in an effort to optimize swallowing. Compensation is referring to either compensatory maneuvers and/or postural changes to address swallowing deficiencies. Special swallowing techniques, e.g., supraglottic swallowing, may support patients with delayed swallowing reflex or incomplete laryngeal closure (e.g., after cordectomy). The patient would then be trained to hold the breath before and during swallowing and forced to cough immediately afterwards to optimize glottic/throat clearance [114, 115]. For patients with impaired laryngeal elevation, reduced tongue force, or dysfunctional opening of the upper esophageal sphincter (UES), the Mendelsohn maneuver can be applied. In this maneuver, during oral preparatory stage, the patient presses the bolus as forcefully as possible against the hard palate for up to 3 s. This elevates the larynx and improves UES opening and clearance of food residuals [116]. Postural change “chin down” reduces the distance between to the tongue basis and pharyngeal dorsal wall, hence narrowing the airway and therefore reducing the risk for leaking (bolus enters prematurely the pharynx) or aspiration within patients known for a delayed swallowing reflex. Moreover, the epiglottic vallecula gets distended, facilitating esophageal bolus passage [117,118,119].
Head movements (backwards, lateralization towards/away to the side of the paresis/palsy) may also be useful in transporting the bolus to the swallow reflex trigger area [117] or facilitating bolus passage via the healthy piriform recess [117, 120]. Functional dysphagia therapy was found successful in improving swallowing function in patients suffering from neurogenic dysphagia [121]. Apparently, an intensive therapy approach with five trainings a week seems to be more effective in the acute stage of swallowing dysfunction [122]. In addition, sphincter myotomy is an irreversible option in patients with a functionally obstructing of the upper esophageal sphincter to facilitate pharyngo-esophageal bolus propulsion [123, 124]. Medialization thyreoplasty can further be applied in patients with unilateral vocal cord paresis and suffering from aspiration to improve cough and throat clearance [125]. A laryngectomy poses a last resort for patients with persisting aspiration and suffering from repeated severe consequences. In doing this, breathing and alimentary pathways become completely separated.
Interventional/technological approaches: pharyngeal electrical stimulation
Recently, pharyngeal electrical stimulation (PES) (Fig. 3) was proposed as a novel treatment modality using a gastric feeding tube-like stimulation catheter to enhance neuromuscular pharyngeal stimulation, targeted to the individual patient. Stimulation levels are personalized at the start of the treatment to ensure that optimal levels of stimulation are delivered. PES is considered to target the afferent sensory feedback within the swallowing network that seems crucial for swallowing safety and efficacy of motor execution [126, 127]. PES may involve two postulated key modes of action: (a) facilitation of cortico-bulbar pathways [128] and (b) increase of swallowing processing efficiency in respective central nervous system areas [129], e.g., the right primary and secondary sensorimotor cortex and the right supplementary motor area. Data also demonstrate an increase of pharyngeal cortical representation and motor excitability for more than half an hour after 10 min of PES treatment. A dose-response study ([130]) showed optimal cost-effectiveness when applying a PES protocol with one cycle of 10-min stimulation per day for a total of 3 consecutive days. Further, substance P is known to enhance the swallow and cough reflex [131, 132] with reduced amounts of being observed in the sputum of elderly people suffering from aspiration pneumonia [133]. As demonstrated [134], PES may induce local substance P release into the saliva. This peripheral action with a postulated local sensitization of primary sensory neurons in the oropharyngeal effector area may then facilitate a motor swallow response by the cerebral cortex in a remote fashion.
Peripheral (pharyngeal electrical stimulation, PES) and central (transcranial direct current stimulation, tDCS) stimulation strategies targeting the swallowing network. Reprinted with permission from the authors [140], copyright Heike Blum, University Hospital Münster, Germany
Recently, PES was shown of therapeutic potential, especially within selected patient populations, i.e., in patients with post-stroke dysphagia (PSD). In a cohort of patients with severe persisting PSD with tracheostomy and decannulation failure, a recent study could demonstrate enhanced remission of dysphagia resulting in decannulation in 75% of PES-treated patients vs. 20% of patients decannulated in sham-treated individuals [129]. Two recently published studies support respective findings [135, 136]. Due to its ease of application, PES seems to be a suitable treatment approach for daily clinical practice in patients with post-stroke dysphagia. PES was validated in stroke patients, and data support a reduced hospital length of stay after treatment with PES [136].
Outlook
In the light of the fact that dysphagia is not routinely screened for in critically ill patients on most ICUs, it appears that post-extubation dysphagia awareness should be increased [137, 138] and systematic bedside screening should be implemented on the ICU [8]. Further, after identification of patients with PED on the ICU, rehabilitation measures should be started. The promising results of recent randomized controlled trials assessing PES, rTMS (repetitive transcranial magnetic stimulation), and/or tDCS (transcranial direct current stimulation) (Fig. 3) pointed to positive effects in patients with severe post-stroke dysphagia. In the future, a novel therapeutic interventions using peripheral afferent approaches (e.g., via PES) and/or central efferent stimulation of pathways of the swallowing network may be of particular interest.
Conclusions
In the light of the fact that the clinical consequences of ICU-acquired dysphagia (e.g., aspiration-induced pneumonitis/pneumonia) can often be observed on ICUs, more data on underlying mechanisms and/or risk factors seems required. Post-extubation dysphagia as a key subgroup affects a considerable number of critically ill patients and often persists far beyond ICU discharge. Awareness for dysphagia on the ICU should be increased, and systematic screening protocols should be established. Furthermore, dysphagia on the ICU appears an overlooked health care problem and studies on novel therapeutic interventions seem warranted.
References
Brodsky MB, Gellar JE, Dinglas VD, Colantuoni E, Mendez-Tellez PA, Shanholtz C, Palmer JB, Needham DM. Duration of oral endotracheal intubation is associated with dysphagia symptoms in acute lung injury patients. J Crit Care. 2014;29(4):574–9.
Brown CV, Hejl K, Mandaville AD, Chaney PE, Stevenson G, Smith C. Swallowing dysfunction after mechanical ventilation in trauma patients. J Critical Care. 2011;26(1):108 e109–113.
Macht M, King CJ, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, Moss M. Post-extubation dysphagia is associated with longer hospitalization in survivors of critical illness with neurologic impairment. Crit Care. 2013;17(3):R119.
Macht M, Wimbish T, Bodine C, Moss M. ICU-acquired swallowing disorders. Crit Care Med. 2013;41(10):2396–405.
Moraes DP, Sassi FC, Mangilli LD, Zilberstein B, de Andrade CR. Clinical prognostic indicators of dysphagia following prolonged orotracheal intubation in ICU patients. Crit Care. 2013;17(5):R243.
Zielske J, Bohne S, Brunkhorst FM, Axer H, Guntinas-Lichius O. Acute and long-term dysphagia in critically ill patients with severe sepsis: results of a prospective controlled observational study. Eur Arch Otorhinolaryngol. 2014;271(11):3085–93.
Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: a systematic review. Chest. 2010;137(3):665–73.
Schefold JC, Berger D, Zurcher P, Lensch M, Perren A, Jakob SM, Parviainen I, Takala J. Dysphagia in mechanically ventilated ICU patients (DYnAMICS): a prospective observational trial. Crit Care Med. 2017;45(12):2061–9.
Brodsky MB, Huang M, Shanholtz C, Mendez-Tellez PA, Palmer JB, Colantuoni E, Needham DM. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study. Ann Am Thorac Soc. 2017;14(3):376–83.
Christensen M, Trapl M. Development of a modified swallowing screening tool to manage post-extubation dysphagia. Nurs Crit Care. 2018;23(2):102-107. https://doi.org/10.1111/nicc.12333. Epub 2017 Dec 28..
Medeiros GC, Sassi FC, Zambom LS, Andrade CR. Correlation between the severity of critically ill patients and clinical predictors of bronchial aspiration. J Bras Pneumol. 2016;42(2):114–20.
Oliveira ACM, Friche AAL, Salomao MS, Bougo GC, Vicente LCC. Predictive factors for oropharyngeal dysphagia after prolonged orotracheal intubation. Braz J Otorhinolaryngol. 2018;84(6):722–28. https://doi.org/10.1016/j.bjorl.2017.08.010. Epub 2017 Sep 13.
Scheel R, Pisegna JM, McNally E, Noordzij JP, Langmore SE. Endoscopic assessment of swallowing after prolonged intubation in the ICU setting. Ann Otol Rhinol Laryngol. 2016;125(1):43–52.
See KC, Peng SY, Phua J, Sum CL, Concepcion J. Nurse-performed screening for postextubation dysphagia: a retrospective cohort study in critically ill medical patients. Crit Care. 2016;20(1):326.
Loeb M, McGeer A, McArthur M, Walter S, Simor AE. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med. 1999;159(17):2058–64.
Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124(1):328–36.
Martin BJ, Corlew MM, Wood H, Olson D, Golopol LA, Wingo M, Kirmani N. The association of swallowing dysfunction and aspiration pneumonia. Dysphagia. 1994;9(1):1–6.
Vergis EN, Brennen C, Wagener M, Muder RR. Pneumonia in long-term care: a prospective case-control study of risk factors and impact on survival. Arch Intern Med. 2001;161(19):2378–81.
Ajemian MS, Nirmul GB, Anderson MT, Zirlen DM, Kwasnik EM. Routine fiberoptic endoscopic evaluation of swallowing following prolonged intubation: implications for management. Archives Surgery (Chicago, Ill : 1960). 2001;136(4):434–7.
Barquist E, Brown M, Cohn S, Lundy D, Jackowski J. Postextubation fiberoptic endoscopic evaluation of swallowing after prolonged endotracheal intubation: a randomized, prospective trial. Crit Care Med. 2001;29(9):1710–3.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
El Solh A, Okada M, Bhat A, Pietrantoni C. Swallowing disorders post orotracheal intubation in the elderly. Intensive Care Med. 2003;29(9):1451–5.
Holas MA, DePippo KL, Reding MJ. Aspiration and relative risk of medical complications following stroke. Arch Neurol. 1994;51(10):1051–3.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665–71.
Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994;9(1):7–11.
Tolep K, Getch CL, Criner GJ. Swallowing dysfunction in patients receiving prolonged mechanical ventilation. Chest. 1996;109(1):167–72.
Ponfick M, Linden R, Nowak DA. Dysphagia--a common, transient symptom in critical illness polyneuropathy: a fiberoptic endoscopic evaluation of swallowing study*. Crit Care Med. 2015;43(2):365–72.
DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990;18(12):1328–30.
Daly E, Miles A, Scott S, Gillham M. Finding the red flags: swallowing difficulties after cardiac surgery in patients with prolonged intubation. J Crit Care. 2016;31(1):119–24.
Medeiros GC, Sassi FC, Mangilli LD, Zilberstein B, Andrade CR. Clinical dysphagia risk predictors after prolonged orotracheal intubation. Clinics. 2014;69(1):8–14.
Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010;136(8):784–9.
Barker J, Martino R, Reichardt B, Hickey EJ, Ralph-Edwards A. Incidence and impact of dysphagia in patients receiving prolonged endotracheal intubation after cardiac surgery. Can J Surg. 2009;52(2):119–24.
Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996;27(7):1200–4.
Brodsky MB, Gonzalez-Fernandez M, Mendez-Tellez PA, Shanholtz C, Palmer JB, Needham DM. Factors associated with swallowing assessment after oral endotracheal intubation and mechanical ventilation for acute lung injury. Ann Am Thorac Soc. 2014;11(10):1545–52.
Macht M, White SD, Moss M. Swallowing dysfunction after critical illness. Chest. 2014;146(6):1681–9.
Reiter R, Brosch S. Update oropharyngeal dysphagia part 1: physiology, pathology and diagnosis. Laryngorhinootologie. 2012;91(4):224–7.
Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, Diamant NE. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Phys. 1999;277(1 Pt 1):G219–25.
Hamdy S, Rothwell JC, Brooks DJ, Bailey D, Aziz Q, Thompson DG. Identification of the cerebral loci processing human swallowing with H2(15)O PET activation. J Neurophysiol. 1999;81(4):1917–26.
Riecker A, Gastl R, Kuhnlein P, Kassubek J, Prosiegel M. Dysphagia due to unilateral infarction in the vascular territory of the anterior insula. Dysphagia. 2009;24(1):114–8.
Kumar S. Swallowing and dysphagia in neurological disorders. Rev Neurol Dis. 2010;7(1):19–27.
Lang IM. Brain stem control of the phases of swallowing. Dysphagia. 2009;24(3):333–48.
Prosiegel M, Holing R, Heintze M, Wagner-Sonntag E, Wiseman K. The localization of central pattern generators for swallowing in humans--a clinical-anatomical study on patients with unilateral paresis of the vagal nerve, Avellis’ syndrome, Wallenberg’s syndrome, posterior fossa tumours and cerebellar hemorrhage. Acta Neurochir Suppl. 2005;93:85–8.
Lear CS, Flanagan JB Jr, Moorrees CF. The frequency of deglutition in man. Arch Oral Biol. 1965;10:83–100.
Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154(5):953–63.
Reiter R, Brosch S. Update oropharyngeal dysphagia part 2: etiology and therapy. Laryngorhinootologie. 2012;91(5):291–9.
Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of 150 critically ill adult patients. Am J Med. 1981;70(1):65–76.
Suiter DM, McCullough GH, Powell PW. Effects of cuff deflation and one-way tracheostomy speaking valve placement on swallow physiology. Dysphagia. 2003;18(4):284–92.
Terk AR, Leder SB, Burrell MI. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. 2007;22(2):89–93.
Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003;24(3):457–71.
Hong SJ, Lee JY. Isolated unilateral paralysis of the hypoglossal nerve after transoral intubation for general anesthesia. Dysphagia. 2009;24(3):354–6.
Bramer S, Koscielny S, Witte OW, Terborg C. Bilateral hypoglossal nerve palsy following intubation. Nervenarzt. 2006;77(2):204–7.
Batjom E, Coron T, Mercier F, Benhamou D. Hypoglossal nerve palsy, a rare complication of orotracheal intubation. Ann Fr Anesth Reanim. 2006;25(5):541–2.
Dziewas R, Ludemann P. Hypoglossal nerve palsy as complication of oral intubation, bronchoscopy and use of the laryngeal mask airway. Eur Neurol. 2002;47(4):239–43.
Schefold JC, Bierbrauer J, Weber-Carstens S. Intensive care unit-acquired weakness (ICUAW) and muscle wasting in critically ill patients with severe sepsis and septic shock. J Cachexia Sarcopenia Muscle. 2010;1(2):147–57.
Berger D, Bloechlinger S, von Haehling S, Doehner W, Takala J, Z'Graggen WJ, Schefold JC. Dysfunction of respiratory muscles in critically ill patients on the intensive care unit. J Cachexia Sarcopenia Muscle. 2016;7(4):403–12.
Jolley SE, Bunnell AE, Hough CL. ICU-acquired weakness. Chest. 2016;150(5):1129–40.
Goldsmith T. Evaluation and treatment of swallowing disorders following endotracheal intubation and tracheostomy. Int Anesthesiol Clin. 2000;38(3):219–42.
Feng X, Todd T, Lintzenich CR, Ding J, Carr JJ, Ge Y, Browne JD, Kritchevsky SB, Butler SG. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol A Biol Sci Med Sci. 2013;68(7):853–60.
Brodsky MB, De I, Chilukuri K, Huang M, Palmer JB, Needham DM. Coordination of pharyngeal and laryngeal swallowing events during single liquid swallows after Oral endotracheal intubation for patients with acute respiratory distress syndrome. Dysphagia. 2018;33(6):768–77.
Aviv JE. Clinical assessment of pharyngolaryngeal sensitivity. Am J Med. 2000;108(Suppl 4a):68S–72S.
Aviv JE, Spitzer J, Cohen M, Ma G, Belafsky P, Close LG. Laryngeal adductor reflex and pharyngeal squeeze as predictors of laryngeal penetration and aspiration. Laryngoscope. 2002;112(2):338–41.
Bradley RM. Sensory receptors of the larynx. Am J Med. 2000;108(Suppl 4a):47S–50S.
Shaker R, Hogan WJ. Reflex-mediated enhancement of airway protective mechanisms. Am J Med. 2000;108(Suppl 4a):8S–14S.
Leder SB, Suiter DM, Lisitano Warner H. Answering orientation questions and following single-step verbal commands: effect on aspiration status. Dysphagia. 2009;24(3):290–5.
Boden K, Cedborg AI, Eriksson LI, Hedstrom HW, Kuylenstierna R, Sundman E, Ekberg O. Swallowing and respiratory pattern in young healthy individuals recorded with high temporal resolution. Neurogastroenterol Motil. 2009;21(11):1163–e1101.
Perren A, Zurcher P, Schefold JC. Clinical approaches to assess post-extubation dysphagia (PED) in the critically ill. Dysphagia. 2019. https://doi.org/10.1007/s00455-019-09977-w.
Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, Moss M. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011;15(5):R231.
Bordon A, Bokhari R, Sperry J, Testa D, Feinstein A, Ghaemmaghami V. Swallowing dysfunction after prolonged intubation: analysis of risk factors in trauma patients. Am J Surg. 2011;202(6):679–82 discussion 682-673.
Ferraris VA, Ferraris SP, Moritz DM, Welch S. Oropharyngeal dysphagia after cardiac operations. Ann Thorac Surg. 2001;71(6):1792–5 discussion 1796.
Hogue CW Jr, Lappas GD, Creswell LL, Ferguson TB Jr, Sample M, Pugh D, Balfe D, Cox JL, Lappas DG. Swallowing dysfunction after cardiac operations. Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110(2):517–22.
Rousou JA, Tighe DA, Garb JL, Krasner H, Engelman RM, Flack JE 3rd, Deaton DW. Risk of dysphagia after transesophageal echocardiography during cardiac operations. Ann Thorac Surg. 2000;69(2):486–9 discussion 489-490.
Skoretz SA, Yau TM, Ivanov J, Granton JT, Martino R. Dysphagia and associated risk factors following extubation in cardiovascular surgical patients. Dysphagia. 2014;29(6):647–54.
de Larminat V, Montravers P, Dureuil B, Desmonts JM. Alteration in swallowing reflex after extubation in intensive care unit patients. Crit Care Med. 1995;23(3):486–90.
Leder SB, Cohn SM, Moller BA. Fiberoptic endoscopic documentation of the high incidence of aspiration following extubation in critically ill trauma patients. Dysphagia. 1998;13(4):208–12.
Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994;105(2):563–6.
Metheny NA, Clouse RE, Chang YH, Stewart BJ, Oliver DA, Kollef MH. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med. 2006;34(4):1007–15.
Omura K, Komine A, Yanagigawa M, Chiba N, Osada M. Frequency and outcome of post-extubation dysphagia using nurse-performed swallowing screening protocol. Nurs Crit Care. 2019;24(2):70–75. https://doi.org/10.1111/nicc.12359. Epub 2018 Jul 3..
Sassi FC, Medeiros GC, Zambon LS, Zilberstein B, Andrade CRF. Evaluation and classification of post-extubation dysphagia in critically ill patients. Rev Col Bras Cir. 2018;45(3):e1687.
Kim MJ, Park YH, Park YS, Song YH. Associations between prolonged intubation and developing post-extubation dysphagia and aspiration pneumonia in non-neurologic critically ill patients. Ann Rehabil Med. 2015;39(5):763–71.
Kwok AM, Davis JW, Cagle KM, Sue LP, Kaups KL. Post-extubation dysphagia in trauma patients: it's hard to swallow. Am J Surg. 2013;206(6):924–7 discussion 927-928.
Doggett DL, Tappe KA, Mitchell MD, Chapell R, Coates V, Turkelson CM. Prevention of pneumonia in elderly stroke patients by systematic diagnosis and treatment of dysphagia: an evidence-based comprehensive analysis of the literature. Dysphagia. 2001;16(4):279–95.
Teuschl Y, Trapl M, Ratajczak P, Matz K, Dachenhausen A, Brainin M. Systematic dysphagia screening and dietary modifications to reduce stroke-associated pneumonia rates in a stroke-unit. PLoS One. 2018;13(2):e0192142.
Marvin S, Thibeault S, Ehlenbach WJ: Post-extubation dysphagia: does timing of evaluation matter? Dysphagia. 2019;34(2):210–19. https://doi.org/10.1007/s00455-018-9926-3. Epub 2018 Jul 24.
Lynch YT, Clark BJ, Macht M, White SD, Taylor H, Wimbish T, Moss M. The accuracy of the bedside swallowing evaluation for detecting aspiration in survivors of acute respiratory failure. J Crit Care. 2017;39:143–8.
Clave P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27(6):806–15.
Antonios N, Carnaby-Mann G, Crary M, Miller L, Hubbard H, Hood K, Sambandam R, Xavier A, Silliman S. Analysis of a physician tool for evaluating dysphagia on an inpatient stroke unit: the modified Mann Assessment of Swallowing Ability. J Stroke Cerebrovasc Dis. 2010;19(1):49–57.
Carnaby GD, Crary MA. Development and validation of a cancer-specific swallowing assessment tool: MASA-C. Support Care Cancer. 2014;22(3):595–602.
Gonzalez-Fernandez M, Sein MT, Palmer JB. Clinical experience using the Mann assessment of swallowing ability for identification of patients at risk for aspiration in a mixed-disease population. Am J Speech-Lang Pathol. 2011;20(4):331–6.
Oh JC, Park JH, Jung MY, Yoo EY, Chang KY, Lee TY. Relationship between quantified instrumental swallowing examination and comprehensive clinical swallowing examination. Occup Ther Int. 2016;23(1):3–10.
Hansen T, Lambert HC, Faber J. Validation of the Danish version of the McGill Ingestive Skills Assessment using classical test theory and the Rasch model. Disabil Rehabil. 2012;34(10):859–68.
Lambert HC, Gisel EG, Groher ME, Abrahamowicz M, Wood-Dauphinee S. Psychometric testing of the McGill Ingestive Skills Assessment. Am J Occup Ther. 2006;60(4):409–19.
Trapl M, Enderle P, Nowotny M, Teuschl Y, Matz K, Dachenhausen A, Brainin M. Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke. 2007;38(11):2948–52.
Logemann JA, Veis S, Colangelo L. A screening procedure for oropharyngeal dysphagia. Dysphagia. 1999;14(1):44–51.
Sheppard JJ, Hochman R, Baer C. The dysphagia disorder survey: validation of an assessment for swallowing and feeding function in developmental disability. Res Dev Disabil. 2014;35(5):929–42.
Zhou Z, Salle J, Daviet J, Stuit A, Nguyen C. Combined approach in bedside assessment of aspiration risk post stroke: PASS. Eur J Phys Rehabil Med. 2011;47(3):441–6.
Maeda K, Shamoto H, Wakabayashi H, Enomoto J, Takeichi M, Koyama T. Reliability and validity of a simplified comprehensive assessment tool for feeding support: Kuchi-Kara Taberu Index. J Am Geriatr Soc. 2016;64(12):e248–52.
Lee KM, Kim HJ. Practical assessment of dysphagia in stroke patients. Ann Rehabil Med. 2015;39(6):1018–27.
Hacki T, Kramer H, Kleinjung C, Perez-Alvarez C, Schmid J. Endoscopic multi-color deglutition study. Laryngorhinootologie. 2001;80(6):335–40.
Aviv JE, Kaplan ST, Thomson JE, Spitzer J, Diamond B, Close LG. The safety of flexible endoscopic evaluation of swallowing with sensory testing (FEESST): an analysis of 500 consecutive evaluations. Dysphagia. 2000;15(1):39–44.
Schindler A, Ginocchio D, Peri A, Felisati G, Ottaviani F. FEESST in the rehabilitation of dysphagia after partial laryngectomy. Ann Otol Rhinol Laryngol. 2010;119(2):71–6.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Hannig C, Wuttge-Hannig A, Hess U. Analysis and radiologic staging of the type and severity of aspiration. Radiologe. 1995;35(10):741–6.
Palmer JB, Kuhlemeier KV, Tippett DC, Lynch C. A protocol for the videofluorographic swallowing study. Dysphagia. 1993;8(3):209–14.
Fanucci A, Cerro P, Ietto F, Brancaleone C, Berardi F. Physiology of oral swallowing studied by ultrasonography. Dentomaxillofac Radiol. 1994;23(4):221–5.
Manabe N, Haruma K, Nakato R, Kusunoki H, Kamada T, Hata J. New ultrasonographic screening method for oropharyngeal dysphagia: tissue Doppler imaging. Am J Physiol Gastrointest Liver Physiol. 2018;314(1):G32–8.
Castell JA, Castell DO. Modern solid state computerized manometry of the pharyngoesophageal segment. Dysphagia. 1993;8(3):270–5.
Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, Hogan WJ. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989;4(1):8–15.
Dodds WJ, Hogan WJ, Lydon SB, Stewart ET, Stef JJ, Arndorfer RC. Quantitation of pharyngeal motor function in normal human subjects. J Appl Physiol. 1975;39(4):692–6.
Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154(5):965–74.
McConnel FM. Analysis of pressure generation and bolus transit during pharyngeal swallowing. Laryngoscope. 1988;98(1):71–8.
Fattori B, Grosso M, Bongioanni P, Nacci A, Cristofani R, AlSharif A, Licitra R, Matteucci F, Rossi B, Rubello D, et al. Assessment of swallowing by oropharyngoesophageal scintigraphy in patients with amyotrophic lateral sclerosis. Dysphagia. 2006;21(4):280–6.
Kozlow JH, Berenholtz SM, Garrett E, Dorman T, Pronovost PJ. Epidemiology and impact of aspiration pneumonia in patients undergoing surgery in Maryland, 1999–2000. Crit Care Med. 2003;31(7):1930–7.
Rassameehiran S, Klomjit S, Mankongpaisarnrung C, Rakvit A. Postextubation dysphagia. Proc (Bayl Univ Med Cent). 2015;28(1):18–20.
Hirst LJ, Sama A, Carding PN, Wilson JA. Is a ‘safe swallow’ really safe? Int J Lang Commun Disord. 1998;33(Suppl):279–80.
Ohmae Y, Logemann JA, Kaiser P, Hanson DG, Kahrilas PJ. Effects of two breath-holding maneuvers on oropharyngeal swallow. Ann Otol Rhinol Laryngol. 1996;105(2):123–31.
Kahrilas PJ, Logemann JA, Krugler C, Flanagan E. Volitional augmentation of upper esophageal sphincter opening during swallowing. Am J Phys. 1991;260(3 Pt 1):G450–6.
Logemann JA. Treatment of oral and pharyngeal dysphagia. Phys Med Rehabil Clin N Am. 2008;19(4):803–16 ix.
Shanahan TK, Logemann JA, Rademaker AW, Pauloski BR, Kahrilas PJ. Chin-down posture effect on aspiration in dysphagic patients. Arch Phys Med Rehabil. 1993;74(7):736–9.
Welch MV, Logemann JA, Rademaker AW, Kahrilas PJ. Changes in pharyngeal dimensions effected by chin tuck. Arch Phys Med Rehabil. 1993;74(2):178–81.
Logemann JA, Kahrilas PJ, Kobara M, Vakil NB. The benefit of head rotation on pharyngoesophageal dysphagia. Arch Phys Med Rehabil. 1989;70(10):767–71.
Prosiegel M, Heintze M, Wagner-Sonntag E, Hannig C, Wuttge-Hannig A, Yassouridis A. Deglutition disorders in neurological patients. A prospective study of diagnosis, pattern of impairment, therapy and outcome. Nervenarzt. 2002;73(4):364–70.
Carnaby G, Hankey GJ, Pizzi J. Behavioural intervention for dysphagia in acute stroke: a randomised controlled trial. Lancet Neurol. 2006;5(1):31–7.
Kos MP, David EF, Klinkenberg-Knol EC, Mahieu HF. Long-term results of external upper esophageal sphincter myotomy for oropharyngeal dysphagia. Dysphagia. 2010;25(3):169–76.
Shama L, Connor NP, Ciucci MR, McCulloch TM. Surgical treatment of dysphagia. Phys Med Rehabil Clin N Am. 2008;19(4):817–35 ix.
Flint PW, Purcell LL, Cummings CW. Pathophysiology and indications for medialization thyroplasty in patients with dysphagia and aspiration. Otolaryngol Head Neck Surg. 1997;116(3):349–54.
Muhle P, Claus I, Marian T, Schroder JB, Wollbrink A, Pantev C, Warnecke T, Dziewas R, Suntrup-Krueger S. Introducing a virtual lesion model of dysphagia resulting from pharyngeal sensory impairment. Neurosignals. 2018;26(1):1–10.
Teismann IK, Steinstraeter O, Stoeckigt K, Suntrup S, Wollbrink A, Pantev C, Dziewas R. Functional oropharyngeal sensory disruption interferes with the cortical control of swallowing. BMC Neurosci. 2007;8:62.
Hamdy S, Rothwell JC, Aziz Q, Singh KD, Thompson DG. Long-term reorganization of human motor cortex driven by short-term sensory stimulation. Nat Neurosci. 1998;1(1):64–8.
Suntrup S, Marian T, Schroder JB, Suttrup I, Muhle P, Oelenberg S, Hamacher C, Minnerup J, Warnecke T, Dziewas R. Electrical pharyngeal stimulation for dysphagia treatment in tracheotomized stroke patients: a randomized controlled trial. Intensive Care Med. 2015;41(9):1629–37.
Jayasekeran V, Singh S, Tyrrell P, Michou E, Jefferson S, Mistry S, Gamble E, Rothwell J, Thompson D, Hamdy S. Adjunctive functional pharyngeal electrical stimulation reverses swallowing disability after brain lesions. Gastroenterology. 2010;138(5):1737–46.
Imoto Y, Kojima A, Osawa Y, Sunaga H, Fujieda S. Cough reflex induced by capsaicin inhalation in patients with dysphagia. Acta Otolaryngol. 2011;131(1):96–100.
Jin Y, Sekizawa K, Fukushima T, Morikawa M, Nakazawa H, Sasaki H. Capsaicin desensitization inhibits swallowing reflex in guinea pigs. Am J Respir Crit Care Med. 1994;149(1):261–3.
Nakagawa T, Ohrui T, Sekizawa K, Sasaki H. Sputum substance P in aspiration pneumonia. Lancet. 1995;345(8962):1447.
Suntrup-Krueger S, Bittner S, Recker S, Meuth SG, Warnecke T, Suttrup I, Marian T, Dziewas R. Electrical pharyngeal stimulation increases substance P level in saliva. Neurogastroenterol Motil. 2016;28(6):855–60.
Dziewas R, Mistry S, Hamdy S, Minnerup J, Van Der Tweel I, Schabitz W, Bath PM, Investigators P-T. Design and implementation of Pharyngeal electrical Stimulation for early de-cannulation in TRACheotomized (PHAST-TRAC) stroke patients with neurogenic dysphagia: a prospective randomized single-blinded interventional study. Int J Stroke. 2017;12(4):430–7.
Dziewas R, Stellato R, van der Tweel I, Walther E, Werner CJ, Braun T, Citerio G, Jandl M, Friedrichs M, Notzel K, et al. Pharyngeal electrical stimulation for early decannulation in tracheotomised patients with neurogenic dysphagia after stroke (PHAST-TRAC): a prospective, single-blinded, randomised trial. Lancet Neurol. 2018;17(10):849–59.
Marian T, Dunser M, Citerio G, Kokofer A, Dziewas R. Are intensive care physicians aware of dysphagia? The MAD(ICU) survey results. Intensive Care Med. 2018;44(6):973–5.
van Snippenburg W, Kroner A, Flim M, Hofhuis J, Buise M, Hemler R, Spronk P. Awareness and management of dysphagia in Dutch intensive care units: a nationwide survey. Dysphagia. 2019;34(2):220–28. https://doi.org/10.1007/s00455-018-9930-7. Epub 2018 Aug 1.
Dziewas R, Glahn J. Dysphagiemanagement, in: Stefan Schwab, Peter Schellinger, Andreas Unterberger, Christian Werner, Werner Hacker (Hrsg), NeuroIntensiv, 3. Auflage, Springer Verlag, Berlin, Heidelberg. 2015. p. 108–14.
PanEuropean Networks; Science technology (24) 65: firing up the swallowing network, 188–89. Copyright Heike Blum, Department of Neurology, University Hospital Münster, Germany
Acknowledgements
Not applicable.
Funding
No funding applies
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the literature search, drafted the article, and contributed to important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Drs. Zuercher, Moret, and Schefold declare that the Department of Intensive Care Medicine, Inselspital, Bern, has received research or other grants from (full disclosure) Orion Pharma, Abbott Nutrition International, B. Braun Medical AG, CSEM AG, Edwards Lifesciences Services GmbH, Kenta Biotech Ltd., Maquet Critical Care AB, Omnicare Clinical Research AG, Nestle, Pierre Fabre Pharma AG, Pfizer, Bard Medica S.A., Abbott AG, Anandic Medical Systems, Pan Gas AG Healthcare, Bracco, Hamilton Medical AG, Fresenius Kabi, Getinge Group Maquet AG, Dräger AG, Teleflex Medical GmbH, Glaxo Smith Kline, Merck Sharp and Dohme AG, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, and Nycomed outside the submitted work. The money was paid into departmental funds. No personal financial gain applies. Dr. Dziewas declares no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zuercher, P., Moret, C.S., Dziewas, R. et al. Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Crit Care 23, 103 (2019). https://doi.org/10.1186/s13054-019-2400-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-019-2400-2