Abstract
The transport of bicarbonate across the enterocyte cell membrane regulates the intracellular as well as the luminal pH and is an essential part of directional fluid movement in the gut. Since the first description of “active” transport of HCO3− ions against a concentration gradient in the 1970s, the fundamental role of HCO3− transport for multiple intestinal functions has been recognized. The ion transport proteins have been identified and molecularly characterized, and knockout mouse models have given insight into their individual role in a variety of functions. This review describes the progress made in the last decade regarding novel techniques and new findings in the molecular regulation of intestinal HCO3− transport in the different segments of the gut. We discuss human diseases with defects in intestinal HCO3− secretion and potential treatment strategies to increase luminal alkalinity. In the last part of the review, the cellular and organismal mechanisms for acid/base sensing in the intestinal tract are highlighted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Historical perspective
Scientists recognized more than a century ago that the gastric mucosa does secrete not just acidic but also alkaline fluids, both of which could be stimulated [125]. The interrelatedness of high gastric acidity and a protective alkaline “Verdünnungsflüssigkeit,” an alkaline diluent, was also recognized and its origins were hotly debated at the beginning of the last century [14]. More detailed studies of gastrointestinal bicarbonate transport started in the 1970s, after the development of a technique that combined electrophysiological investigations of epithelia in Ussing chambers with pH–stat microtitration techniques to record the rates of proton or base output into the luminal fluid [46, 47, 62]. Another groundbreaking technique was the intestinal perfusion technique, which permitted the perfusion of a segment of the intestine with defined solutions via separate inflow and outflow catheters, isolated from the other parts of the bowel by inflatable balloons, both in laboratory animals and in man [48]. This technique allowed the formulation of the hypotheses that the human jejunum combines fluid absorption with bicarbonate absorption by a parallel operation of electroneutral Na+/H+ exchange with Cl−/HCO3− exchange in the brush border membrane [175]. Regional differences in the ratios of the activities of the two types of exchangers could explain proton secretion in the jejunum, in which the rate of Na+/H+ exchange exceeds that of Cl−/HCO3− exchange, and bicarbonate secretion in the ileum, in which the rate of Cl−/HCO3− exchange exceeds that of rate of Na+/H+ exchange [10].
A similar technique was used to study the response of the human duodenum upon contact of the mucosa with luminal acid. It was shown that patients who had developed duodenal ulcer disease displayed a reduced HCO3− secretory response to a contact of the duodenal mucosa with acid, even after the ulcers had been healed by pharmacological inhibition of gastric acid secretion [74]. Although these results were under debate at a time when it became clear that a very high percentage of patients with duodenal ulcer disease harbored a chronic infection with Helicobacter pylori in their antrum [69, 109], it is now clear that the findings were likely due to the gastric metaplasia in the duodenum [16]. This metaplasia is caused by chronic hypersecretion of gastric acid, secondary to the destruction of the complex and finely regulated feedback inhibition of high gastric acidity in the antrum by the Helicobacter pylori–induced low-grade antral inflammation [16]. Indeed, the same group showed a decade later that after pH eradication and mucosal healing, the duodenal HCO3− secretory response to acid was normalized in former duodenal ulcer patients [63].
In the last century, the study of molecular mechanisms and physiological regulation of intestinal HCO3− secretion focused on the upper gastrointestinal (GI) tract, while mechanisms of fluid secretion and absorption were studied in the lower GI tract. Only a few studies addressed the role of an alkaline micromilieu for the restitution of the colonic mucosa after injury [45, 130]. Therefore, it was not realized for a long time that the rates of HCO3− output in the colon are far higher than those in the duodenum [12]. The physiological significance of these high colonic HCO3− output rates is not limited to Cl− reabsorption from the lumen but also plays an important role in the luminal pH-maintenance during bacterial fermentation, because the generated fermentation products (short-chain fatty acids (SCFA), ammonia/ammonium ions, and carbonic acid/CO2) need to be neutralized [11, 163]. Because of the decreasing incidence and better manageability of gastric and duodenal ulcer disease, in parallel to an increased incidence and severity, as well as more treatment resistance, of inflammatory bowel diseases (IBD), the interest has recently shifted and more studies on alkaline output and the involved transport and regulatory mechanisms have been performed in the ileocolon, which will be discussed later. Another area of intense research became the defective HCO3− transport in the epithelia of patients with cystic fibrosis [98].
Classic techniques and recent technological advances for the study of intestinal HCO3 − transport
More than 10 years ago, a review has carefully described the techniques which were then available to measure cystic fibrosis transmembrane conductance regulator (CFTR)–dependent HCO3− transport, which was the most interesting aspect of alkaline output for scientists involved in research related to cystic fibrosis [72]. Another review published at that time addressed the novel techniques that had increased the armamentarium to study HCO3− transport in transgenic mice. Major advances have been made in the assessment of surface epithelial function using video-imaging and two-photon techniques to assess the intracellular and juxtamucosal pH in anesthetized rodents and isolated tissues using dye methods, and combine microelectrode techniques, laser Doppler flow, and optical techniques to simultaneously assess blood flow, pH, and mucus layer buildup. In addition, the techniques to determine alkalinization rates of different segments of the murine gastrointestinal tract and of organs that secrete alkaline fluids into the digestive tract have become more sophisticated, in part due to miniaturization of equipment to keep a perfect systemic blood pressure and acid/base control in anesthetized transgenic mice [144].
During the last decade, three novel developments have revolutionized the way how we are studying HCO3− transport processes: The first is an ability to preserve the intestinal stem cells that are present in the cryptal region, to generate intestinal epithelium from these stem cells, and to differentiate the epithelium in a segmental organotypic fashion [34, 140, 169]. The second is the elucidation of all components of the “gene scissor” CRISPR-Cas9 prokaryote immune defense system [83] and to optimize its applicability for the use in mammalian cells [31, 84, 107]. The third technical advance is the ability to continuously measure the pH directly at the apical surface of a cell monolayer and thus investigate acid/base flux via the apical membrane (although flux rates cannot be exactly quantitated) [135]. A combination of these techniques may allow a much better delineation of the importance, transport mode, and regulation of the individual HCO3− transporters expressed along the crypt-villus axis, particularly in the human GI tract.
Current understanding of bicarbonate transport in the different segments of the gastrointestinal tract
To the knowledge of the authors, no previously unrecognized HCO3− transporters have been described in intestinal tissues in the last decade. Since a number of excellent recent reviews have recently been published that describe the transport mode of individual HCO3− transport proteins in detail, we will focus on the physiological significance of individual HCO3− transporters, on their interplay with other transporters, and on intervention strategies to improve pathological HCO3− transport dysfunction. Because of the multitude of investigations, this review will focus on information obtained in mice and where available in human tissue.
Basal luminal alkalinization rates in the different intestinal segments
The alkalinization rates of different segments of isolated and chambered murine intestinal mucosa are very different, with particularly low rates in the jejunum and proximal colon and particularly high rates in the cecum and mid-distal colon [89, 196]. The same pattern is observed when the different segments are perfused with an unbuffered electrolyte solution of neutral pH in anesthetized mice. In the distal intestine, the basal alkalinization rates in the different segments correspond well with the expression levels of the luminal Cl−/HCO3− exchanger Slc26a3 [165] and are only minimally reduced in the absence of CFTR [196]. In the proximal intestine, basal alkalinization rates are 3–fourfold lower than in the mid-distal intestine and are reduced in the absence of CFTR [146, 196], Slc26a3 (DRA) [157, 182], and to a lesser extent of Slc26a6 (PAT-1) [185]. These results are similar in vitro and in vivo, and they only apply for a situation with unbuffered luminal saline or Ringer’s solution.
Effect of nutrients on basal alkalinization
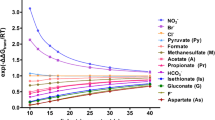
The situation changes when nutrients are present in the luminal perfusate. The addition of glucose to the luminal bath of chambered small intestine results not only in a strong increase of Na+ and fluid absorption but also in a decrease in alkalinization rates in vitro [146], as well as a decrease in the jejunal pH-microclimate in vivo. Among other mechanisms, the intracellular utilization of glucose generates acidic moieties that leave the cell via luminal Na+/H+ exchangers [33, 102]. The addition of short-chain fatty acids (SCFA), which are important nutrients for the colonocyte, to the colonic mucosa is associated with an increase in HCO3− output [7, 176]. The explanations for this phenomenon varied widely, including the postulation of a SCFA/HCO3− exchanger in the luminal membrane [178]. We now know that monocarboxylate transporters which are either proton coupled (MCT1) or sodium coupled (SMCT1) are expressed in the apical membranes of colonocytes and that SCFA can also transverse the apical membrane in a non-dissociated form when the luminal pH is low [160]. The cotransport of SCFA with H+ via MCT1 (likely the predominant transport protein for SCFA [115]) will result in a removal of protons from the lumen, which is equivalent with an alkalinization. In addition, MCT1-mediated SCFA absorption will acidify the colonocyte, resulting in a stimulation of the apical NHE3 and thus Na+ and fluid absorption. However, because SCFA anions are cotransported with protons via MCT1 and MCT4 in the basolateral membrane into the blood stream, the apical proton recycling via NHE3 does not match the rate of proton disappearance from the lumen, and a luminal alkalinization is observed. In line with the predominant site of microbiome-mediated SCFA production in the proximal colon, both MCT1 and NHE3 are strongly expressed in the mucosa of the proximal colon, both in mice and humans, whereas Slc26a3 is weakly expressed [145, 160]. This results in low alkalinization rates in the presence of luminal saline but high rates in the presence of luminal SCFA anions [178]. These are just two examples how the presence of nutrients in the lumen may completely change the alkalinization rates both in vivo and in vitro.
Secretagogue-stimulated intestinal HCO3 − secretion
In the intestine, the CFTR anion channel remains the most important, if not the only, conductive pathway for HCO3− exit under agonist-stimulated conditions. If heterologously expressed, the HCO3− conductivity of CFTR is only approximately one-fifth of that for Cl− under maximal electrochemical gradients [126, 168]. Recent data have shown how the CFTR channel may switch from a predominantly Cl−-conductive to an HCO3−-conductive channel through the activation of WNK (with-no-lysine) kinase and the phosphorylation of the downstream kinases SPAK and OSR1 in pancreatic ducts cells [123]. WNK signaling is activated when the intracellular Cl− concentration falls to low levels [91]. In the distal pancreatic ducts of guinea pigs (and possibly humans as well), this is a likely scenario during secretin-stimulated pancreatic juice secretion, because the ductal cells express low levels of basolateral NKCC1, which is a major Cl− importer during stimulated anion secretion [200]. In murine duodenum, phosphorylated SPAK and OSR1 are very abundant [196], which may be one reason why, even without exogenous stimulation, the percentage of HCO3− secretion that is dependent on luminal Cl− (and therefore presumably mediated by Cl−/HCO3− exchange) is much lower than in the murine colon, and the percentage that is dependent on CFTR expression is high [155]. A capsule pH-metry in CF patients displayed a strong difference in the neutralization capacity of the proximal but not the distal intestine [53]. A CFTR-targeted therapy significantly improved the acid-neutralizing capacity of the proximal intestine [54]. The regulation of the CFTR channel by hormonal, neural, and luminal agonists and endogenous inhibitors is complex and not the topic of this review.
Another mode of CFTR-dependent, agonist-stimulated HCO3− secretion is a functional interaction between the agonist-activated CFTR Cl− conductance and an apical Cl−/HCO3− exchanger, which recycles the luminal Cl− in exchange for HCO3− [44, 71, 101]. For this coupling mechanism to become operative, the two transporters need to be coexpressed in the apical membrane of the same cell type, a requirement for apical Cl− recycling, rather than rapid import of Cl− via the basolateral membrane needs to exist, and an ample supply of HCO3− to the cell needs to be present. All these requirements appear to be met in the proximal pancreatic duct cells, which coexpress CFTR and SLC26a6 in the apical membrane [76, 186] and have high expression levels for the basolateral Na+/HCO3− cotransporter NBCe1 [201] and low expression of the basolateral AE2, which would export HCO3− in exchange for Cl− and therefore lower the availability of intracellular HCO3− for apical exchange [133].
In the intestine, the situation is different, because the expression of CFTR and NKCC1 is strongly crypt predominant, and that of NBCe1 and the apical SLC26 anion exchangers is villus/surface predominant [78, 79, 152, 185]. An area of overlapping expression along the crypt/villus (surface) axis is necessary for CFTR-dependent HCO3− secretion via apical Cl− recycling. Because of insecurities with antibody specificity, technical issues, and species differences, the literature is equivocal regarding the expression pattern and the relevance for agonist-induced HCO3− secretion for either of the three SLC26 members expressed in the duodenum, namely, SLC26A3 (DRA), SLC26A6 (PAT-1), and SLC26A9 as well as of CFTR. While most publications report a crucial role for a functional CFTR in cAMP-, cGMP-, and Ca2+-dependent stimulation of duodenal HCO3− secretion in vitro [30, 64, 146] and in vivo [64, 65, 155], some reports found only a minor or minimal role [139, 149]. The reason for these discrepancies might be due to technical issues. There is indeed an agonist-mediated pathway of luminal alkalinization that is independent of CFTR expression and operates in murine as well as human intestine: The agonist-induced inhibition of apical proton extrusion mechanisms such as the Na+/H+ exchanger isoform NHE3, which is highly expressed in the brush border membrane of most intestinal segments except the distal colon, or of the distally expressed colonic H+/K+ ATPase will result in a CFTR-independent increase in luminal alkalinization in the presence of a highly expressed and cAMP-insensitive SLC26A3 [145, 166]. It has also been suggested that SLC26A3 may traffic to the brush border membrane in a cAMP-dependent but CFTR-independent fashion [172].
Role of SLC26A6 in intestinal HCO3 − secretion
Slc26a6 is strongly expressed in the proximal intestinal tract, with a gradient towards much lower expression in the colon [184]. If the expression levels are compared in the same sample of laser-dissected mucosal cells, mRNA expression of Slc26a6 is somewhat higher in the adult murine villous area from the duodenum than that of SLC26a3 expression, and both transporters are expressed in a villous-predominant fashion [103]. In the suckling murine intestinal mucosa, Slc26a6 mRNA expression levels were lower than for Slc26a3 in all small intestinal segments [205]. Slc26a6 is discussed as an electrogenic transporter, exporting two HCO3− ions and importing one Cl− ion [75, 82, 119, 131]. Other reports find evidence for an electroneutral Cl−/HCO3− exchange [4, 26, 183].
When slc26a6−/− and WT chambered duodenal mucosae were compared in Ussing chambers and the HCO3− secretion rate into a CO2/HCO3− free luminal electrolyte solution was measured (which offers a perfect driving force for a 2 HCO3−out/1 Cl−in exchange), a contribution of Slc26a6 for luminal alkalinization was observed, but the relative importance was less than expected, since the majority of basal and cAMP-dependent HCO3− secretion was preserved in the absence of Slc26a6 expression [173, 185]. Interestingly, Slc26a6 is involved in fluid absorption in isolated jejunal mucosa [148] and in anesthetized mice [156, 195]. In addition, Slc26a6 was shown to mediate HCO3− import during PEPT-1 mediated enterocyte acidification [153]. Another study demonstrated that the role Slc26a6 in basal and stimulated duodenal HCO3− secretion was dependent on the systemic acid/base status of the anesthetized mice [155]. Therefore, while the role of Slc26a6 in small intestinal oxalate secretion is well established [49, 50, 94], its exact physiological function as an intestinal HCO3− transporter is less clear.
Role of SLC26A3 in intestinal HCO3 − transport
SLC26A3 was one of the first members of the gene family whose molecular sequence was identified during a screening of a subtraction cDNA library constructed from colonic normal epithelium and adenomatous and cancer tissue and named downregulated in adenoma (DRA) [142]. A group of Finnish geneticists had narrowed the chromosomal location of the presumed gene that was defective in the rare hereditary chloride-losing diarrhea (CLD) to a narrow locus [90], and this enabled them to rapidly identify the DRA gene locus as the locus for all mutations know so far known in CLD [66]. This quickly established its potential role as the gene encoding for a luminal Cl−/HCO3− exchanger, hypothesized to be defective in CLD [174]. However, it took several more years until the transporter was functionally identified to be a bona fide Cl−/HCO3− transporter [100, 113, 114]. Its stoichiometry is still debated: Some reports suggest an electrogenic 2 Cl−i/1 HCO3−o exchange [151], while others suggest an electroneutral exchange [5, 100].
A slc26a3−/− mouse model was established, which recapitulated many features of CLD in humans [143]. Massive hyperaldosteronism and its sequelae were reported, namely, the strong upregulation of the Na+/H+ exchanger NHE3 and the epithelial Na+ channel ENaC in the colon of slc26a3−/− mice. However, this rescue mechanism may be less effective than originally thought, because the mid-distal colon of these mice did not absorb fluid [198]. The likely reason is that the acidic luminal and stool pH of these mice [92] inhibits apical Na+i/H+o exchange due to the high affinity of protons to the external binding site of the transporter. When the luminal pH is buffered to 7.4, the slc26a3−/− mid-distal colon is able to absorb fluid at approx. 50% of the rate seen in WT littermates ([166] and unpublished observations).
The slc26a3−/− mice have extremely low colonic luminal alkalinization rates [198] and a very acidic surface pH and develop a mild distal colitis over time [92]. This feature is interesting because CLD patients also have a high incidence of inflammatory bowel disease [117, 189]. A search for potential underlying mechanisms included a lack of an adherent mucus layer [198] as well as alterations in mucus formation and release [92], a dysbiotic microbiome [92, 93], a reciprocal cellular expression and action of TNFα and SLC26A3 [41], and disturbances of tight junction regulation [97, 207]. An interesting recent finding was a very strong upregulation of the expression of several classes of antimicrobial peptides in the slc26a3−/− colonic mucosa, which may in part explain the surprisingly mild inflammation in the slc26a3−/− colon, which occurs late in life, despite mucus abnormalities and dysbiosis from shortly after birth [92, 93]. However, a recent investigation reported a proinflammatory effect of an overproduction of Reg3, one of the antimicrobial proteins strongly upregulated in slc26a3−/− colonic mucosa [93], via a reduction in Enterococcus species that were protective in C57B/6 mice against DSS-induced colonic inflammation [80]. Enterococcus species were not abundant, and not different between genotypes, in the microbiota in our slc26a3−/− and WT mouse cohort (also C57B/6 background). This demonstrates how mouse house-associated factors may impact the outcome of research related to the highly complex pathophysiology of intestinal inflammation.
Effect of basolateral HCO3 − transporting mechanisms on basal and stimulated alkalinization rates
Early studies in chambered amphibian duodenum noticed that luminal alkalinization required the presence of physiological concentrations of Na+ and HCO3− in the serosal bath [154]. In the rabbit duodenum, neither the specific inhibition of the basolateral Na+/H+ exchanger NHE1 nor of a Na+/HCO3− cotransporter had a significant effect on basal or stimulated HCO3− secretion, but the combined inhibition of both pathways effectively reduced the alkalinization rate [77]. The contribution of the electroneutral Na+/HCO3− cotransporter NBCn1 (SLC4A7) to duodenal HCO3− secretion was confirmed by studying cAMP-dependent duodenal HCO3− secretion in vitro [24] as well as luminal acid–induced HCO3− secretory response in vivo [158] in slc4a7−/− mice. NBCn1 is relatively DIDS-insensitive [27, 132] and was found to be expressed in the murine and human duodenum [13, 32]. To study an involvement of the electrogenic NBCe1 in intestinal HCO3− secretion proved very difficult, because the mice die during weaning [52]. Although they display reduced HCO3− import into enterocytes in response to nutrient- or electrolyte transport–induced acid loads and a decreased basal alkalinization rate in the small, but not the large intestine, as well as a reduced anion and fluid secretory response to cAMP stimulation, the cAMP-induced HCO3− secretory response was not different between the small intestinal and colonic mucosa of the suckling slc4a4−/− and WT littermates [205]. It was noticed in that study that the HCO3− uptake rates into the surface colonocytes, but not into colonocytes in the cryptal base, were significantly reduced in slc4a4−/− compared to WT mice, whereas the opposite was found for surface and cryptal base colonocytes of slc4a7−/− mice. This suggested that there may a differential expression of the two NBCs along the cryptal axis and therefore a differential effect of their deletion on basal vs cAMP-induced HCO3− secretion. A recent study in human colonic organoids confirmed the strong expression of the electroneutral NBCn1, together with other components of the anion secretory machinery, namely, CFTR, NKCC1, TMEM16a, and AE2, in the non-differentiated, proliferative enteroids, with a strong downregulation of their expression during differentiation [136]. In contrast, the electrogenic NBCe1 was upregulated during differentiation. This also makes sense functionally, because a cAMP-induced opening of basolateral K+ channels, which increases the electrochemical gradient for apical anion secretion, at the same time, reduces the electrochemical gradient for NBCe1-mediated HCO3− import, while it does not affect that for NBCn1. Thus, NBCn1 may play an important role for agonist-induced CFTR-dependent HCO3− secretion and may augment the NKCC1-independent AE2-dependent Cl− import into colonic crypts [141]. In contrast, the cellular acidification mediated by H+-coupled dipeptide, by H+-coupled short-chain fatty acid anion import, or by apical Cl−/HCO3− exchange in the surface cells either depolarizes the membrane potential or does not affect it, permitting electrogenic 1 Na+/2 HCO3− import (Fig. 1).
Differential expression of the acid/base transporters along the human colonic cryptal axis. As deduced from studies in proliferating and differentiated human colonic enteroids, in situ hybridization, immunohistochemical staining, and fluorometric pHi-measurements, the acid/base transporters are differentially expressed along the cryptal axis. The ion transport machinery for electrogenic anion secretion, with the lead components CFTR and NKCC1, is coexpressed with AE2, NBCn1, and TMEM16a in the highly proliferative lower cryptal region and strongly downregulated during enterocyte differentiation. In contrast, the acid/base transporters SLC26a3, NHE3, and NBCe1 and the colonic H+/K+ ATPase, together with the ENaC subunits, are upregulated in the differentiated absorptive enterocytes. The intracellular pH is more acidic in the cryptal region than in the surface enterocytes. The full names of the abbreviations can be found in the manuscript
Strategies to influence luminal alkalinity in patients with defects in intestinal HCO3 − transport
Cystic fibrosis
Patients with cystic fibrosis have traditionally been treated with laxatives to prevent recurrent obstructive episodes and with agents that inhibit acid secretion to mitigate reflux symptoms and optimize digestion. These suboptimal strategies to improve CF-associated intestinal disease are now being successfully replaced by CFTR targeted therapy which improves not only the pulmonary but also the intestinal symptoms [54, 88, 112]. Preliminary results suggest that this improvement is not reached via an alteration of the dysbiotic gut microbiota seen in patients with CF [108]. Recent studies in CFTR null mice aimed to explore strategies to increase the alkalinity and fluidity in an intestine that expressed no functional CFTR protein at all and therefore is not a candidate for CFTR-targeted therapy. Indeed, several FDA-approved agents were identified that increased the luminal alkalinity and reduced small and in part also large intestinal fluid absorptive rate [166, 167] or reduced the CF-associated delayed small intestinal transit time [111]. Other experimental drugs also carry the potential to increase gut fluidity, but have not yet been tested in CFTR-deficient mice [28, 59]. Two agents, one of them a TMEM16a/SLC26A3 inhibitor [181] and the other one an intestine-specific, selective, and FDA-approved NHE3 inhibitor [167], were able to significantly reduce the frequency of intestinal obstructions in CFTR null mice. Both agents also reduced the mucus impactions in the intestine The latter study demonstrated a reversal of several of the “CF gut” features within the short 3-week period of the application period, including a decrease in cryptal hyperproliferation, mucus accumulation, and mucosal mast cell number. Figure 2 schematically explains the mode of action of NHE3 and SLC26A3/A6 inhibitors may increase luminal fluidity in the CF gut. Only NHE3 inhibition will result in both an increase in fluidity and alkalinity in the CF gut. These studies raise hope that pharmacological therapies will soon be available to ameliorate the intestinal symptoms in all patients with cystic fibrosis.
Schematic diagram of pharmacological strategies to increase the luminal fluidity in the CFTR-deficient intestine. In the left panel, the situation in the villous/surface enterocytes of the CFTR-deficient intestine is depicted. The ongoing absorptive activity of the absorptive enterocytes, together with the lack of fluid/alkaline secretion from the CFTR-expressing cryptal region, results in an acidic, dehydrated gut lumen. Left-middle panel: Oral inhibition of the apical Na/H exchanger isoform NHE3 with the intestine-specific selective NHE3 inhibitor tenapanor results in an increase in luminal fluidity and alkalinity in the intestine of CFTR null or F508del mutant mice [141, 149]. Middle-right and right panel: The inhibitors for SLC26A3 [112] and SLCA6 [108] are also able to inhibit fluid absorption and may be beneficial to alleviate constipation and obstructive episodes in patients with CF. They are not expected to increase the luminal alkalinity, however. The full names for the abbreviations can be found in the manuscript
Congenital chloride diarrhea CCD (chloride-losing diarrhea, CLD)
Early intestinal perfusion studies in CLD patients localized the defective transport to the ileocolon [174]. Therefore, compensatory mechanisms, such as the expression of SLC26a6, passive Cl− absorption, or the predominant role of nutrient-coupled electrolyte absorptive mechanisms, may mitigate the effects of a defective SLC26a3 in the small intestine of patients with CLD. In the large intestine, alternative fluid and electrolyte uptake systems are available, but their efficacy may be compromised by the low luminal pH [92, 93, 198] and by the dysbiosis with a strong reduction of SCFA-producing bacteria [93]. Indeed, the luminal application of SCFA in the concentrations that are present in the healthy colon increased the alkaline output into the luminal solution in isolated chambered slc26a3−/− mucosa [60], and it resulted in a strong increase in fluid absorptive rates in the slc26a3−/− cecum and colon in anesthetized mice (Tan, Qinghai. 2021, unpublished observations). However, an oral application of butyrate salt or of tributyrin did not significantly increase the cecal and colonic SCFA levels and did not reverse the diarrhea in slc26a3−/− mice (Ye, Zhenghao and Kini, Archana, unpublished observations), demonstrating that even high doses of butyrate, taken orally, are completely absorbed in the small intestine of mice. Consistent with these observations, the oral application of butyrate to patients did not result in an improvement of the CLD biomarkers [190].
However, one pediatric center was able to apply surprisingly high doses of oral butyrate to CLD children and normalize their stool and serum parameters [18, 40]. Since oral butyrate salts firstly smell very bad even in a microencapsulated form, need to be applied in high doses, and are absorbed in the small intestine, the challenge will be to deliver the high millimolar concentrations required for effective SCFA-dependent fluid absorption to the colon. Possibly, a strategy will be developed to replenish the missing colonic microbiota and thereby enhance local production of SCFA in the colon of CLD patients.
Inflammatory bowel disease
Many studies have been conducted to explore the electrolyte transport abnormalities in the inflamed mucosa of IBD patients of animal models of intestinal inflammation, summarized in reviews that have been published in the last decades [6, 106, 110, 147, 204]. One prominent feature of IBD is a strong decrease in the expression of SCL26a3 in the inflamed colonic epithelium, resulting not only in reduced electrolyte and fluid absorption but also in a reduction in luminal alkalinization [197]. However, the paracellular leakage of HCO3− through the tight junctional pathway with a loss of cation selectivity may offset the reduced SLC26A3-mediated luminal alkalinization, in particular in the ileum and proximal colon, where SLC26A3 expression is much lower than in the mid-distal colon [86]. This may be a reason why pH capsule investigations of patients with IBD gave mixed results [118, 127, 202]. Polymorphisms in SLC26A3 have been associated with either an increased incidence of IBD [9, 51, 150] or have been associated with response to therapy [8, 17, 188]. Therefore, intense research has been ongoing to elucidate the potential role of SLC26A3 in mucosal protection, as mentioned above, and in the maintenance of barrier properties [19, 81]. The hope is to somehow restore Slc26a3 function in IBD [58, 128, 199]. However, recent evidence suggests that the downregulation of SLC26A3 observed in the inflamed mucosa of IBD patients is just one component of a dysregulated differentiation process in the inflamed mucosa which prevents the full differentiation of absorptive enterocytes [116]. Therefore, the only effective strategy to improve the expression and function of the absorptive ion transporters may be an effective anti-inflammatory treatment.
Acid/base sensing in the intestine
As already described in the previous chapters, luminal pH has to be tightly controlled to provide adequate defense of the intestinal epithelium against luminal acid and to maintain homeostasis. Therefore, the concentration of acid/base equivalents is tightly monitored by a sophisticated network of proton- and bicarbonate-sensing proteins, which are situated in epithelial cells and sensory neurons along the gastrointestinal tract. These acid/base-sensing proteins comprise acid-sensitive ion channels (ASICs) and transient receptor potential cation channels (TRPs) [67, 124, 164, 206]. But also, other acid/base-sensitive proteins like soluble adenylyl cyclase (sAC), two-pore domain potassium (TASK) channels, H+-sensing G-protein-coupled receptors (GPCRs), P2X receptors, and inward rectifier potassium (Kir) channels could play a role in gastrointestinal pH sensing [55, 57, 68, 70]. Besides pH-sensing proteins, efficient acid/base sensing also requires acid/base transporters and carbonic anhydrases (CAs) [3].
Luminal acid/base sensing requires catalytic function of carbonic anhydrases
CAs catalyze the reversible hydration of CO2 to HCO3− and H+. Due to the fast interconversion, CO2, HCO3−, and H+ form a “trinity,” which allows both H+ and HCO3− sensors to monitor changes in pH, bicarbonate concentration, and CO2 partial pressure at the same time.
A good example of how CAs, acid/base transporters, and acid receptors work together to monitor luminal pH is acid sensing by afferent neurons in the duodenum, as first proposed by Akiba and colleagues [2, 3] (Fig. 3): Luminal pH in the duodenum can rapidly change between 2 and 7, due to bursts of acid from the stomach. Therefore, the duodenal mucosa has to be able to rapidly adjust its defense mechanism against luminal acid. The acid is neutralized by HCO3−, which is secreted from duodenal epithelial cells by bicarbonate transporters from the SLC26 family and the cystic fibrosis transmembrane conductance regulator (CFTR). In the mucous layer, H+ and HCO3− react to CO2, catalyzed by extracellular CAs, which are situated at the apical site of the membrane. The CO2 diffuses from the mucus layer into the cell, where it is hydrated to H+ and HCO3−, catalyzed by cytosolic CA. While HCO3− is again secreted at the apical site to support neutralization of luminal acid, H+ is exported into the interstitial space via Na+/H+ exchanger 1 (NHE1) at the basolateral site of the epithelial cell. The H+ activates proton receptors, situated on adjacent neurons of afferent nerves, which in turn stimulate secretion of HCO3− and mucus to protect the mucosa from further acidosis. Through this cascade, luminal pH can be precisely monitored by neuronal acid sensors, even if these nerve fibers have no direct access to the lumen [2, 3]. This hypothesis has been tested by assessing the intracellular pH (pHi) of the duodenal villi during acid exposure in vivo by two-photon microscopy in mice that were deficient for the major intracellular CA isoform in the duodenocytes, namely, CAII, and their WT littermates [161]. The authors found that in WT mice, a 5-min exposure of the duodenal mucosa to a pH of 2.2 resulted in strong decrease of the duodenocyte pHi in the villus tip and mid-villus region, which was strongly blunted in the absence of CAII. In parallel, the acid-induced bicarbonate secretory response was virtually ablated in the CAII-deficient duodenum, but only mildly reduced during perfusion with a membrane-impermeable CA inhibitor. Thus, the conduction of an “acid” signal through the duodenocyte to the acid-sensing receptors on neuronal structures requires both luminal and intracellular CAs. However, the CAII was not essential for the HCO3− stimulatory response of the epithelium to secretagogues such as forskolin or the stable PGE2 analogue 16,16,-dimethyl PGE2.
Acid sensing by afferent neurons in the duodenum is mediated by the collaboration between carbonic anhydrases, acid/base transporters, and acid receptors. Protons, which enter the mucus gel layer, are neutralized by HCO3−, which is exported from the duodenal mucosal cell via Cl−/HCO3− exchangers and CFTR. The reaction of H+ and HCO3− to CO2 is catalyzed by extracellular CA. CO2 diffuses into the cell, where it is again hydrated by intracellular CAs. While HCO3− is again exported on the apical side to neutralize acid, H+ is exported from the cell on the basolateral side via NHE1. H+ can then activate H+ receptors like TRPV1 on the surface of neurons of afferent nerves, to induce neuronal activity. Figure modified from [2, 68]
Role of acid-sensing ion channels in gastrointestinal acid/base sensing
Acid sensing in afferent nerve fibers of the gastrointestinal tract is mainly mediated by the transient receptor potential cation channel subfamily V member 1 (TRPV1), also termed capsaicin receptor or vanilloid receptor 1. TRPV1 belongs to the transient receptor potential (TRP) channels. TRPs comprise six families, five of which (TRPV, TRPM, TRPA, TRPP, TRPC) are relevant for chemo-, thermo-, or mechanosensation [29]. Out of these five subfamilies, only TRPV1 has been attributed a function in gastrointestinal acid sensing. TRPV1 is a non-selective cation channel with a high Ca2+ permeability, but can also function as proton channel at low pH [61, 68]. The channel is opened at acidic pH values below 6; however, mild acidity can sensitize TRPV1 to other stimuli like heat [68, 85, 170].
Acid-induced secretion of bicarbonate in the duodenum can also be mediated by acid-sensitive ion channels (ASICs), which are expressed in intestinal epithelial cells [42, 208]. ASICs are proton-gated cation channels, which are activated by protonation of the extracellular loop and therefore serve as detectors for extracellular acidification [96, 180, 193]. ASICs have a high permeability for Na+ ions; however, some isoforms also show substantial conductance for other cations like Ca2+ or K+ [68, 208]. In mammals, ASICs are encoded by three different genes (ACCN1, ACCN2, and ACCN3). These three genes produce the five protein isoforms ASIC1a, ASIC1b, ASIC2b, and ASIC3 by alternative splicing, which can form homo- and heterodimers [68]. ASICs have been attributed various physiological and pathophysiological functions, including gastrointestinal mechanoreception [121], learning and memory [191, 203], olfaction [177], pain sensation and fear [38, 39, 192], heart failure [56], and neuronal disorders like epilepsy, mood disorders, and Alzheimer’8520/s disease [162]. Furthermore, ASICs play a role in gastrointestinal pain, gastroesophageal reflux disease, and gastric cancer, where expression of ASIC1a correlates with cancer progression and formation of metastasis [25, 208]. In the duodenum, ASIC1a is thought to be involved in the regulation of bicarbonate secretion [42]: By performing measurements in mouse duodenal epithelial cells and the human intestinal epithelial cell line HT29, the authors could show that extracellular acidification induces an increase in intracellular Ca2+ concentration and secretion of HCO3−. Both Ca2+ increase and HCO3− secretion were inhibited by inhibition of ASICs with amiloride. From this, it was concluded that ASICs, expressed in duodenal epithelial cells, can induce duodenal HCO3− secretion via a Ca2+-dependent pathway [42].
Proton-sensing G-protein coupled receptors in the gastrointestinal tract and their role in IBD
Proton-sensing G-protein coupled receptors (GPRs) serve as detectors for extracellular acidification in almost every tissue. H+-sensitive GPRs comprise of the four members GPR4, GPR65 (TDAG8), GPR68 (OGR1), and GPR132 (G2A) [104, 159]. GPR132, however, displays only weak proton-sensitivity and was not found to have pH-sensitive functions [129]. GPR4 and GPR68 are ubiquitously expressed, including the GI tract, while expression of GPR65 is restricted to lymphoid tissue [159]. GPR4 and GPR65 have both been attributed functions in inflammatory bowel disease (IBD).
Inflammation promotes glycolytic energy production, which is attributed to the increased demand for energy by infiltrating immune cells and to local hypoxia of the mucosal tissue, which results in increased formation of lactate and protons [37, 95, 122]. The acidification activates GPR4 and GPR65 with severe consequences. Activation of GPR4 results in increased expression of various inflammatory genes, including different chemokines and cytokines, adhesion molecules, and COX-2. Furthermore, it activated stress-response genes, such as ATF3 and CHOP, and increased cell adhesion though the cAMP/Epac pathway [23, 43]. Thereby, GPR4 can exacerbate inflammation, which results in a positive feedback loop that again activates GPR4 and drives further inflammation [187]. Indeed, it was shown that absence of GPR4 or pharmacological inhibition attenuates colitis in an IBD mouse model, including less severe inflammation [137, 138]. It was therefore concluded that GPR4 might serve as a potential drug target for the treatment of IBD.
GPR68 does also play a role in IBD, mainly by regulation of the intestinal barrier function [35, 36]. GPR68 is coupled via the G-protein Gq11 and activates an intracellular signaling cascade with phospholipase C (PLCβ), inositol phosphate 3 (IP3), elevation of Ca2+, and extracellular signal-regulated kinase (ERK) [104], but it was also shown to couple via Gα12/13 and the Rho pathway [36].
GPR68 was found to be increased in the mucosa of patients with IBD and inflamed segments showed higher abundance of GPR68 than uninflamed mucosa [37]. Short-term expression of GPR68 is induced by the proinflammatory cytokine TNF, which was also shown to function as a major mediator for IBD-associated inflammation. GPR68 is expressed in endothelial cells, macrophages, granulocytes, and fibroblasts. In fibroblasts, activation of GPR68 by extraocular acidification induced formation of inositol phosphate, Rho activation, and formation of F-actin and stress fibers and does therefore increases epithelial barrier function [36]. In IBD patients, expression of GPR68 positively correlates with the expression of the profibrotic genes Vim, Col3a1, Tgfb1, and Ctgf and cellular deposition of collagen [73]. In the CaCo-2 cell line, an acidic pH shift from 7.8 to 6.6 improved barrier function and stimulated the reorganization of F-actin and formation of stress fibers. Furthermore, acidic pH inhibited proliferation and cell migration within a wound healing assay [35]. It was also shown that GPR68 deficiency protects from inflammation in an IL-10 knockout mouse model of IBD [35]. GPR68 also contributed a role in the regulation of ER stress via the IRE1α-JNK pathway, as well as blockage of late stage autophagy [105].
IBD is usually associated with local acidification which can result in severe alterations in epithelial barrier function. Therefore, it would seem that strengthening of intestinal barrier function should be beneficial. However, cell proliferation and migration are required to regain homeostasis. Therefore, chronic activation of GPR68 could exacerbate tissue damage in IBD [36].
Soluble adenylate cyclase is a bicarbonate sensor in the gastrointestinal tract
A bona fide bicarbonate sensor, which is also expressed in the gastrointestinal tract, is soluble adenylyl cyclase (sAC). Adenylyl clyclases catalyze the conversion of ATP to AMP, which functions as second messenger, either by promoting protein phosphorylation via cAMP-dependent protein kinase or by direct activation of cAMP-regulated proteins [134]. Mammals express ten isoforms of adenylyl clyclases. However, out of these ten isoforms, nine are membrane-bound and activated by the G protein α subunit; only the sAC isoform is directly activated by binding of HCO3− to the enzyme [55, 87, 120, 179]. Human sAC has an EC50 between 11 and 12 mM for HCO3−, which is close to physiological HCO3− concentration and enables sAC to detect already small changes in intracellular HCO3− concentration [22, 87]. Therefore, sAC can serve as a key regulator for acid/base-depending cell signaling in various intracellular compartments, including cytosolic microdomains and organelles like mitochondria and the nucleus [1, 209]. A recent study could demonstrate that sAC can regulate the cytosolic NADH/NAD+ redox state and is therefore involved in the bioenergetic switch between glycolysis and oxidative phosphorylation [21]. sAC was first found in the testis [15] but is ubiquitously expressed in mammalian tissue, including the intestine [67]. Intestinal HCO3− sensing by sAC, however, has been primarily studied in teleost and cartilage fish: Marine fish, which live in a hyperosmotic environment, absorb water through their intestine to compensate for dehydration due to water loss across the gills. Water absorption is driven by absorption of Na+ and Cl− via Na–K-2Cl-Cotransporters (NKCC) and Cl−/HCO3− exchangers in the gastrointestinal tract. Water absorption, however, also requires the removal of divalent cations like Ca2+ and Mg2+ to further decrease osmotic pressure. Removal of Ca2+ and Mg2+ is facilitated by HCO3−, which is secreted in exchange for Cl− via an anion exchanger of the SLC26A6 family on the apical site of intestinal cells [99]. Additionally, HCO3− can be imported into the epithelial cell from the apical side via the Na+/HCO3− cotransporter NBCe1 [99] or luminal CO2, which diffuses back into the cell and is converted to HCO3− and H+ by intracellular carbonic anhydrase in the subapical region of the cytosol [171]. This results in extremely high luminal HCO3− concentrations of more than 100 mM. The resulting alkaline conditions induce precipitation of Mg2+ and Ca2+ ions as MgCO3 and CaCO3 and reduce osmotic pressure to facilitate water absorption [171, 194]. Furthermore, the HCO3− activates sAC. Activated sAC activates the NKCC and triggers intestinal NaCl absorption [20, 194]. By this mechanism, sAC can locally modulate bicarbonate secretion and water absorption in the fish intestine [20, 194].
Outlook
Many of the reviewed publications have been performed in genetically altered mice. However, this has recently changed, with new studies focusing on HCO3− transport and the regulation of enterocyte pH in human intestinal two- or three-dimensional organoids. Although the in vitro differentiation of intestinal organoids still needs refinement, it is anticipated that this technique, in combination with genetic manipulations and novel optical approaches to study acid/base transport in cultured epithelia, will greatly enhance our understanding of the regulation and interplay of the different ion transport proteins and pH sensors along the crypt-villus/surface axes of the different intestinal segments.
Data availability
No datasets were generated or analyzed during the current study.
Abbreviations
- AE2:
-
Anion exchanger isoform 2
- ASIC:
-
Acid-sensitive ion channel
- CA:
-
Carbonic anhydrase
- CF:
-
Cystic fibrosis
- CFTR:
-
Cystic fibrosis transmembrane conductance regulator
- CCD:
-
Congenital chloride diarrhea
- CLD:
-
Chloride-losing diarrhea
- DIDS:
-
4,4′-Diisothiocyano-2,2′-stilbenedisulfonic acid
- DRA:
-
Downregulated in adenoma (SLC26A3)
- ENaC:
-
Epithelial sodium channel
- GI:
-
Gastrointestinal
- GPCR:
-
G-protein-coupled receptor
- IBD:
-
Inflammatory bowel disease
- MCT1:
-
Monocarboxylate transporter isoform 1
- NBCe1:
-
Electrogenic Na+/HCO3− cotransporter isoform 1
- NBCn1:
-
Electroneutral Na+/HCO3− cotransporter isoform 1
- NHE:
-
Sodium/proton exchanger
- NKCC1:
-
Na–K–Cl cotransporter
- OSR1:
-
Odd-skipped-related 1
- sAC:
-
Soluble adenylyl cyclase
- SCFA:
-
Short-chain fatty acids
- SLC26:
-
Solute carrier family 26
- SPAK:
-
Ste20-related proline alanine-rich kinase
- sMCT1:
-
Sodium-coupled monocarboxylate transporter isoform 1
- TASK:
-
Two-pore domain potassium channel
- TMEM16a:
-
Transmembrane member 16A
- TRP:
-
Transient receptor potential cation channel
- WNK:
-
With no lysine kinase
- wt:
-
Wild type
References
Acin-Perez R, Salazar E, Kamenetsky M, Buck J, Levin LR, Manfredi G (2009) Cyclic AMP produced inside mitochondria regulates oxidative phosphorylation. Cell Metab 9:265–276. https://doi.org/10.1016/j.cmet.2009.01.012
Akiba Y, Kaunitz JD (2009) Luminal chemosensing and upper gastrointestinal mucosal defenses. Am J Clin Nutr 90:826S-831S. https://doi.org/10.3945/ajcn.2009.27462U
Akiba Y, Ghayouri S, Takeuchi T, Mizumori M, Guth PH, Engel E, Swenson ER, Kaunitz JD (2006) Carbonic anhydrases and mucosal vanilloid receptors help mediate the hyperemic response to luminal CO2 in rat duodenum. Gastroenterology 131:142–152. https://doi.org/10.1053/j.gastro.2006.04.018
Alper SL, Stewart AK, Chernova MN, Zolotarev AS, Clark JS, Vandorpe DH (2006) Anion exchangers in flux: functional differences between human and mouse SLC26A6 polypeptides. Novartis Found Symp 273:107–19
Alper SL, Stewart AK, Vandorpe DH, Clark JS, Horack RZ, Simpson JE, Walker NM, Clarke LL (2011) Native and recombinant Slc26a3 (downregulated in adenoma, Dra) do not exhibit properties of 2Cl-/1HCO3- exchange. Am J Physiol Cell Physiol 300:C276–C286. https://doi.org/10.1152/ajpcell.00366.2010
Anbazhagan AN, Priyamvada S, Alrefai WA, Dudeja PK (2018) Pathophysiology of IBD associated diarrhea. Tissue Barriers 6:e1463897. https://doi.org/10.1080/21688370.2018.1463897
Argenzio RA, Southworth M, Lowe JE, Stevens CE (1977) Interrelationship of Na, HCO3, and volatile fatty acid transport by equine large intestine. Am J Physiol 233:E469–E478. https://doi.org/10.1152/ajpendo.1977.233.6.E469
Asano K, Matsushita T, Umeno J, Hosono N, Takahashi A, Kawaguchi T, Matsumoto T, Matsui T, Kakuta Y, Kinouchi Y, Shimosegawa T, Hosokawa M, Arimura Y, Shinomura Y, Kiyohara Y, Tsunoda T, Kamatani N, Iida M, Nakamura Y, Kubo M (2009) A genome-wide association study identifies three new susceptibility loci for ulcerative colitis in the Japanese population. Nat Genet 41:1325–1329. https://doi.org/10.1038/ng.482
Asano K, Esaki M, Umeno J, Hirano A, Maehata Y, Moriyama T, Nakamura S, Matsumoto T, Kitazono T (2015) Contribution of susceptibility variants at FCGR2A and 13q12 to the risk of relapse among Japanese patients with ulcerative colitis. J Gastroenterol 50:1094–1102. https://doi.org/10.1007/s00535-015-1062-3
Bieberdorf FA, Gorden P, Fordtran JS (1972) Pathogenesis of congenital alkalosis with diarrhea. Implications for the physiology of normal ileal electrolyte absorption and secretion. J Clin Invest 51:1958–1968. https://doi.org/10.1172/JCI107002
Binder HJ (2010) Role of colonic short-chain fatty acid transport in diarrhea. Annu Rev Physiol 72:297–313
Binder HJ, Rajendran V, Sadasivan V, Geibel JP (2005) Bicarbonate secretion: a neglected aspect of colonic ion transport. J Clin Gastroenterol 39:S53–S58. https://doi.org/10.1097/01.mcg.0000155521.81382.3a
Boedtkjer E, Praetorius J, Füchtbauer E-M, Aalkjaer C (2008) Antibody-independent localization of the electroneutral Na+-HCO3- cotransporter NBCn1 (slc4a7) in mice. Am J Physiol Cell Physiol 294:C591-603. https://doi.org/10.1152/ajpcell.00281.2007
Boldyreff W (1914) The self-regulation of the acidity of the gastric contents and the real acidity of the gastric juice. Q J Exp Physiol 8:1–12. https://doi.org/10.1113/expphysiol.1914.sp000167
Braun T, Dods RF (1975) Development of a Mn2+ sensitive, “soluble” adenylate cyclase in rat testis. Proc Natl Acad Sci U S A 72:1097–1101. https://doi.org/10.1073/pnas.72.3.1097
Calam J (1995) Pathogenic mechanisms. Baillieres Clin Gastroenterol 9:487–506. https://doi.org/10.1016/0950-3528(95)90044-6
Camarillo GF, Goyon EI, Zuñiga RB, Salas LAS, Escárcega AEP, Yamamoto-Furusho JK (2020) Gene expression profiling of mediators associated with the inflammatory pathways in the intestinal tissue from patients with ulcerative colitis. Mediators Inflamm 2020:9238970. https://doi.org/10.1155/2020/9238970
Canani RB, Terrin G, Cirillo P, Castaldo G, Salvatore F, Cardillo G, Coruzzo A, Troncone R (2004) Butyrate as an effective treatment of congenital chloride diarrhea. Gastroenterology 127:630–634. https://doi.org/10.1053/j.gastro.2004.03.071
Cartwright IM, Dowdell AS, Lanis JM, Brink KR, Mu A, Kostelecky RE, Schaefer REM, Welch N, Onyiah JC, Hall CHT, Gerich ME, Tabor JJ, Colgan SP (2021) Mucosal acidosis elicits a unique molecular signature in epithelia and intestinal tissue mediated by GPR31-induced CREB phosphorylation. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2023871118
Carvalho ESM, Gregório SF, Power DM, Canário AVM, Fuentes J (2012) Water absorption and bicarbonate secretion in the intestine of the sea bream are regulated by transmembrane and soluble adenylyl cyclase stimulation. J Comp Physiol B Biochem Syst Environ Physiol 182:1069–1080. https://doi.org/10.1007/s00360-012-0685-4
Chang JC, Go S, Gilglioni EH, Duijst S, Panneman DM, Rodenburg RJ, Li HL, Huang HL, Levin LR, Buck J, Verhoeven AJ, Oude Elferink RPJ (2021) Soluble adenylyl cyclase regulates the cytosolic NADH/NAD+ redox state and the bioenergetic switch between glycolysis and oxidative phosphorylation. Biochim Biophys Acta - Bioenerg 1862:148367. https://doi.org/10.1016/j.bbabio.2020.148367
Chen Y, Cann MJ, Litvin TN, Iourgenko V, Sinclair ML, Levin LR, Buck J (2000) Soluble adenylyl cyclase as an evolutionarily conserved bicarbonate sensor. Science 289:625–628. https://doi.org/10.1126/science.289.5479.625
Chen A, Dong L, Leffler NR, Asch AS, Witte ON, Yang L V. (2011) Activation of GPR4 by acidosis increases endothelial cell adhesion through the cAMP/Epac pathway. PLoS One 6. https://doi.org/10.1371/journal.pone.0027586
Chen M, Praetorius J, Zheng W, Xiao F, Riederer B, Singh AK, Stieger N, Wang J, Shull GE, Aalkjaer C, Seidler U (2012) The electroneutral Na+:HCOa- cotransporter NBCn1 is a major pHi regulator in murine duodenum. J Physiol 590:3317–3333. https://doi.org/10.1113/jphysiol.2011.226506
Chen X, Sun X, Wang Z, Zhou X, Xu L, Li F, Zhang X, Pan J, Qi L, Qian H, Mao Z (2018) Involvement of acid-sensing ion channel 1a in gastric carcinoma cell migration and invasion. Acta Biochim Biophys Sin (Shanghai) 50:440–446. https://doi.org/10.1093/abbs/gmy026
Chernova MN, Jiang L, Friedman DJ, Darman RB, Lohi H, Kere J, Vandorpe DH, Alper SL (2005) Functional comparison of mouse slc26a6 anion exchanger with human SLC26A6 polypeptide variants: differences in anion selectivity, regulation, and electrogenicity. J Biol Chem 280:8564–8580. https://doi.org/10.1074/jbc.M411703200
Choi I, Aalkjaer C, Boulpaep EL, Boron WF (2000) An electroneutral sodium/bicarbonate cotransporter NBCn1 and associated sodium channel. Nature 405:571–575. https://doi.org/10.1038/35014615
Cil O, Haggie PM, Tan J-AT, Rivera AA, Verkman AS (2021) SLC26A6-selective inhibitor identified in a small-molecule screen blocks fluid absorption in small intestine. JCI insight 6. https://doi.org/10.1172/jci.insight.147699
Clapham DE, Julius D, Montell C, Schultz G (2005) International Union of Pharmacology. XLIX. Nomenclature and structure-function relationships of transient receptor potential channels. Pharmacol Rev 57:427–450. https://doi.org/10.1124/pr.57.4.6
Clarke LL, Harline MC (1998) Dual role of CFTR in cAMP-stimulated HCO3- secretion across murine duodenum. Am J Physiol 274:G718–G726. https://doi.org/10.1152/ajpgi.1998.274.4.G718
Cong L, Ran FA, Cox D, Lin S, Barretto R, Habib N, Hsu PD, Wu X, Jiang W, Marraffini LA, Zhang F (2013) Multiplex genome engineering using CRISPR/Cas systems. Science 339:819–823. https://doi.org/10.1126/science.1231143
Damkier HH, Nielsen S, Praetorius J (2006) An anti-NH2-terminal antibody localizes NBCn1 to heart endothelia and skeletal and vascular smooth muscle cells. Am J Physiol Heart Circ Physiol 290:H172–H180. https://doi.org/10.1152/ajpheart.00713.2005
Daniel H, Rehner G (1986) Effect of metabolizable sugars on the mucosal surface pH of rat intestine. J Nutr 116:768–777. https://doi.org/10.1093/jn/116.5.768
De Gregorio V, Imparato G, Urciuolo F, Netti PA (2018) Micro-patterned endogenous stroma equivalent induces polarized crypt-villus architecture of human small intestinal epithelium. Acta Biomater 81:43–59. https://doi.org/10.1016/j.actbio.2018.09.061
De Vallière C, Wang Y, Eloranta JJ, Vidal S, Clay I, Spalinger MR, Tcymbarevich I, Terhalle A, Ludwig MG, Suply T, Fried M, Kullak-Ublick GA, Frey-Wagner I, Scharl M, Seuwen K, Wagner CA, Rogler G (2015) G protein-coupled pH-sensing receptor OGR1 is a regulator of intestinal inflammation. Inflamm Bowel Dis 21:1269–1281. https://doi.org/10.1097/MIB.0000000000000375
De Vallière C, Vida S, Clay I, Jurisic G, Tcymbarevich I, Lang S, Ludwig MG, Okoniewski M, Eloranta JJ, Kullak-Ublick GA, Wagner CA, Rogler G, Seuwen K (2015) The pH-sensing receptor OGR1 improves barrier function of epithelial cells and inhibits migration in an acidic environment. Am J Physiol - Gastrointest Liver Physiol 309:G475–G490. https://doi.org/10.1152/ajpgi.00408.2014
de Vallière C, Cosin-Roger J, Baebler K, Schoepflin A, Mamie C, Mollet M, Schuler C, Bengs S, Lang S, Scharl M, Seuwen K, Ruiz PA, Hausmann M, Rogler G (2022) pH-sensing G protein-coupled receptor OGR1 (GPR68) expression and activation increases in intestinal inflammation and fibrosis. Int J Mol Sci 23:1–20. https://doi.org/10.3390/ijms23031419
Deval E, Lingueglia E (2015) Acid-sensing ion channels and nociception in the peripheral and central nervous systems. Neuropharmacology 94:49–57. https://doi.org/10.1016/j.neuropharm.2015.02.009
Deval E, Gasull X, Noël J, Salinas M, Baron A, Diochot S, Lingueglia E (2010) Acid-sensing ion channels (ASICs): pharmacology and implication in pain. Pharmacol Ther 128:549–558. https://doi.org/10.1016/j.pharmthera.2010.08.006
Di Meglio L, Grimaldi G, Esposito F, Gelzo M, Esposito MV, Castaldo G, Canani RB (2021) Step-up approach for sodium butyrate treatment in children with congenital chloride diarrhea. Front Pediatr 9:810765. https://doi.org/10.3389/fped.2021.810765
Ding X, Li D, Li M, Tian D, Yu H, Yu Q (2018) Tumor necrosis factor-α acts reciprocally with solute carrier family 26, member 3, (downregulated-in-adenoma) and reduces its expression, leading to intestinal inflammation. Int J Mol Med 41:1224–1232. https://doi.org/10.3892/ijmm.2017.3347
Dong X, Ko KH, Chow J, Tuo B, Barrett KE, Dong H (2011) Expression of acid-sensing ion channels in intestinal epithelial cells and their role in the regulation of duodenal mucosal bicarbonate secretion. Acta Physiol 201:97–107. https://doi.org/10.1111/j.1748-1716.2010.02207.x
Dong L, Li Z, Leffler NR, Asch AS, Chi JT, Yang L V. (2013) Acidosis activation of the proton-sensing GPR4 receptor stimulates vascular endothelial cell inflammatory responses revealed by transcriptome analysis. PLoS One 8. https://doi.org/10.1371/journal.pone.0061991
El Khouri E, Touré A (2014) Functional interaction of the cystic fibrosis transmembrane conductance regulator with members of the SLC26 family of anion transporters (SLC26A8 and SLC26A9): physiological and pathophysiological relevance. Int J Biochem Cell Biol 52:58–67. https://doi.org/10.1016/j.biocel.2014.02.001
Feil W, Lacy ER, Wong YM, Burger D, Wenzl E, Starlinger M, Schiessel R (1989) Rapid epithelial restitution of human and rabbit colonic mucosa. Gastroenterology 97:685–701. https://doi.org/10.1016/0016-5085(89)90640-9
Fiddian-Green RG, Silen W (1975) Mechanisms of disposal of acid and alkali in rabbit duodenum. Am J Physiol 229:1641–1648. https://doi.org/10.1152/ajplegacy.1975.229.6.1641
Flemström G, Sachs TG (1975) Ion transport by amphibian antrum in vitro. I General characteristics Am J Physiol 228:1188–1198. https://doi.org/10.1152/ajplegacy.1975.228.4.1188
Fordtran JS, Rector FC, Carter NW (1968) The mechanisms of sodium absorption in the human small intestine. J Clin Invest 47:884–900. https://doi.org/10.1172/JCI105781
Freel RW, Hatch M, Green M, Soleimani M (2006) Ileal oxalate absorption and urinary oxalate excretion are enhanced in Slc26a6 null mice. Am J Physiol Gastrointest Liver Physiol 290:G719–G728. https://doi.org/10.1152/ajpgi.00481.2005
Freel RW, Morozumi M, Hatch M (2009) Parsing apical oxalate exchange in Caco-2BBe1 monolayers: siRNA knockdown of SLC26A6 reveals the role and properties of PAT-1. Am J Physiol Gastrointest Liver Physiol 297:G918–G929. https://doi.org/10.1152/ajpgi.00251.2009
Fujii T, Sato M, Hosoi K, Ohbayashi N, Ikuse T, Jimbo K, Aoyagi Y, Kudo T, Ohtsuka Y, Shimizu T (2016) Assessment of the family history of patients with ulcerative colitis at a single center in Japan. J Pediatr Gastroenterol Nutr 63:512–515. https://doi.org/10.1097/MPG.0000000000001275
Gawenis LR, Bradford EM, Prasad V, Lorenz JN, Simpson JE, Clarke LL, Woo AL, Grisham C, Sanford LP, Doetschman T, Miller ML, Shull GE (2007) Colonic anion secretory defects and metabolic acidosis in mice lacking the NBC1 Na+/HCO3- cotransporter. J Biol Chem 282:9042–9052. https://doi.org/10.1074/jbc.M607041200
Gelfond D, Ma C, Semler J, Borowitz D (2013) Intestinal pH and gastrointestinal transit profiles in cystic fibrosis patients measured by wireless motility capsule. Dig Dis Sci 58:2275–2281. https://doi.org/10.1007/s10620-012-2209-1
Gelfond D, Heltshe S, Ma C, Rowe SM, Frederick C, Uluer A, Sicilian L, Konstan M, Tullis E, Roach RNC, Griffin K, Joseloff E, Borowitz D (2017) Impact of CFTR modulation on intestinal pH, motility, and clinical outcomes in patients with cystic fibrosis and the G551D mutation. Clin Transl Gastroenterol 8:e81. https://doi.org/10.1038/ctg.2017.10
Geng W, Wang Z, Zhang J, Reed BY, Pak CYC, Moe OW (2005) Cloning and characterization of the human soluble adenylyl cyclase. Am J Physiol - Cell Physiol 288:1305–1316. https://doi.org/10.1152/ajpcell.00584.2004
Gibbons DD, Kutschke WJ, Weiss RM, Benson CJ (2015) Heart failure induces changes in acid-sensing ion channels in sensory neurons innervating skeletal muscle. J Physiol 593:4575–4587. https://doi.org/10.1113/JP270690
Goldstein SAN, Bayliss DA, Kim D, Lesage F, Plant LD (2005) Nomenclature and molecular relationships of two-P potassium channels. Pharmacol Rev 57:527–540. https://doi.org/10.1124/pr.57.4.12.1
Guo Y, Li X, Geng C, Song S, Xie X, Wang C (2023) Vitamin D receptor involves in the protection of intestinal epithelial barrier function via up-regulating SLC26A3. J Steroid Biochem Mol Biol 227:106231. https://doi.org/10.1016/j.jsbmb.2022.106231
Haggie PM, Cil O, Lee S, Tan J-A, Rivera AA, Phuan P-W, Verkman AS (2018) SLC26A3 inhibitor identified in small molecule screen blocks colonic fluid absorption and reduces constipation. JCI insight 3. https://doi.org/10.1172/jci.insight.121370
Hayashi H, Nagai H, Ohba K-I, Soleimani M, Suzuki Y (2021) Segmental differences in Slc26a3-dependent Cl- absorption and HCO3- secretion in the mouse large intestine in vitro in Ussing chambers. J Physiol Sci 71:5. https://doi.org/10.1186/s12576-020-00784-9
Hellwig N, Plant TD, Janson W, Schäfer M, Schultz G, Schaefer M (2004) TRPV1 acts as proton channel to induce acidification in nociceptive neurons. J Biol Chem 279:34553–34561. https://doi.org/10.1074/jbc.M402966200
Heylings JR, Garner A (1981) Influence of luminal acidification on bicarbonate transport by gastric and duodenal isolated mucosae. Prostaglandins 21(Suppl):67–71. https://doi.org/10.1016/0090-6980(81)90120-9
Hogan DL, Rapier RC, Dreilinger A, Koss MA, Basuk PM, Weinstein WM, Nyberg LM, Isenberg JI (1996) Duodenal bicarbonate secretion: eradication of Helicobacter pylori and duodenal structure and function in humans. Gastroenterology 110:705–716. https://doi.org/10.1053/gast.1996.v110.pm8608879
Hogan DL, Crombie DL, Isenberg JI, Svendsen P, Schaffalitzky de Muckadell OB, Ainsworth MA (1997) Acid-stimulated duodenal bicarbonate secretion involves a CFTR-mediated transport pathway in mice. Gastroenterology 113:533–541. https://doi.org/10.1053/gast.1997.v113.pm9247473
Hogan DL, Crombie DL, Isenberg JI, Svendsen P, Schaffalitzky de Muckadell OB, Ainsworth MA (1997) CFTR mediates cAMP- and Ca2+-activated duodenal epithelial HCO3- secretion. Am J Physiol 272:G872–G878. https://doi.org/10.1152/ajpgi.1997.272.4.G872
Höglund P, Haila S, Socha J, Tomaszewski L, Saarialho-Kere U, Karjalainen-Lindsberg ML, Airola K, Holmberg C, de la Chapelle A, Kere J (1996) Mutations of the down-regulated in adenoma (DRA) gene cause congenital chloride diarrhoea. Nat Genet 14:316–319. https://doi.org/10.1038/ng1196-316
Holzer P (2009) Acid-sensitive ion channels and receptors. Handb Exp Pharmacol 194:283–332. https://doi.org/10.1007/978-3-540-79090-7_9
Holzer P (2011) Acid sensing by visceral afferent neurones. Acta Physiol 201:63–75. https://doi.org/10.1111/j.1748-1716.2010.02143.x
Hornick RB (1987) Peptic ulcer disease: a bacterial infection? N Engl J Med 316:1598–1600. https://doi.org/10.1056/NEJM198706183162509
Huang CW, Tzeng JN, Chen YJ, Tsai WF, Chen CC, Sun WH (2007) Nociceptors of dorsal root ganglion express proton-sensing G-protein-coupled receptors. Mol Cell Neurosci 36:195–210. https://doi.org/10.1016/j.mcn.2007.06.010
Hug MJ, Tamada T, Bridges RJ (2003) CFTR and bicarbonate secretion by [correction of to] epithelial cells. News Physiol Sci 18:38–42. https://doi.org/10.1152/nips.01412.2002
Hug MJ, Clarke LL, Gray MA (2011) How to measure CFTR-dependent bicarbonate transport: from single channels to the intact epithelium. Methods Mol Biol 741:489–509. https://doi.org/10.1007/978-1-61779-117-8_30
Hutter S, Van Haaften WT, Hünerwadel A, Baebler K, Herfarth N, Raselli T, Mamie C, Misselwitz B, Rogler G, Weder B, Dijkstra G, Meier CF, De Vallière C, Weber A, Imenez Silva PH, Wagner CA, Frey-Wagner I, Ruiz PA, Hausmann M (2018) Intestinal activation of pH-sensing receptor OGR1 [GPR68] contributes to fibrogenesis. J Crohn’s Colitis 12:1348–1358. https://doi.org/10.1093/ecco-jcc/jjy118
Isenberg JI, Selling JA, Hogan DL, Koss MA (1987) Impaired proximal duodenal mucosal bicarbonate secretion in patients with duodenal ulcer. N Engl J Med 316:374–379. https://doi.org/10.1056/NEJM198702123160704
Ishiguro H, Steward M, Naruse S (2007) Cystic fibrosis transmembrane conductance regulator and SLC26 transporters in HCOa- secretion by pancreatic duct cells. Sheng Li Xue Bao 59:465–476
Ishiguro H, Yamamoto A, Nakakuki M, Yi L, Ishiguro M, Yamaguchi M, Kondo S, Mochimaru Y (2012) Physiology and pathophysiology of bicarbonate secretion by pancreatic duct epithelium. Nagoya J Med Sci 74:1–18
Jacob P, Christiani S, Rossmann H, Lamprecht G, Vieillard-Baron D, Müller R, Gregor M, Seidler U (2000) Role of Na(+)HCO(3)(-) cotransporter NBC1, Na(+)/H(+) exchanger NHE1, and carbonic anhydrase in rabbit duodenal bicarbonate secretion. Gastroenterology 119:406–419. https://doi.org/10.1053/gast.2000.9358
Jacob P, Rossmann H, Lamprecht G, Kretz A, Neff C, Lin-Wu E, Gregor M, Groneberg DA, Kere J, Seidler U (2002) Down-regulated in adenoma mediates apical Cl-/HCO3- exchange in rabbit, rat, and human duodenum. Gastroenterology 122:709–724. https://doi.org/10.1053/gast.2002.31875
Jakab RL, Collaco AM, Ameen NA (2011) Physiological relevance of cell-specific distribution patterns of CFTR, NKCC1, NBCe1, and NHE3 along the crypt-villus axis in the intestine. Am J Physiol Gastrointest Liver Physiol 300:G82-98. https://doi.org/10.1152/ajpgi.00245.2010
Jang KK, Heaney T, London M, Ding Y, Putzel G, Yeung F, Ercelen D, Chen YH, Axelrad J, Gurunathan S, Zhou C, Podkowik M, Arguelles N, Srivastava A, Shopsin B, Torres VJ, Keestra-Gounder AM, Pironti A, Griffin ME, Hang HC, Cadwell K (2023) Antimicrobial overproduction sustains intestinal inflammation by inhibiting Enterococcus colonization. Cell Host Microbe 31(9):1450-1468.e8
Jayawardena D, Priyamvada S, Kageyama T, White Z, Kumar A, Griggs TF, Majumder A, Akram R, Anbazhagan AN, Sano T, Dudeja PK (2023) Loss of SLC26A3 results in colonic mucosal immune dysregulation via epithelial-immune cell crosstalk. Cell Mol Gastroenterol Hepatol 15:903–919. https://doi.org/10.1016/j.jcmgh.2022.12.009
Jiang Z, Grichtchenko II, Boron WF, Aronson PS (2002) Specificity of anion exchange mediated by mouse Slc26a6. J Biol Chem 277:33963–33967. https://doi.org/10.1074/jbc.M202660200
Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E (2012) A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science 337:816–821. https://doi.org/10.1126/science.1225829
Jinek M, East A, Cheng A, Lin S, Ma E, Doudna J (2013) RNA-programmed genome editing in human cells. Elife 2:e00471. https://doi.org/10.7554/eLife.00471
Jordt SE, Tominaga M, Julius D (2000) Acid potentiation of the capsaicin receptor determined by a key extracellular site. Proc Natl Acad Sci U S A 97:8134–8139. https://doi.org/10.1073/pnas.100129497
Juric M, Xiao F, Amasheh S, May O, Wahl K, Bantel H, Manns MP, Seidler U, Bachmann O (2013) Increased epithelial permeability is the primary cause for bicarbonate loss in inflamed murine colon. Inflamm Bowel Dis 19:904–911. https://doi.org/10.1097/MIB.0b013e3182813322
Kamenetsky M, Middelhaufe S, Bank EM, Levin LR, Buck J, Steegborn C (2006) Molecular details of cAMP generation in mammalian cells: a tale of two systems. J Mol Biol 362:623–639. https://doi.org/10.1016/j.jmb.2006.07.045
Karb DB, Cummings LC (2021) The intestinal microbiome and cystic fibrosis transmembrane conductance regulator modulators: emerging themes in the management of gastrointestinal manifestations of cystic fibrosis. Curr Gastroenterol Rep 23:17. https://doi.org/10.1007/s11894-021-00817-2
Kawamata K, Hayashi H, Suzuki Y (2006) Chloride-dependent bicarbonate secretion in the mouse large intestine. Biomed Res 27:15–21. https://doi.org/10.2220/biomedres.27.15
Kere J, Sistonen P, Holmberg C, de la Chapelle A (1993) The gene for congenital chloride diarrhea maps close to but is distinct from the gene for cystic fibrosis transmembrane conductance regulator. Proc Natl Acad Sci U S A 90:10686–10689. https://doi.org/10.1073/pnas.90.22.10686
Kim Y, Jun I, Shin DH, Yoon JG, Piao H, Jung J, Park HW, Cheng MH, Bahar I, Whitcomb DC, Lee MG (2020) Regulation of CFTR bicarbonate channel activity by WNK1: implications for pancreatitis and CFTR-related disorders. Cell Mol Gastroenterol Hepatol 9:79–103. https://doi.org/10.1016/j.jcmgh.2019.09.003
Kini A, Singh AK, Riederer B, Yang I, Tan X, di Stefano G, Tan Q, Xiao F, Xia W, Suerbaum S, Seidler U (2020) Slc26a3 deletion alters pH-microclimate, mucin biosynthesis, microbiome composition and increases the TNFα expression in murine colon. Acta Physiol 230:e13498. https://doi.org/10.1111/apha.13498
Kini A, Zhao B, Basic M, Roy U, Iljazovic A, Odak I, Ye Z, Riederer B, Di Stefano G, Römermann D, Koenecke C, Bleich A, Strowig T, Seidler U (2022) Upregulation of antimicrobial peptide expression in slc26a3-/- mice with colonic dysbiosis and barrier defect. Gut Microbes 14:2041943. https://doi.org/10.1080/19490976.2022.2041943
Knauf F, Ko N, Jiang Z, Robertson WG, Van Itallie CM, Anderson JM, Aronson PS (2011) Net intestinal transport of oxalate reflects passive absorption and SLC26A6-mediated secretion. J Am Soc Nephrol 22:2247–2255. https://doi.org/10.1681/ASN.2011040433
Krawczyk CM, Holowka T, Sun J, Blagih J, Amiel E, DeBerardinis RJ, Cross JR, Jung E, Thompson CB, Jones RG, Pearce EJ (2010) Toll-like receptor-induced changes in glycolytic metabolism regulate dendritic cell activation. Blood 115:4742–4749. https://doi.org/10.1182/blood-2009-10-249540
Krishtal OA, Pidoplichko VI (1980) A receptor for protons in the nerve cell membrane. Neuroscience 5:2325–2327. https://doi.org/10.1016/0306-4522(80)90149-9
Kumar A, Priyamvada S, Ge Y, Jayawardena D, Singhal M, Anbazhagan AN, Chatterjee I, Dayal A, Patel M, Zadeh K, Saksena S, Alrefai WA, Gill RK, Zadeh M, Zhao N, Mohamadzadeh M, Dudeja PK (2021) A novel role of SLC26A3 in the maintenance of intestinal epithelial barrier integrity. Gastroenterology 160:1240-1255.e3. https://doi.org/10.1053/j.gastro.2020.11.008
Kunzelmann K, Schreiber R, Hadorn HB (2017) Bicarbonate in cystic fibrosis. J Cyst Fibros 16:653–662. https://doi.org/10.1016/j.jcf.2017.06.005
Kurita Y, Nakada T, Kato A, Doi H, Mistry AC, Chang MH, Romero MF, Hirose S (2008) Identification of intestinal bicarbonate transporters involved in formation of carbonate precipitates to stimulate water absorption in marine teleost fish. Am J Physiol - Regul Integr Comp Physiol 294:1402–1412. https://doi.org/10.1152/ajpregu.00759.2007
Lamprecht G, Baisch S, Schoenleber E, Gregor M (2005) Transport properties of the human intestinal anion exchanger DRA (down-regulated in adenoma) in transfected HEK293 cells. Pflugers Arch 449:479–490. https://doi.org/10.1007/s00424-004-1342-x
Lee MG, Ahn W, Lee JA, Kim JY, Choi JY, Moe OW, Milgram SL, Muallem S, Kim KH (2001) Coordination of pancreatic HCO3- secretion by protein-protein interaction between membrane transporters. JOP 2:203–206
Legen I, Kristl A (2003) Factors affecting the microclimate pH of the rat jejunum in ringer bicarbonate buffer. Biol Pharm Bull 26:886–889. https://doi.org/10.1248/bpb.26.886
Liu X, Li T, Riederer B, Lenzen H, Ludolph L, Yeruva S, Tuo B, Soleimani M, Seidler U (2015) Loss of Slc26a9 anion transporter alters intestinal electrolyte and HCO3(-) transport and reduces survival in CFTR-deficient mice. Pflugers Arch 467:1261–1275. https://doi.org/10.1007/s00424-014-1543-x
Ludwig M-G, Vanek M, Guerini D, Gasser JA, Jones CE, Junker U, Hofstetter H, Wolf RM, Seuwen K (2003) Proton-sensing G-protein-coupled receptors. Nature 425:93–98. https://doi.org/10.1038/nature01905
Maeyashiki C, Melhem H, Hering L, Baebler K, Cosin-Roger J, Schefer F, Weder B, Hausmann M, Scharl M, Rogler G, de Vallière C, Ruiz PA (2020) Activation of pH-sensing receptor OGR1 (GPR68) induces ER stress via the IRE1α/JNK pathway in an intestinal epithelial cell model. Sci Rep 10:1–12. https://doi.org/10.1038/s41598-020-57657-9
Magalhães D, Cabral JM, Soares-da-Silva P, Magro F (2016) Role of epithelial ion transports in inflammatory bowel disease. Am J Physiol Gastrointest Liver Physiol 310:G460–G476. https://doi.org/10.1152/ajpgi.00369.2015
Mali P, Yang L, Esvelt KM, Aach J, Guell M, DiCarlo JE, Norville JE, Church GM (2013) RNA-guided human genome engineering via Cas9. Science 339:823–826. https://doi.org/10.1126/science.1232033
Marsh R, Dos Santos C, Hanson L, Ng C, Major G, Smyth AR, Rivett D, van der Gast C (2023) Tezacaftor/ivacaftor therapy has negligible effects on the cystic fibrosis gut microbiome. Microbiol Spectr 11:e0117523. https://doi.org/10.1128/spectrum.01175-23
Marshall BJ, Warren JR (1984) Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet 1:1311–1315. https://doi.org/10.1016/s0140-6736(84)91816-6
McCole DF, Barrett KE (2003) Epithelial transport and gut barrier function in colitis. Curr Opin Gastroenterol 19:578–582. https://doi.org/10.1097/00001574-200311000-00011
McHugh DR, Cotton CU, Moss FJ, Vitko M, Valerio DM, Kelley TJ, Hao S, Jafri A, Drumm ML, Boron WF, Stern RC, McBennett K, Hodges CA (2018) Linaclotide improves gastrointestinal transit in cystic fibrosis mice by inhibiting sodium/hydrogen exchanger 3. Am J Physiol Gastrointest Liver Physiol 315:G868–G878. https://doi.org/10.1152/ajpgi.00261.2017
Megalaa R, Gopalareddy V, Champion E, Goralski JL (2019) Time for a gut check: pancreatic sufficiency resulting from CFTR modulator use. Pediatr Pulmonol 54:E16–E18. https://doi.org/10.1002/ppul.24353
Melvin JE, Park K, Richardson L, Schultheis PJ, Shull GE (1999) Mouse down-regulated in adenoma (DRA) is an intestinal Cl(-)/HCO(3)(-) exchanger and is up-regulated in colon of mice lacking the NHE3 Na(+)/H(+) exchanger. J Biol Chem 274:22855–22861. https://doi.org/10.1074/jbc.274.32.22855
Moseley RH, Höglund P, Wu GD, Silberg DG, Haila S, de la Chapelle A, Holmberg C, Kere J (1999) Downregulated in adenoma gene encodes a chloride transporter defective in congenital chloride diarrhea. Am J Physiol 276:G185–G192. https://doi.org/10.1152/ajpgi.1999.276.1.G185
Nedjadi T, Moran AW, Al-Rammahi MA, Shirazi-Beechey SP (2014) Characterization of butyrate transport across the luminal membranes of equine large intestine. Exp Physiol 99:1335–1347. https://doi.org/10.1113/expphysiol.2014.077982
Nikolovska K, Tytmonas E, Seidler A, di Stefano G, Voigtländer T, Hellms T, Lenzen H, Seidler U (2023) Altered colonocyte differentiation may lead to decreased electrolyte and fluid absorption in the ileocolon of IBD patients by affecting the expression pattern of the responsible ion transporters. Physiology 38. https://doi.org/10.1152/physiol.2023.38.S1.5732076
Norsa L, Berni Canani R, Duclaux-Loras R, Bequet E, Köglmeier J, Russell RK, Uhlig HH, Travis S, Hollis J, Koletzko S, Grimaldi G, Castaldo G, Rodrigues A, Deflandre J, Dembinski L, Shah N, Heinz-Erian P, Janecke A, Leskinen S, Wedenoja S, Koskela R, Lachaux A, Kolho K-L, Ruemmele FM (2021) Inflammatory bowel disease in patients with congenital chloride diarrhoea. J Crohns Colitis 15:1679–1685. https://doi.org/10.1093/ecco-jcc/jjab056
Nugent SG, Kumar D, Rampton DS, Evans DF (2001) Intestinal luminal pH in inflammatory bowel disease: possible determinants and implications for therapy with aminosalicylates and other drugs. Gut 48:571–577. https://doi.org/10.1136/gut.48.4.571
Ohana E, Yang D, Shcheynikov N, Muallem S (2009) Diverse transport modes by the solute carrier 26 family of anion transporters. J Physiol 587:2179–2185. https://doi.org/10.1113/jphysiol.2008.164863
Okamura N, Tajima Y, Soejima A, Masuda H, Sugita Y (1985) Sodium bicarbonate in seminal plasma stimulates the motility of mammalian spermatozoa through direct activation of adenylate cyclase. J Biol Chem 260:9699–9705. https://doi.org/10.1016/s0021-9258(17)39295-5
Page AJ, Brierley SM, Martin CM, Price MP, Symonds E, Butler R, Wemmie JA, Blackshaw LA (2005) Different contributions of ASIC channels 1a, 2, and 3 in gastrointestinal mechanosensory function. Gut 54:1408–1415. https://doi.org/10.1136/gut.2005.071084
Palazon A, Goldrath AW, Nizet V, Johnson RS (2014) HIF transcription factors, inflammation, and immunity. Immunity 41:518–528. https://doi.org/10.1016/j.immuni.2014.09.008
Park HW, Nam JH, Kim JY, Namkung W, Yoon JS, Lee J-S, Kim KS, Venglovecz V, Gray MA, Kim KH, Lee MG (2010) Dynamic regulation of CFTR bicarbonate permeability by [Cl-]i and its role in pancreatic bicarbonate secretion. Gastroenterology 139:620–631. https://doi.org/10.1053/j.gastro.2010.04.004
Patterson LM, Zheng H, Ward SM, Berthoud HR (2003) Vanilloid receptor (VR1) expression in vagal afferent neurons innervating the gastrointestinal tract. Cell Tissue Res 311:277–287. https://doi.org/10.1007/s00441-002-0682-0
Pavlov I (1904) Nobel lecture. NobelPrize.org. Nobel Prize Outreach AB 2023. https://www.nobelprize.org/prizes/medicine/1904/pavlov/lecture/. 13 Nov 2023
Poulsen JH, Fischer H, Illek B, Machen TE (1994) Bicarbonate conductance and pH regulatory capability of cystic fibrosis transmembrane conductance regulator. Proc Natl Acad Sci U S A 91:5340–5344. https://doi.org/10.1073/pnas.91.12.5340
Press AG, Hauptmann IA, Hauptmann L, Fuchs B, Fuchs M, Ewe K, Ramadori G (1998) Gastrointestinal pH profiles in patients with inflammatory bowel disease. Aliment Pharmacol Ther 12:673–678. https://doi.org/10.1046/j.1365-2036.1998.00358.x
Priyamvada S, Anbazhagan AN, Kumar A, Chatterjee I, Borthakur A, Saksena S, Gill RK, Alrefai WA, Dudeja PK (2020) All-trans retinoic acid counteracts diarrhea and inhibition of downregulated in adenoma expression in gut inflammation. Inflamm Bowel Dis 26:534–545. https://doi.org/10.1093/ibd/izz249
Radu CG, Nijagal A, McLaughlin J, Wang L, Witte ON (2005) Differential proton sensitivity of related G protein-coupled receptors T cell death-associated gene 8 and G2A expressed in immune cells. Proc Natl Acad Sci U S A 102:1632–1637. https://doi.org/10.1073/pnas.0409415102
Riegler M, Feil W, Wenzl E, Schiessel R (1991) Factors influencing the restitution of the duodenal and colonic mucosa after damage. J Physiol Pharmacol 42:61–71
Romero MF, Chang M-H, Plata C, Zandi-Nejad K, Mercado A, Broumand V, Sussman CR, Mount DB (2006) Physiology of electrogenic SLC26 paralogues. Novartis Found Symp 273:126–38
Romero MF, Chen AP, Parker MD, Boron WF (2013) The SLC4 family of bicarbonate (HCO3-) transporters. Mol Aspects Med 34:159–182. https://doi.org/10.1016/j.mam.2012.10.008
Roussa E, Alper SL, Thévenod F (2001) Immunolocalization of anion exchanger AE2, Na(+)/H(+) exchangers NHE1 and NHE4, and vacuolar type H(+)-ATPase in rat pancreas. J Histochem Cytochem 49:463–474. https://doi.org/10.1177/002215540104900406
Sabbatini ME, Gorelick F, Glaser S (2014) Adenylyl cyclases in the digestive system. Cell Signal 26:1173–1181. https://doi.org/10.1016/j.cellsig.2014.01.033
Saint-Criq V, Haq IJ, Gardner AI, Garnett JP, Ward C, Brodlie M, Gray MA (2019) Real-time, semi-automated fluorescent measurement of the airway surface liquid pH of primary human airway epithelial cells. J Vis Exp. https://doi.org/10.3791/59815
Salari A, Zhou K, Nikolovska K, Seidler U, Amiri M (2023) Human colonoid-myofibroblast coculture for study of apical Na+/H+ exchangers of the lower cryptal neck region. Int J Mol Sci 24. https://doi.org/10.3390/ijms24054266
Sanderlin EJ, Leffler NR, Lertpiriyapong K, Cai Q, Hong H, Bakthavatchalu V, Fox JG, Oswald JZ, Justus CR, Krewson EA, O’Rourke D, Yang LV (2017) GPR4 deficiency alleviates intestinal inflammation in a mouse model of acute experimental colitis. Biochim Biophys Acta - Mol Basis Dis 1863:569–584. https://doi.org/10.1016/j.bbadis.2016.12.005
Sanderlin EJ, Marie M, Velcicky J, Loetscher P, Yang LV (2019) Pharmacological inhibition of GPR4 remediates intestinal inflammation in a mouse colitis model. Eur J Pharmacol 852:218–230. https://doi.org/10.1016/j.ejphar.2019.03.038
Sarthi JB, Trumbull AM, Abazari SM, van Unen V, Chan JE, Joo NS, Jiang Y, Kuo CJ, Sellers ZM (2023) Critical role of down-regulated in adenoma bicarbonate transporter in linaclotide stimulated intestinal bicarbonate secretion. bioRxiv Prepr Serv Biol 315:G868. https://doi.org/10.1101/2023.05.05.539132
Sato T, Clevers H (2013) Growing self-organizing mini-guts from a single intestinal stem cell: mechanism and applications. Science 340:1190–1194. https://doi.org/10.1126/science.1234852
Schultheiss G, Hörger S, Diener M (1998) The bumetanide-resistant part of forskolin-induced anion secretion in rat colon. Acta Physiol Scand 164:219–228
Schweinfest CW, Henderson KW, Suster S, Kondoh N, Papas TS (1993) Identification of a colon mucosa gene that is down-regulated in colon adenomas and adenocarcinomas. Proc Natl Acad Sci U S A 90:4166–4170. https://doi.org/10.1073/pnas.90.9.4166
Schweinfest CW, Spyropoulos DD, Henderson KW, Kim J-H, Chapman JM, Barone S, Worrell RT, Wang Z, Soleimani M (2006) slc26a3 (dra)-deficient mice display chloride-losing diarrhea, enhanced colonic proliferation, and distinct up-regulation of ion transporters in the colon. J Biol Chem 281:37962–37971. https://doi.org/10.1074/jbc.M607527200
Seidler UE (2013) Gastrointestinal HCO3- transport and epithelial protection in the gut: new techniques, transport pathways and regulatory pathways. Curr Opin Pharmacol 13:900–908. https://doi.org/10.1016/j.coph.2013.10.001
Seidler U, Nikolovska K (2019) Slc26 family of anion transporters in the gastrointestinal tract: expression, function, regulation, and role in disease. Compr Physiol 9:839–872. https://doi.org/10.1002/cphy.c180027
Seidler U, Blumenstein I, Kretz A, Viellard-Baron D, Rossmann H, Colledge WH, Evans M, Ratcliff R, Gregor M (1997) A functional CFTR protein is required for mouse intestinal cAMP-, cGMP- and Ca(2+)-dependent HCO3- secretion. J Physiol 505(2):411–23. https://doi.org/10.1111/j.1469-7793.1997.411bb.x
Seidler U, Lenzen H, Cinar A, Tessema T, Bleich A, Riederer B (2006) Molecular mechanisms of disturbed electrolyte transport in intestinal inflammation. Ann N Y Acad Sci 1072:262–275. https://doi.org/10.1196/annals.1326.024
Seidler U, Rottinghaus I, Hillesheim J, Chen M, Riederer B, Krabbenhöft A, Engelhardt R, Wiemann M, Wang Z, Barone S, Manns MP, Soleimani M (2008) Sodium and chloride absorptive defects in the small intestine in Slc26a6 null mice. Pflugers Arch 455:757–766. https://doi.org/10.1007/s00424-007-0318-z
Sellers ZM, Childs D, Chow JYC, Smith AJ, Hogan DL, Isenberg JI, Dong H, Barrett KE, Pratha VS (2005) Heat-stable enterotoxin of Escherichia coli stimulates a non-CFTR-mediated duodenal bicarbonate secretory pathway. Am J Physiol Gastrointest Liver Physiol 288:G654–G663. https://doi.org/10.1152/ajpgi.00386.2004
Shao X-X, Lin D-P, Sun L, Wu C-Q, Yang W, Jiang Y (2018) Association of ulcerative colitis with solute-linked carrier family 26 member A3 gene polymorphisms and its expression in colonic tissues in Chinese patients. Int J Colorectal Dis 33:1169–1172. https://doi.org/10.1007/s00384-018-3097-4
Shcheynikov N, Wang Y, Park M, Ko SBH, Dorwart M, Naruse S, Thomas PJ, Muallem S (2006) Coupling modes and stoichiometry of Cl-/HCO3- exchange by slc26a3 and slc26a6. J Gen Physiol 127:511–524. https://doi.org/10.1085/jgp.200509392
Simpson JE, Schweinfest CW, Shull GE, Gawenis LR, Walker NM, Boyle KT, Soleimani M, Clarke LL (2007) PAT-1 (Slc26a6) is the predominant apical membrane Cl-/HCO3- exchanger in the upper villous epithelium of the murine duodenum. Am J Physiol Gastrointest Liver Physiol 292:G1079–G1088. https://doi.org/10.1152/ajpgi.00354.2006
Simpson JE, Walker NM, Supuran CT, Soleimani M, Clarke LL (2010) Putative anion transporter-1 (Pat-1, Slc26a6) contributes to intracellular pH regulation during H+-dipeptide transport in duodenal villous epithelium. Am J Physiol Gastrointest Liver Physiol 298:G683–G691. https://doi.org/10.1152/ajpgi.00293.2009
Simson JN, Merhav A, Silen W (1981) Alkaline secretion by amphibian duodenum I General characteristics. Am J Physiol 240:G401–G408. https://doi.org/10.1152/ajpgi.1981.240.5.G401
Singh AK, Sjöblom M, Zheng W, Krabbenhöft A, Riederer B, Rausch B, Manns MP, Soleimani M, Seidler U (2008) CFTR and its key role in in vivo resting and luminal acid-induced duodenal HCO3- secretion. Acta Physiol (Oxf) 193:357–365. https://doi.org/10.1111/j.1748-1716.2008.01854.x
Singh AK, Amlal H, Haas PJ, Dringenberg U, Fussell S, Barone SL, Engelhardt R, Zuo J, Seidler U, Soleimani M (2008) Fructose-induced hypertension: essential role of chloride and fructose absorbing transporters PAT1 and Glut5. Kidney Int 74:438–447. https://doi.org/10.1038/ki.2008.184
Singh AK, Riederer B, Chen M, Xiao F, Krabbenhöft A, Engelhardt R, Nylander O, Soleimani M, Seidler U (2010) The switch of intestinal Slc26 exchangers from anion absorptive to HCOFormula secretory mode is dependent on CFTR anion channel function. Am J Physiol Cell Physiol 298:C1057–C1065. https://doi.org/10.1152/ajpcell.00454.2009
Singh AK, Xia W, Riederer B, Juric M, Li J, Zheng W, Cinar A, Xiao F, Bachmann O, Song P, Praetorius J, Aalkjaer C, Seidler U (2013) Essential role of the electroneutral Na+-HCO3- cotransporter NBCn1 in murine duodenal acid-base balance and colonic mucus layer build-up in vivo. J Physiol 591:2189–2204. https://doi.org/10.1113/jphysiol.2012.247874
Sisignano M, Fischer MJM, Geisslinger G (2021) Proton-sensing GPCRs in health and disease. Cells 10. https://doi.org/10.3390/cells10082050
Sivaprakasam S, Bhutia YD, Yang S, Ganapathy V (2017) Short-chain fatty acid transporters: role in colonic homeostasis. Compr Physiol 8:299–314. https://doi.org/10.1002/cphy.c170014
Sjöblom M, Singh AK, Zheng W, Wang J, Tuo B, Krabbenhöft A, Riederer B, Gros G, Seidler U (2009) Duodenal acidity “sensing” but not epithelial HCO3- supply is critically dependent on carbonic anhydrase II expression. Proc Natl Acad Sci U S A 106:13094–13099. https://doi.org/10.1073/pnas.0901488106
Storozhuk M, Cherninskyi A, Maximyuk O, Isaev D, Krishtal O (2021) Acid-sensing ion channels: focus on physiological and some pathological roles in the brain. Curr Neuropharmacol 19:1570–1589. https://doi.org/10.2174/1570159x19666210125151824
Stumpff F (2018) A look at the smelly side of physiology: transport of short chain fatty acids. Pflugers Arch 470(4):571–598
Sugiura T, Dang K, Lamb K, Bielefeldt K, Gebhart GF (2005) Acid-sensing properties in rat gastric sensory neurons from normal and ulcerated stomach. J Neurosci 25:2617–2627. https://doi.org/10.1523/JNEUROSCI.2894-04.2005
Talbot C, Lytle C (2010) Segregation of Na/H exchanger-3 and Cl/HCO3 exchanger SLC26A3 (DRA) in rodent cecum and colon. Am J Physiol Gastrointest Liver Physiol 299:G358–G367. https://doi.org/10.1152/ajpgi.00151.2010
Tan Q, di Stefano G, Tan X, Renjie X, Römermann D, Talbot SR, Seidler UE (2021) Inhibition of Na+ /H+ exchanger isoform 3 improves gut fluidity and alkalinity in cystic fibrosis transmembrane conductance regulator-deficient and F508del mutant mice. Br J Pharmacol 178:1018–1036. https://doi.org/10.1111/bph.15323
Tan X, Kini A, Römermann D, Seidler U (2022) The NHE3 inhibitor tenapanor prevents intestinal obstructions in CFTR-deleted mice. Int J Mol Sci 23. https://doi.org/10.3390/ijms23179993
Tang L, Fatehi M, Linsdell P (2009) Mechanism of direct bicarbonate transport by the CFTR anion channel. J Cyst Fibros 8:115–121. https://doi.org/10.1016/j.jcf.2008.10.004
Thompson CA, DeLaForest A, Battle MA (2018) Patterning the gastrointestinal epithelium to confer regional-specific functions. Dev Biol 435:97–108. https://doi.org/10.1016/j.ydbio.2018.01.006
Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D (1998) The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 21:531–543. https://doi.org/10.1016/S0896-6273(00)80564-4
Tresguerres M, Levin LR, Buck J, Grosell M (2010) Modulation of NaCl absorption by [HCO3-] in the marine teleost intestine is mediated by soluble adenylyl cyclase. Am J Physiol - Regul Integr Comp Physiol 299:62–71. https://doi.org/10.1152/ajpregu.00761.2009
Tse C-M, Yin J, Singh V, Sarker R, Lin R, Verkman AS, Turner JR, Donowitz M (2019) cAMP stimulates SLC26A3 activity in human colon by a CFTR-dependent mechanism that does not require CFTR activity. Cell Mol Gastroenterol Hepatol 7:641–653. https://doi.org/10.1016/j.jcmgh.2019.01.002
Tuo B, Riederer B, Wang Z, Colledge WH, Soleimani M, Seidler U (2006) Involvement of the anion exchanger SLC26A6 in prostaglandin E2- but not forskolin-stimulated duodenal HCO3- secretion. Gastroenterology 130:349–358. https://doi.org/10.1053/j.gastro.2005.10.017
Turnberg LA (1971) Abnormalities in intestinal electrolyte transport in congenital chloridorrhoea. Gut 12:544–551. https://doi.org/10.1136/gut.12.7.544
Turnberg LA, Fordtran JS, Carter NW, Rector FC (1970) Mechanism of bicarbonate absorption and its relationship to sodium transport in the human jejunum. J Clin Invest 49:548–556. https://doi.org/10.1172/JCI106265
Umesaki Y, Yajima T, Yokokura T, Mutai M (1979) Effect of organic acid absorption on bicarbonate transport in rat colon. Pflugers Arch 379:43–47. https://doi.org/10.1007/BF00622903
Vann KT, Xiong ZG (2018) Acid-sensing ion channel 1 contributes to normal olfactory function. Behav Brain Res 337:246–251. https://doi.org/10.1016/j.bbr.2017.09.014
Vidyasagar S, Barmeyer C, Geibel J, Binder HJ, Rajendran VM (2005) Role of short-chain fatty acids in colonic HCO(3) secretion. Am J Physiol Gastrointest Liver Physiol 288:G1217–G1226. https://doi.org/10.1152/ajpgi.00415.2004
Visconti PE, Muschietti JP, Flawia MM, Tezon JG (1990) Bicarbonate dependence of cAMP accumulation induced by phorbol esters in hamster spermatozoa. BBA - Mol Cell Res 1054:231–236. https://doi.org/10.1016/0167-4889(90)90246-A
Waldmann R, Champigny G, Bassilana F, Heurteaux C, Lazdunski M (1997) A proton-gated cation channel involved in acid-sensing. Nature 386:173–177. https://doi.org/10.1038/386173a0
Walker NM, Simpson JE, Levitt RC, Boyle KT, Clarke LL (2006) Talniflumate increases survival in a cystic fibrosis mouse model of distal intestinal obstructive syndrome. J Pharmacol Exp Ther 317:275–283. https://doi.org/10.1124/jpet.105.094847
Walker NM, Simpson JE, Brazill JM, Gill RK, Dudeja PK, Schweinfest CW, Clarke LL (2009) Role of down-regulated in adenoma anion exchanger in HCO3- secretion across murine duodenum. Gastroenterology 136:893–901. https://doi.org/10.1053/j.gastro.2008.11.016
Walker NM, Simpson JE, Hoover EE, Brazill JM, Schweinfest CW, Soleimani M, Clarke LL (2011) Functional activity of Pat-1 (Slc26a6) Cl(−)/HCOa (−) exchange in the lower villus epithelium of murine duodenum. Acta Physiol 201:21–31. https://doi.org/10.1111/j.1748-1716.2010.02210.x
Wang Z, Petrovic S, Mann E, Soleimani M (2002) Identification of an apical Cl(-)/HCO3(-) exchanger in the small intestine. Am J Physiol Gastrointest Liver Physiol 282:G573–G579. https://doi.org/10.1152/ajpgi.00338.2001
Wang Z, Wang T, Petrovic S, Tuo B, Riederer B, Barone S, Lorenz JN, Seidler U, Aronson PS, Soleimani M (2005) Renal and intestinal transport defects in Slc26a6-null mice. Am J Physiol Cell Physiol 288:C957–C965. https://doi.org/10.1152/ajpcell.00505.2004
Wang Y, Soyombo AA, Shcheynikov N, Zeng W, Dorwart M, Marino CR, Thomas PJ, Muallem S (2006) Slc26a6 regulates CFTR activity in vivo to determine pancreatic duct HCO3- secretion: relevance to cystic fibrosis. EMBO J 25:5049–5057. https://doi.org/10.1038/sj.emboj.7601387
Wang Y, de Vallière C, Imenez Silva PH, Leonardi I, Gruber S, Gerstgrasser A, Melhem H, Weber A, Leucht K, Wolfram L, Hausmann M, Krieg C, Thomasson K, Boyman O, Frey-Wagner I, Rogler G, Wagner CA (2018) The proton-activated receptor GPR4 modulates intestinal inflammation. J Crohn’s Colitis 12:355–369. https://doi.org/10.1093/ecco-jcc/jjx147
Wang Y, Huang X, Zhou G, Han J, Xie Z, Zhang M, Li X, Wu Q-R, Li L, Ye Z, Chen M, Qiu Y, Zhang S (2023) A novel nomogram combining mucus barrier index for predicting treatment failures in ulcerative colitis. J Inflamm Res 16:1879–1894. https://doi.org/10.2147/JIR.S410057
Wedenoja S, Pekansaari E, Höglund P, Mäkelä S, Holmberg C, Kere J (2011) Update on SLC26A3 mutations in congenital chloride diarrhea. Hum Mutat 32:715–722. https://doi.org/10.1002/humu.21498
Wedenoja S, Saarikivi A, Mälkönen J, Leskinen S, Lehto M, Adeshara K, Tuokkola J, Nikkonen A, Merras-Salmio L, Höyhtyä M, Hörkkö S, Haaramo A, Salonen A, de Vos WM, Korpela K, Kolho K-L (2022) Fecal microbiota in congenital chloride diarrhea and inflammatory bowel disease. PLoS ONE 17:e0269561. https://doi.org/10.1371/journal.pone.0269561
Wemmie JA, Chen J, Askwith CC, Hruska-Hageman AM, Price MP, Nolan BC, Yoder PG, Lamani E, Hoshi T, Freeman JH, Welsh MJ (2002) The acid-activated ion channel ASIC contributes to synaptic plasticity, learning, and memory. Neuron 34:463–477. https://doi.org/10.1016/S0896-6273(02)00661-X
Wemmie JA, Coryell MW, Askwith CC, Lamani E, Leonard AS, Sigmund CD, Welsh MJ (2004) Overexpression of acid-sensing ion channel 1a in transgenic mice increases acquired fear-related behavior. Proc Natl Acad Sci U S A 101:3621–3626. https://doi.org/10.1073/pnas.0308753101
Wemmie JA, Price MP, Welsh MJ (2006) Acid-sensing ion channels: advances, questions and therapeutic opportunities. Trends Neurosci 29:578–586. https://doi.org/10.1016/j.tins.2006.06.014
Wilson RW, Wilson JM, Grosell M (2002) Intestinal bicarbonate secretion by marine teleost fish - why and how? Biochim Biophys Acta - Biomembr 1566:182–193. https://doi.org/10.1016/S0005-2736(02)00600-4
Xia W, Yu Q, Riederer B, Singh AK, Engelhardt R, Yeruva S, Song P, Tian D-A, Soleiman M, Seidler U (2014) The distinct roles of anion transporters Slc26a3 (DRA) and Slc26a6 (PAT-1) in fluid and electrolyte absorption in the murine small intestine. Pflugers Arch 466:1541–1556. https://doi.org/10.1007/s00424-013-1381-2
Xiao F, Li J, Singh AK, Riederer B, Wang J, Sultan A, Park H, Lee MG, Lamprecht G, Scholte BJ, De Jonge HR, Seidler U (2012) Rescue of epithelial HCO3- secretion in murine intestine by apical membrane expression of the cystic fibrosis transmembrane conductance regulator mutant F508del. J Physiol 590:5317–5334. https://doi.org/10.1113/jphysiol.2012.232124
Xiao F, Juric M, Li J, Riederer B, Yeruva S, Singh AK, Zheng L, Glage S, Kollias G, Dudeja P, Tian D-A, Xu G, Zhu J, Bachmann O, Seidler U (2012) Loss of downregulated in adenoma (DRA) impairs mucosal HCO3(-) secretion in murine ileocolonic inflammation. Inflamm Bowel Dis 18:101–111. https://doi.org/10.1002/ibd.21744
Xiao F, Yu Q, Li J, Johansson MEV, Singh AK, Xia W, Riederer B, Engelhardt R, Montrose M, Soleimani M, Tian DA, Xu G, Hansson GC, Seidler U (2014) Slc26a3 deficiency is associated with loss of colonic HCO3 (-) secretion, absence of a firm mucus layer and barrier impairment in mice. Acta Physiol (Oxf) 211:161–175. https://doi.org/10.1111/apha.12220
Xue H-H, Li J-J, Li S-F, Guo J, Yan R-P, Chen T-G, Shi X-H, Wang J-D, Zhang L-W (2023) Phillygenin attenuated colon inflammation and improved intestinal mucosal barrier in DSS-induced colitis mice via TLR4/Src mediated MAPK and NF-κB signaling pathways. Int J Mol Sci 24. https://doi.org/10.3390/ijms24032238
Yamaguchi M, Steward MC, Smallbone K, Sohma Y, Yamamoto A, Ko SBH, Kondo T, Ishiguro H (2017) Bicarbonate-rich fluid secretion predicted by a computational model of guinea-pig pancreatic duct epithelium. J Physiol 595:1947–1972. https://doi.org/10.1113/JP273306
Yang D, Shcheynikov N, Zeng W, Ohana E, So I, Ando H, Mizutani A, Mikoshiba K, Muallem S (2009) IRBIT coordinates epithelial fluid and HCO3- secretion by stimulating the transporters pNBC1 and CFTR in the murine pancreatic duct. J Clin Invest 119:193–202. https://doi.org/10.1172/JCI36983
Yao CK, Burgell RE, Taylor KM, Ward MG, Friedman AB, Barrett JS, Muir JG, Gibson PR (2021) Effects of fiber intake on intestinal pH, transit, and predicted oral mesalamine delivery in patients with ulcerative colitis. J Gastroenterol Hepatol 36:1580–1589. https://doi.org/10.1111/jgh.15311
Yermolaieva O, Leonard AS, Schnizler MK, Abboud FM, Welsh MJ (2004) Extracellular acidosis increases neuronal cell calcium by activating acid-sensing ion channel 1a. Proc Natl Acad Sci U S A 101:6752–6757. https://doi.org/10.1073/pnas.0308636100
Yu Q (2021) Slc26a3 (DRA) in the gut: expression, function, regulation, role in infectious diarrhea and inflammatory bowel disease. Inflamm Bowel Dis 27:575–584. https://doi.org/10.1093/ibd/izaa256
Yu Q, Liu X, Liu Y, Riederer B, Li T, Tian D-A, Tuo B, Shull G, Seidler U (2016) Defective small intestinal anion secretion, dipeptide absorption, and intestinal failure in suckling NBCe1-deficient mice. Pflugers Arch 468:1419–1432. https://doi.org/10.1007/s00424-016-1836-3
Yu X, Yu M, Liu Y, Yu S (2016) TRP channel functions in the gastrointestinal tract. Semin Immunopathol 38:385–396. https://doi.org/10.1007/s00281-015-0528-y
Zhang N, Heruth DP, Wu W, Zhang LQ, Nsumu MN, Shortt K, Li K, Jiang X, Wang B, Friesen C, Li D-Y, Ye SQ (2019) Functional characterization of SLC26A3 c.392C>G (p.P131R) mutation in intestinal barrier function using CRISPR/CAS9-created cell models. Cell Biosci 9:40. https://doi.org/10.1186/s13578-019-0303-1
Zhang L, Zheng L, Yang X, Yao S, Wang H, An J, Jin H, Wen G, Tuo B (2022) Pathology and physiology of acid-sensitive ion channels in the digestive system (Review). Int J Mol Med 50. https://doi.org/10.3892/IJMM.2022.5150
Zippin JH, Chen Y, Nahirney P, Kamenetsky M, Wuttke MS, Fischman DA, Levin LR, Buck J (2003) Compartmentalization of bicarbonate-sensitive adenylyl cyclase in distinct signaling microdomains. FASEB J 17:82–84. https://doi.org/10.1096/fj.02-0598fje
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
H.M.B. and U.E.S. wrote the manuscript
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on Physiology of systemic and cellular pH regulation in Pflügers Archiv—European Journal of Physiology.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Becker, H.M., Seidler, U.E. Bicarbonate secretion and acid/base sensing by the intestine. Pflugers Arch - Eur J Physiol 476, 593–610 (2024). https://doi.org/10.1007/s00424-024-02914-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-024-02914-3