Abstract
Aim
This study reports venous thromboembolism (VTE) rates following colectomy for diverticular disease to explore the magnitude of postoperative VTE risk in this population and identify high risk subgroups of interest.
Method
English national cohort study of colectomy patients between 2000 and 2019 using linked primary (Clinical Practice Research Datalink) and secondary (Hospital Episode Statistics) care data. Stratified by admission type, absolute incidence rates (IR) per 1000 person-years and adjusted incidence rate ratios (aIRR) were calculated for 30- and 90-day post-colectomy VTE.
Results
Of 24,394 patients who underwent colectomy for diverticular disease, over half (57.39%) were emergency procedures with the highest VTE rate seen in patients ≥70-years-old (IR 142.27 per 1000 person-years, 95%CI 118.32–171.08) at 30 days post colectomy. Emergency resections (IR 135.18 per 1000 person-years, 95%CI 115.72–157.91) had double the risk (aIRR 2.07, 95%CI 1.47–2.90) of developing a VTE at 30 days following colectomy compared to elective resections (IR 51.14 per 1000 person-years, 95%CI 38.30–68.27). Minimally invasive surgery (MIS) was shown to be associated with a 64% reduction in VTE risk (aIRR 0.36 95%CI 0.20–0.65) compared to open colectomies at 30 days post-op. At 90 days following emergency resections, VTE risks remained raised compared to elective colectomies.
Conclusion
Following emergency colectomy for diverticular disease, the VTE risk is approximately double compared to elective resections at 30 days while MIS was found to be associated with a reduced risk of VTE. This suggests advancements in postoperative VTE prevention in diverticular disease patients should focus on those undergoing emergency colectomies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diverticular disease is one of the main indications for colectomy in both the emergency and elective setting [1, 2]. This condition and its complications are becoming more common with increasing hospital admissions being reported in the United States of America (US) and United Kingdom (UK) [3,4,5]. Following this rise in complications of diverticular disease, the rates of elective colectomies for diverticulitis have subsequently increased by 29% over a 7-year period [6, 7].
Current literature reports patients with diverticular disease and those undergoing colorectal surgery, especially as an emergency procedure are at a greater risk of postoperative venous thromboembolism (VTE) [8,9,10,11]. Therefore, VTE rates are expected to be high in this group [12]. However, recent changes in perioperative care such as the increased use of minimally invasive surgery (MIS) and enhanced recovery after surgery (ERAS) guidelines may have affected VTE risk. Current guidelines on VTE prevention following colectomy, used globally in standard practice, target patient groups who are known to be at high risk for VTE such as those with cancer and to a lesser extent Inflammatory Bowel Disease (IBD) [13]. However, there is a paucity of guidance for patients being managed surgically for benign abdominal disease, in particular diverticulitis, with no specific guidance on extended thromboprophylaxis in this group [14, 15]. With cases of surgically managed diverticular disease rising worldwide, this gap in the guidelines could leave patients at significant risk.
Existing studies explore VTE rates following colectomy [16,17,18,19]; however, reports on VTE following surgical management of diverticular disease are scarce. This novel study uses longer follow up timeframes as well as explores the effect of MIS techniques on colectomy for diverticular disease to supplement the current literature [9, 12, 20,21,22,23,24]. The aim of this study was to explore the rates of VTE in patients undergoing surgery for diverticular disease and determine at risk subgroups to inform current guidelines.
Methods
The study was approved by the Independent Scientific Advisory Committee approval board (Protocol 19_180RA3).
Data sources
Three validated and linked healthcare databases were used for this study: The Clinical Practice Research Datalink (CPRD) GOLD, CPRD Aurum and Hospital Episode Statistics Admitted Patient Care (HES APC) databases [25,26,27]. The CPRD databases house primary care data including diagnoses, referrals and prescriptions for 60 million patients collected from General Practitioner practices across the UK [28]. The HES APC database records all admissions to National Health Service (NHS) and independent sector hospitals. Patient admission data regarding discharge diagnosis and procedures are coded using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) codes and the Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures version 4 (OPCS-4) codes respectively [29, 30].
Cohort
OPCS-4 codes from HES data linked to CPRD GOLD and Aurum practices were used to identify patients that underwent colectomy between the years 2000 and 2019. Patient data had to meet the research standard and have coinciding data collection time periods for both primary and secondary databases to be included within the validated cohort. Patients with diverticular disease undergoing colectomy were identified using the HES ICD-10 codes (see Supplementary 1). The exclusion criteria used encompassed completely endoscopic operations, those confined to the anal canal, patients less than 18 years old and those with previous personal history of VTE. Patients identified as having a VTE event prior to colectomy were excluded due to their inherently increased risk of VTE [31] as outlined in the patient flow chart (see supplementary 1). Person-time and postoperative follow-up started the day after the date of operation. All follow-up lasted until earliest date of VTE event, death, and change to a non-participating general practice or 90 days from the date of operation.
Exposures
The main exposures of interest were admission type, sex, operative technique, and co-morbidity. From HES data, admission type was classified as either elective or emergency. For emergency admissions, those with diverticular disease with perforation and/or abscess were included using ICD-10 codes (Supplementary 1) and were classed as perforated or not perforated. Operative technique included colectomies that were carried out open or started using a minimally invasive approach. Minimally invasive techniques were defined as laparoscopic or robotic surgery using OPCS-4 codes (Y50.8, Y57.1, and Y75.2) and (Y75.3) respectively. Defined from HES data, sex was either male or female and length of stay was the time in days from date of operation to discharge. Patients who had stomas were defined using OPCS-4 codes and patient age in years at colectomy was categorized into <60, 60–69, and ≥70. CPRD and HES data reported patient co-morbidity using the Charlson score with categories 0, 1, and ≥2 co-morbidities [30].
Outcomes
A diagnosis of a post-colectomy VTE event was the primary outcome. Post-colectomy VTE was defined as a VTE event occurring after colectomy from either medical or ICD-10 codes in the linked CPRD and HES datasets. To be considered valid VTE events, evidence of treatment in an anticoagulation clinic (for example a medical code) within a period of 15 days before and 90 days after VTE diagnosis, a prescription for anticoagulant medication or a date of death within 30 days of the event was required. Furthermore, VTE diagnosis also included instances where VTE was identified as an underlying cause of death and only the first confirmed VTE event was included within the analysis. This definition using primary care data has been formerly validated [19] and used in previous studies [27].
Statistical analysis
Cohort demographics were presented as proportions and stratified by admission type. Absolute incidence rates (IR) of VTE were calculated per 1000 person-years with 95% confidence intervals (95%CI). Post-colectomy VTE rates and adjusted incidence rate ratios (aIRR) for linear trend at 30 and 90 days post colectomy, adjusted for age, sex, co-morbidity, admission type, and operative technique were calculated using Poisson regression and stratified a priori where possible by admission type. For emergency admissions, the calculated VTE rates and aIRR were also adjusted for perforation and abscess. The cumulative incidence of VTE was calculated up to 90 days using Kaplan-Meier curves.
All data management and analyses were performed using Stata SE® version 17.0 (StataCorp LLC, College Station, Texas, USA).
Results
Cohort demographics
Of 24,394 patients who underwent colectomy for diverticular disease, over half (57.39%) were performed as emergency procedures. These patients were older (≥70 years old 45.22%) and had ≥2 significant co-morbidities (53.08%). There was a similar number of male and female patients undergoing colectomy as an emergency (43.68% vs 56.32%) or elective (44.14% vs 55.86%) procedure. In the emergency setting, 78.61% of patients undergoing colectomy had a stoma while 25.03% of patients had a stoma in the elective group. Overall, the open operative technique was used more frequently in both emergency (91.64%) and elective (64.08%) settings. (See Table 1) However, over the study period there was a notable rise in the rates of MIS. In the elective population, MIS rates increased from 0.87% in the year 2000 to 68.47% (p<0.0001) in 2019. Similarly, the rate of emergency MIS in 2000 was 0.22% and by 2019 was 18.87% (p<0.0001). The median length of stay in the elective and emergency groups were 8 (Interquartile range (IQR) 6–12) days and 13 (IQR 8–22) days respectively.
VTE rates at 30 days
The VTE rate following colectomy at 30 days was 98.76 per 1000 person years (95%CI 86.12–113.25).
Patients who underwent MIS had a 64% reduced risk of VTE (aIRR 0.36 95% CI 0.20–0.65) compared to those who underwent open colectomies at 30 days (Table 2).
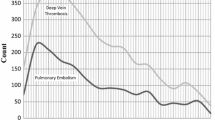
Following elective colectomy, the overall rate of VTE at 30 days was 51.14 per 1000 person-years (95%CI 38.30–68.27) and 135.18 per 1000 person-years (95%CI 115.72–157.91) following emergency colectomy (Table 2). Patients undergoing emergency colectomy had a twofold increased risk (aIRR 2.07, 95%CI 1.47–2.90) of developing VTE 30 days post-surgery when compared to those in the elective group. These differences remained significant after adjusting for age, gender, co-morbidity, and operative technique. The cumulative incidence of VTE at 30 days were 1.11% in the emergency setting and 0.42% (p<0.001) following elective colectomy (see Fig 1).
Cumulative Incidence curve for post colectomy venous thromboembolism rates by time post admission, stratified by admission type. At 30 days, the cumulative incidence was 0.42% and 1.11% for elective and emergency colectomy respectively (p<0.001). At 90 days, the cumulative incidence was 0.69% and 1.82% for elective and emergency colectomy respectively (p<0.001)
VTE rates at 90 days
The overall VTE rate following colectomy at 90 days was 54.72 per 1000 person years (95%CI 48.96–61.15). All VTE rates at 90 days post-op were stratified by admission type as shown below, as there were sufficient VTE events to allow for this.
Emergency colectomy
In our model for the emergency setting, age was the only factor that had a significant effect on VTE rates at 90 days. Table 3 shows that emergency patients ≥70 years old had VTE rates almost 3 times greater (aIRR 2.97, 95% CI 2.05–4.29) than those <70 years old. An almost 50% rise in the crude rate of VTE was seen in female patients (90.7 per 1000 person-years, 95% CI 77.48–106.16) compared to males (59.46 per 1000 person-years, 95% CI 48.01–73.64). The crude rate of VTE was lower post emergency MIS at 90 days (38.1 per 1000 person-years (95% CI 21.11–68.82)) than it was following an open approach (80.5 per 1000 person-years (95% CI 70.68–91.63), translating to a non-significant but almost 50% reduction in VTE risk following MIS colectomy (aIRR 0.57 95%CI 0.31–1.04). Although the crude VTE rates were higher in patients with perforation and/or abscess when compared to those without perforation, this reduced after adjusting for the other factors in the model and was not significant (aIRR 1.27 95%CI 0.95–1.68). Figure 2 shows a cumulative incidence of 0.88% of VTE events following MIS and 1.91% (p=0.015) following open surgery at 90 days post-op. Overall, 1.82% of emergency colectomy patients developed post-op VTE at 90 days.
Cumulative Incidence curve for post-surgery venous thromboembolism rates following emergency colectomy by time post admission, stratified by operative technique: At 30 days, the cumulative incidence was 0.34% and 1.18% (p=0.008) for emergency MIS and open surgery respectively. At 90 days, the cumulative incidence was 0.88% and 1.91% (p=0.015) for emergency MIS and open surgery respectively. MIS, minimally invasive surgery
Elective colectomy
Age, gender, and comorbidity did not have a significant effect on the rate of VTE episodes 90 days post elective colectomy. Table 4 shows a minimally invasive approach resulted in 47% reduction in VTE risk (aIRR 0.53, 95% CI 0.30–0.93) compared to an open approach at 90 days. Additionally, a cumulative incidence of 0.43% and 0.84% (p=0.016) is shown for VTE events 90 days post MIS and open colectomy respectively in Fig. 3. Overall, 0.69% of elective colectomy patients developed post-op VTE at 90 days.
Cumulative Incidence curve for post-surgery venous thromboembolism rates following elective colectomy by time post admission, stratified by operative technique. At 30 days, the cumulative incidence was 0.21% and 0.53% (p=0.013) for elective MIS and open surgery respectively. At 90 days, the cumulative incidence was 0.43% and 0.84% (p=0.016) for elective MIS and open surgery respectively. MIS, minimally invasive surgery
Discussion
Summary
In this cohort of patients undergoing colectomy for diverticular disease, the overall rate of VTE was found to be higher following emergency colectomy. Furthermore, the rates for both emergency and elective admissions continue to rise with time post-surgery. The proportion of emergency colectomy patients that develop VTE following surgery climbs from 1.11 to 1.82% at 30 and 90 days respectively. In those ≥70 years, the VTE rates were 3 times greater (aIRR 2.97, 95% CI 2.05–4.29) than patients <70 years at 90 days post emergency colectomy. This is in comparison to a rise from 0.42 to 0.69% of patients that develop VTE following elective colectomy at 30 and 90 days respectively where age was not a significant factor. Conversely, when looking at operative technique, MIS is associated with lower VTE rates. In the 90 days post elective colectomy, the rate of VTEs was 17.3 per 1000 person-years (95% CI 10.59–28.20) and 34.2 per 1000 person-years (95% CI 26.34–44.48) following MIS and open surgery respectively. Although the results were not significant, a similar reduction is seen when comparing VTE rates post emergency colectomy at 90 days for MIS and open surgery. These findings demonstrate that patients, particularly the elderly, undergoing open emergency colectomy for diverticular disease have a prolonged VTE risk and would therefore potentially benefit from VTE prevention strategies, such as extended VTE prophylaxis.
Strengths and limitations
Being a large population study, this study has the power to allow observed VTE rates to be stratified by admission type, operative technique and known VTE risk factors. Additionally, by using an unselected population-based cohort, its outcomes will also be generalizable to other populations with universally accessible modern healthcare systems. To avoid any surveillance bias [32], a validated definition of VTE was used to capture both inpatient and outpatient VTE events from both primary and secondary care. This ensured the cohort was not comprised of solely hospitalized patients [27].
A limitation of this study was the unavailability of patient level hospital prescribing information on NHS Direct, and therefore it was not possible to assess the effect of VTE prophylaxis regimen directly. However, data from a recent national audit reports risk assessments and therefore appropriateness of VTE prophylaxis for 95–96% of NHS acute admissions were carried out [33, 34]. Consequently, patients in this cohort would have had VTE prophylaxis prescribed in keeping with national trends thereby, not affecting the interpretation of our results. As with any population-based database, there are always concerns surrounding the accuracy of recorded data. However, the databases utilized within this study have been extensively used, previously validated and contain built-in metrics to assure data quality and accuracy, including the use of a validated definition of a VTE outcome [19, 27, 35, 36].
Emergency colectomy
Overall, the rate of VTE is doubled at 30 days following emergency colectomies when compared to those done in an elective setting. Furthermore, patients over 70 years old had a threefold increased risk of VTE at 90 days following emergency colorectal surgery. This coincides with multiple studies that have found emergency surgery to be a risk factor for post-operative VTEs and yield almost double the rates when compared to their elective counterparts [10, 17, 19, 37, 38]. While these studies investigate the occurrence of post-colectomy VTEs, they do not explore those related to diverticular disease in particular or the effect of MIS. Some studies [17] had shorter investigation periods and only included in-patient VTE events. More recently, a large quality improvement project by Poulos et al. explored likely subgroups at increased risk of VTE following diverticular resection [12]. Over an 11-year period, they too found emergency surgery and age > 65 to be significant predictors of VTE events.
Elective colectomy
There are no prior studies specifically addressing the VTE risk following elective surgery in patients with diverticular disease. Operative technique is a significantly associated with VTE events at 90 days following elective colorectal resection [39]. The crude VTE rates following MIS and open surgery were 17.3 and 34.2 per 1000 person years respectively which translates to a halved risk of VTE post MIS. Other studies report a similar reduction in VTE rates following minimally invasive colectomy [40,41,42,43]. Shapiro et al. [40] demonstrated rates of 1.2% and 2.9% following laparoscopic and open approaches however this population included colorectal cancer and IBD and was not specific to diverticular disease. Meanwhile, over a 5 year period Mohadamyeghaneh et al. [42] found open colorectal surgery was associated with a 33% increased risk of deep venous thromboembolism and 73% increased risk of pulmonary embolism when compared to a laparoscopic approach. However, this study focused solely on VTE rates post colectomy for perforated diverticulitis.
Clinical relevance
As the incidence of diverticular disease increases [45, 46] emergent colectomies are becoming more frequent [6, 47]. Emergency colorectal surgery and diverticular disease are known independent risk factors for VTE [9, 48]. Despite this rising prevalence, post-colectomy VTE rates for diverticular disease in particular have not been previously explored. Our cohort of patients with surgically managed disease had significant VTE rates at 30 (98.76 per 1000 person years, 95% CI 86.12–113.25) and 90 (54.72 per 1000 person years 95% CI 48.96–61.15) days following colectomy. Emergent colectomy had a subsequently greater VTE risk at 30 days while those over 70 years old had VTE rates 3 times greater than other age groups at 90 days after colectomy. These clear high-risk groups identified within patients with surgically managed diverticular disease may also be potential targets for future interventional studies in mitigating this increased risk. Minimally invasive alternatives as well as the implementation of ERAS have been shown to reduce the risk of developing post-colectomy VTE and have better surgical outcomes [42,43,44, 49,50,51,52,53,54].
Conclusion
VTE rates are elevated following emergency colorectal surgery for diverticular disease in comparison to elective colectomy. These observed VTE rates were elevated at both 30 and 90 days post-op. As they are at an increased risk for VTE, patients undergoing emergency colectomy for diverticular disease may represent a high risk group for future interventional studies for example on the use of extended VTE prophylaxis.
References
Strate LL, Morris AM (2019) Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology 156(5):1282–98.e1
Morris AM, Regenbogen SE, Hardiman KM, Hendren S (2014) Sigmoid diverticulitis: a systematic review. Jama 311(3):287–297
Weiss AJ, Elixhauser A, Andrews RM (2006) Characteristics of operating room procedures in U.S. Hospitals, 2011. In: Statistical Brief #170. Healthcare cost and utilization project (HCUP) Statistical Briefs. Agency for healthcare research and quality (US), Rockville (MD)
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ et al (2012) Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 143(5):1179–87.e3
Humes DJ, Spiller RC (2014) Review article: The pathogenesis and management of acute colonic diverticulitis. Aliment Pharmacol Ther 39(4):359–370
Etzioni DA, Mack TM, Beart RW Jr, Kaiser AM (2009) Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg 249(2):210–217
Strassle PD, Kinlaw AC, Chaumont N, Angle HL, Lumpkin ST, Koruda MJ et al (2019) Rates of elective colectomy for diverticulitis continued to increase after 2006 Guideline Change. Gastroenterology 157(6):1679–81.e11
McLeod RS, Geerts WH, Sniderman KW, Greenwood C, Gregoire RC, Taylor BM et al (2001) Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian colorectal DVT prophylaxis trial: a randomized, double-blind trial. Ann Surg 233(3):438–444
Strate LL, Erichsen R, Horváth-Puhó E, Pedersen L, Baron JA, Sørensen HT (2014) Diverticular disease is associated with increased risk of subsequent arterial and venous thromboembolic events. Clin Gastroenterol Hepatol 12(10):1695–701.e1. https://doi.org/10.1016/j.cgh.2013.11.026
Lewis-Lloyd CA, Humes DJ, West J, Peacock O, Crooks CJ (2022) The duration and magnitude of postdischarge venous thromboembolism following colectomy. Ann Surg 276(3):e177
Lewis-Lloyd CA, Crooks CJ, West J, Peacock O, Humes DJ (2022) Time trends in the incidence rates of venous thromboembolism following colorectal resection by indication and operative technique. Colorectal Dis 00:1–11
Poulos CM, Althoff AL, Scott RB, Wakefield D, Lewis R (2022) A novel scoring system for identifying patients at risk for venous thromboembolism undergoing diverticular resection: an American College of Surgeons-National Surgical Quality Improvement Program Study. Surg Endosc. https://doi.org/10.1007/s00464-022-09129-6
Fleming F, Gaertner W, Ternent CA, Finlayson E, Herzig D, Paquette IM et al (2018) The American Society of Colon and Rectal Surgeons Clinical Practice Guideline for the Prevention of Venous Thromboembolic Disease in Colorectal Surgery. Dis Colon Rectum 61(1):14–20
Queensland Health. Guideline for the prevention of venous thromboembolism (VTE) in adult hospitalised patients. 2018. https://www.health.qld.gov.au/__data/assets/pdf_file/0031/812938/vte-prevention-guideline.pdf. Accessed 24th March 2022
Peery AF, Crockett SD, Barritt AS, Dellon ES, Eluri S, Gangarosa LM et al (2015) Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology 149(7):1731–41.e3
Beal EW, Tumin D, Chakedis J, Porter E, Moris D, Zhang XF et al (2018) Which patients require extended thromboprophylaxis after colectomy? modeling risk and assessing indications for post-discharge pharmacoprophylaxis. World J Surg 42(7):2242–2251
El-Dhuwaib Y, Selvasekar C, Corless DJ, Deakin M, Slavin JP (2017) Venous thromboembolism following colorectal resection. Colorectal Dis 19(4):385–394
Kaplan GG, Lim A, Seow CH, Moran GW, Ghosh S, Leung Y et al (2015) Colectomy is a risk factor for venous thromboembolism in ulcerative colitis. World J Gastroenterol 21(4):1251–1260
Humes DJ, Walker AJ, Blackwell J, Hunt BJ, West J (2015) Variation in the risk of venous thromboembolism following colectomy. Br J Surg 102(13):1629–1638
Makar M, Bhurwal A, Tawadros A, Reja M, Patel A (2020) Sa1642 The effects of venous thromboembolism in hospitalized patients with acute diverticulitis: a nationwide cohort study. Gastroenterology 158:S-365
Gutta A, Redd MK, Shah R, Jeepalyam S, Yousef O, Clarkston WK (2016) Su1212 Acute diverticulitis is associated with an increased risk of arterial and venous thrombosis in a tertiary hospital-based patient cohort. Gastroenterology 150(4, Supplement 1):S497
Hassan I, Cima RR, Larson DW, Dozois EJ, Byrne MMO, Larson DR et al (2007) The impact of uncomplicated and complicated diverticulitis on laparoscopic surgery conversion rates and patient outcomes. Surg Endosc 21(10):1690–1694
Papageorge CM, Kennedy GD, Carchman EH (2016) National trends in short-term outcomes following non-emergent surgery for diverticular disease. J Gastrointest Surg 20(7):1376–1387
Nelson DW, Simianu VV, Bastawrous AL, Billingham RP, Fichera A, Florence MG, Johnson EK, Johnson MG, Thirlby RC, Flum DR, Steele SR (2015) Thromboembolic Complications and Prophylaxis Patterns in Colorectal Surgery. JAMA surg 150(8):712–720
Weir S, Kuo TC, Samnaliev M, Tierney TS, Manca A, Taylor RS et al (2019) Reoperation following lumbar spinal surgery: costs and outcomes in a UK population cohort study using the Clinical Practice Research Datalink (CPRD) and Hospital Episode Statistics (HES). Eur Spine J 28(4):863–871
Wolf A, Dedman D, Campbell J, Booth H, Lunn D, Chapman J et al (2019) Data resource profile: Clinical Practice Research Datalink (CPRD) aurum. Int J Epidemiol 48(6):1740-g
Lawrenson R, Todd JC, Leydon GM, Williams TJ, Farmer RD (2000) Validation of the diagnosis of venous thromboembolism in general practice database studies. Br J Clin Pharmacol 49(6):591–596
Medicines & Healthcare products Regulatory Agency, National Institute for Health Research. Clinical Practice Research Datalink (CPRD). Department of Health and Social Care. https://cprd.com/home. Published 2021. Accessed 24th March, 2022.
NHS Digital- Hospital Episode Statistics (HES) [Internet]. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics. Edited 5th January 2022. Accessed 24th March 2022.
Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P (2017) Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC). Int J Epidemiol 46(4):1093–109i
Nemeth B, Lijfering WM, Nelissen RGHH et al (2019) Risk and risk factors associated with recurrent venous thromboembolism following surgery in patients with history of venous thromboembolism. JAMA Netw Open 2(5):e193690
Bilimoria KY, Chung J, Ju MH, Haut ER, Bentrem DJ, Ko CY et al (2013) Evaluation of surveillance bias and the validity of the venous thromboembolism quality measure. Jama 310(14):1482–1489
England NHS, Improvement NHS (2020) Quarter 3 2019/20 (October to December 2019). National Health Service (NHS), United Kingdom
Henke PK, Kahn SR, Pannucci CJ et al (2020) Call to action to prevent venous thromboembolism in hospitalized patients: a policy statement from the American Heart Association. Circulation 141(24):e914–e931
Jick SS, Hagberg KW, Persson R, Vasilakis-Scaramozza C, Williams T, Crellin E, Myles P (2020) Quality and completeness of diagnoses recorded in the new CPRD Aurum Database: evaluation of pulmonary embolism. Pharmacoepidemiol Drug Saf 29(9):1134–1140
Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, Smeeth L (2015) Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol 44(3):827–836
Alhassan N, Trepanier M, Sabapathy C, Chaudhury P, Liberman AS, Charlebois P et al (2018) Risk factors for post-discharge venous thromboembolism in patients undergoing colorectal resection: a NSQIP analysis. Tech Coloproctol 22(12):955–964
McKenna NP, Behm KT, Ubl DS, Glasgow AE, Mathis KL, Pemberton JH et al (2017) Analysis of postoperative venous thromboembolism in patients with chronic ulcerative colitis: is it the disease or the operation? Dis Colon Rectum 60(7):714–722
Buchberg B, Masoomi H, Lusby K, Choi J, Barleben A, Magno C et al (2011) Incidence and risk factors of venous thromboembolism in colorectal surgery: does laparoscopy impart an advantage? Arch Surg 146(6):739–743
Shapiro R, Vogel JD, Kiran RP (2011) Risk of postoperative venous thromboembolism after laparoscopic and open colorectal surgery: an additional benefit of the minimally invasive approach? Dis Colon Rectum 54(12):1496–1502
Cui G, Wang X, Yao W, Li H (2013) Incidence of postoperative venous thromboembolism after laparoscopic versus open colorectal cancer surgery: a meta-analysis. Surg Laparosc Endosc Percutan Tech 23(2):128–134
Moghadamyeghaneh Z, Talus H, Fitzgerald S, Muthusamy M, Stamos MJ, Roudnitsky V (2021) Outcomes of minimally invasive colectomy for perforated diverticulitis. Am Surg 87(4):561–567
Masoomi H, Buchberg B, Nguyen B, Tung V, Stamos MJ, Mills S (2011) Outcomes of laparoscopic versus open colectomy in elective surgery for diverticulitis. World J Surg 35(9):2143–2148. https://doi.org/10.1007/s00268-011-1117-4
Hajirawala LN, Moreci R, Leonardi C, Bevier-Rawls ER, Orangio GR, Davis KG et al (2021) Laparoscopic colectomy for acute diverticulitis in the urgent setting is associated with similar outcomes to open. Am Surg 88(5):901–907
Lee TH, Setty PT, Parthasarathy G, Bailey KR, Wood-Wentz CM, Fletcher JG et al (2018) Aging, obesity, and the incidence of diverticulitis: a population-based study. Mayo Clin Proc 93(9):1256–1265
Carr S, Velasco AL. Colon Diverticulitis. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC; 2022.
Masoomi H, Buchberg BS, Magno C, Mills SD, Stamos MJ (2011) Trends in diverticulitis management in the United States from 2002 to 2007. Arch Surg 146(4):400–406
Thomsen L, Troelsen FS, Nagy D, Skajaa N, Körmendiné Farkas D, Erichsen R (2021) Venous thromboembolism and risk of cancer in patients with diverticular disease: a Danish population-based cohort study. Clin Epidemiol 13:735–744
Mohn AC, Egge J, Rokke O (2011) Low risk of thromboembolic complications after fast-track abdominal surgery with thrombosis-prophylaxis only during hospital stay. Gastroenterology Res 4(3):107–113. https://doi.org/10.4021/gr320e
Shang Y, Guo C, Zhang D (2018) Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer: a propensity score matching analysis. Medicine (Baltimore). 97(39):e12348. https://doi.org/10.1097/MD.0000000000012348
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD, Urman RD, Chang GJ, Fichera A, Kessler H, Grass F, Whang EE, Fawcett WJ, Carli F et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced Recovery After Surgery (ERAS®) Society Recommendations: 2018. World J Surg 43(3):659–695. https://doi.org/10.1007/s00268-018-4844-y
Ni X, Jia D, Chen Y, Wang L, Suo J (2019) Is the Enhanced Recovery After Surgery (ERAS) Program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg 23(7):1502–1512. https://doi.org/10.1007/s11605-019-04170-8
Agdgomelashvili I, Mosidze B, Merabishvili G, Demetrashvili Z (2021) Enhanced recovery after surgery vs traditional care in elective colorectal surgery: a retrospective cohort study. Georgian Med News 311:17–21
Vendler MMI, Haidari TA, Waage JE, Kleif J, Kristensen B, Gögenur I, Bertelsen CA (2017) Copenhagen cOmplete Mesocolic Excision Study group (COMES). Incidence of venous thromboembolic events in enhanced recovery after surgery for colon cancer: a retrospective, population-based cohort study. Colorectal Dis 19(11):O393–O401. https://doi.org/10.1111/codi.13910
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Anjali K D S Yapa and Christopher Lewis-Lloyd. The first draft of the manuscript was written by Anjali K D S Yapa, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. All authors have read and complied with the author guidelines.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure
This work is original, and no authors have published, posted, or submitted any related papers from the same study. No funding was available for this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yapa, A.K.D.S., Humes, D.J., Crooks, C.J. et al. Venous thromboembolism following colectomy for diverticular disease: an English population-based cohort study. Langenbecks Arch Surg 408, 203 (2023). https://doi.org/10.1007/s00423-023-02920-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02920-6