Abstract
Background
Enhanced recovery after surgery (ERAS) program has shown a few advantages in colorectal cancer surgery. However, the effectiveness of the ERAS program in laparoscopic colorectal cancer surgery is still unclear. We performed a meta-analysis of randomized controlled trials (RCTs) to evaluate the effect of ERAS program in laparoscopic colorectal cancer surgery compared with traditional perioperative care (TC).
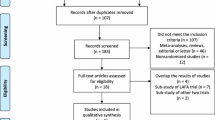
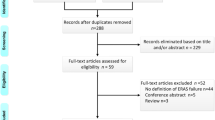
Methods
PubMed, EMBASE, Web of Science, The Cochrane Library, and ClinicalTrials.gov were searched for eligible RCTs comparing ERAS program with TC in laparoscopic colorectal cancer surgery. The main outcomes included the average length of postoperative hospital stay (PHS), time to first flatus and defecation, overall complication, readmission, and mortality rates were undertaken.
Results
Thirteen RCTs involving 1298 patients were included in our study (639 in ERAS group and 659 in TC group). ERAS group had shorter average length of PHS (weighted mean difference [WMD] − 2.00 day, 95% confidence interval [CI] − 2.52 to − 1.48, p = 0.00), time to first flatus (WMD − 12.18 h, 95%CI − 16.69 to − 7.67, p = 0.00), and time to first defecation (WMD − 32.93 h, 95%CI − 45.36 to − 20.50, p = 0.00) than TC group. In addition, the overall complication rates (risk ratio [RR] 0.59, 95%CI 0.40 to 0.86, p < 0.01) were significantly lower in ERAS group compared with TC group.
Conclusions
The results indicated that ERAS program is a much better effective and safe protocol for laparoscopic colorectal cancer surgery compared with TC. Hence, ERAS program should be recommended in laparoscopic colorectal cancer surgery.






Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68: 7–30.
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 2016; 66: 271–289.
Allaix ME, Furnee EJ, Mistrangelo M, Arezzo A, Morino M. Conversion of laparoscopic colorectal resection for cancer: What is the impact on short-term outcomes and survival? World J Gastroenterol 2016; 22: 8304–8313.
Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surgical laparoscopy & endoscopy 1991; 1: 144–150.
Noel JK, Fahrbach K, Estok R, Cella C, Frame D, Linz H, Cima RR, Dozois EJ, Senagore AJ. Minimally invasive colorectal resection outcomes: short-term comparison with open procedures. J Am Coll Surg 2007; 204: 291–307.
Junghans T, Raue W, Haase O, Neudecker J, Schwenk W. Value of laparoscopic surgery in elective colorectal surgery with “fast-track”-rehabilitation. Zentralblatt fur chirurgie 2006; 131: 298–303.
Kaltoft B, Gogenur I, Rosenberg J. Reduced length of stay and convalescence in laparoscopic vs open sigmoid resection with traditional care: a double blinded randomized clinical trial. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 2011; 13: e123–130.
Coratti F, Coratti A, Malatesti R, Testi W, Tani F. Laparoscopic versus open resection for colorectal cancer: meta-analysis of the chief trials. Il Giornale di chirurgia 2009; 30: 377–384.
Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet 1995; 345: 763–764.
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clinical nutrition (Edinburgh, Scotland) 2005; 24: 466–477.
Kehlet H. Fast-track colorectal surgery. Lancet 2008; 371: 791–793.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997; 78: 606–617.
Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C, von Meyenfeldt MF, Fearon KC, Revhaug A, Norderval S, Ljungqvist O, Lobo DN, Dejong CH. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Archives of surgery (Chicago, Ill : 1960) 2009; 144: 961–969.
Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ (Clinical research ed) 2001; 322: 473–476.
Kehlet H. Fast-track colonic surgery: status and perspectives. Recent results in cancer research Fortschritte der Krebsforschung Progres dans les recherches sur le cancer 2005; 165: 8–13.
Feng F, Li XH, Shi H, Wu GS, Zhang HW, Liu XN, Zhao QC. Fast-track surgery combined with laparoscopy could improve postoperative recovery of low-risk rectal cancer patients: a randomized controlled clinical trial. Journal of digestive diseases 2014; 15: 306–313.
Taupyk Y, Cao X, Zhao Y, Wang C, Wang Q. Fast-track laparoscopic surgery: a better option for treating colorectal cancer than conventional laparoscopic surgery. Oncology Letters 2015; 10: 443–448.
Lee SM, Kang SB, Jang JH, Park JS, Hong S, Lee TG, Ahn S. Early rehabilitation versus conventional care after laparoscopic rectal surgery: a prospective, randomized, controlled trial. Surgical Endoscopy 2013; 27: 3902–3909.
Zhao JH, Sun JX, Gao P, Chen XW, Song YX, Huang XZ, Xu HM, Wang ZN. Fast-track surgery versus traditional perioperative care in laparoscopic colorectal cancer surgery: a meta-analysis. BMC Cancer 2014; 14: 607.
Song MX, Li XR. Efficacy of fast track surgery in elderly patients with colorectal cancer undergoing laparoscopic treatment: A meta-analysis. World Chinese Journal of Digestology 2015; 23: 3960–3966.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62: e1–34.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2011; 343: d5928.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD, Urman RD, Chang GJ, Fichera A, Kessler H, Grass F, Whang EE, Fawcett WJ, Carli F, Lobo DN, Rollins KE, Balfour A, Baldini G, Riedel B, Ljungqvist O. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS((R))) Society Recommendations: 2018. World J Surg 2018.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5: 13.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 2018; 27: 1785–1805.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials 2015; 45: 139–145.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ (Clinical research ed) 1998; 316: 469; author reply 470-461.
Lee T-G, Kang S-B, Kim D-W, Hong S, Heo SC, Park KJ. Comparison of Early Mobilization and Diet Rehabilitation Program With Conventional Care After Laparoscopic Colon Surgery: A Prospective Randomized Controlled Trial. Diseases of the Colon & Rectum 2011; 54: 21–28.
van Bree SH, Vlug MS, Bemelman WA, Hollmann MW, Ubbink DT, Zwinderman AH, de Jonge WJ, Snoek SA, Bolhuis K, van der Zanden E, The FO, Bennink RJ, Boeckxstaens GE. Faster recovery of gastrointestinal transit after laparoscopy and fast-track care in patients undergoing colonic surgery. Gastroenterology 2011; 141: 872–880.e871–874.
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, Sprangers MA, Cuesta MA, Bemelman WA. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 2011; 254: 868–875.
Wang G, Jiang Z-W, Xu J, Gong J-F, Bao Y, Xie L-F, Li J-S. Fast-track rehabilitation program vs conventional care after colorectal resection: A randomized clinical trial. World Journal of Gastroenterology 2011; 17: 671–676.
Veenhof AAFA, Vlug MS, Van Der Pas MHGM, Sietses C, Van Der Peet DL, De Lange-De Klerk ESM, Bonjer HJ, Bemelman WA, Cuesta MA. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: A randomized trial. Annals of Surgery 2012; 255: 216–221.
Wang G, Jiang Z, Zhao K, Li G, Liu F, Pan H, Li J. Immunologic response after laparoscopic colon cancer operation within an enhanced recovery program. Journal of gastrointestinal surgery 2012; 16: 1379–1388.
Wang Q, Suo J, Jiang J, Wang C, Zhao YQ, Cao X. Effectiveness of fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for elderly patients: a randomized trial. Colorectal disease 2012; 14: 1009–1013.
Mari GM, Costanzi A, Maggioni D, Origi M, Ferrari GC, De Martini P, De Carli S, Pugliese R. Fast-track versus standard care in laparoscopic high anterior resection: a prospective randomized-controlled trial. Surgical laparoscopy, endoscopy & percutaneous techniques 2014; 24: 118–121.
Mari G, Crippa J, Costanzi A, Mazzola M, Rossi M, Maggioni D. ERAS Protocol Reduces IL-6 Secretion in Colorectal Laparoscopic Surgery: results From a Randomized Clinical Trial. Surgical laparoscopy, endoscopy & percutaneous techniques 2016; 26: 444–448.
Shetiwy M, Fady T, Shahatto F, Setit A. Standardizing the protocols for enhanced recovery from colorectal cancer surgery: are we a step closer to ideal recovery? Annals of coloproctology 2017; 33: 86–92.
Blazeby JM. Systematic review of outcomes used to evaluate enhanced recovery after surgery (Br J Surg 2014; 101: 159-170). Br J Surg 2014; 101: 171.
Carli F. Physiologic considerations of Enhanced Recovery After Surgery (ERAS) programs: implications of the stress response. Canadian journal of anaesthesia = Journal canadien d'anesthesie 2015; 62: 110–119.
Stowers MD, Lemanu DP, Hill AG. Health economics in Enhanced Recovery After Surgery programs. Canadian journal of anaesthesia = Journal canadien d'anesthesie 2015; 62: 219–230.
Li P, Fang F, Cai JX, Tang D, Li QG, Wang DR. Fast-track rehabilitation VS conventional care in laparoscopic colorectal resection for colorectal malignancy: A meta-analysis. World Journal of Gastroenterology 2013; 19: 9119–9126.
Tan SJ, Zhou F, Yui WK, Chen QY, Lin ZL, Hu RY, Gao T, Li N. Fast track programmes vs. traditional care in laparoscopic colorectal surgery: a meta-analysis of randomized controlled trials. Hepato-gastroenterology 2014; 61: 79–84.
Author information
Authors and Affiliations
Contributions
XFN and JS: designed the study. XFN and DJ: searched the databases and collected full-text papers. LW and YC: performed statistical analysis. XFN and JS: wrote the manuscript. All authors read the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
The article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ni, X., Jia, D., Chen, Y. et al. Is the Enhanced Recovery After Surgery (ERAS) Program Effective and Safe in Laparoscopic Colorectal Cancer Surgery? A Meta-Analysis of Randomized Controlled Trials. J Gastrointest Surg 23, 1502–1512 (2019). https://doi.org/10.1007/s11605-019-04170-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04170-8