Abstract
Purpose
This study evaluated the short-term outcomes and prognosis after laparoscopic total gastrectomy (LTG) in elderly patients aged ≥ 80 years in a multicenter retrospective cohort study using propensity score matching.
Methods
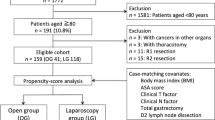
We retrospectively enrolled 440 patients who underwent curative LTG for gastric cancer at six institutions between January 2004 and December 2018. Patients were categorized into an elderly patient group (EG; age ≥ 80 years) and non-elderly patient group (non-EG; age < 80 years). Patients were matched using the following propensity score covariates: sex, body mass index, American Society of Anesthesiologists physical status, extent of lymph node dissection, and Japanese Classification of Gastric Carcinoma stage. Short-term outcomes and prognoses were compared.
Results
We identified 37 propensity score-matched pairs. The median operative time was significantly shorter, and postoperative stay was longer in the EG. In terms of postoperative outcomes, the rates of all complications were comparable. The median follow-up period of the EG and non-EG was 11.5 (1–106.4) months and 35.7 (1–110.0) months, respectively; there were significant differences in 5-year overall survival between the two groups (EG, 58.5% vs. non-EG, 91.5%; P = 0.031). However, there were no significant differences in 5-year disease-specific survival (EG, 62.1% vs. non-EG, 91.5%; P = 0.068) or 5-year disease-free survival (EG, 52.9% vs. non-EG, 60.8%; P = 0.132).
Conclusions
LTG seems to be safe and feasible in elderly patients. LTG had a limited effect on morbidity, disease recurrence, and survival in elderly patients. Therefore, age should not prevent elderly patients from benefitting from LTG.


Similar content being viewed by others
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Asaka M, Sugiyama T, Nobuta A, Kato M, Takeda H, Graham DY (2001) Atrophic gastritis and intestinal metaplasia in Japan: results of a large multicenter study. Helicobacter 6:294–299. https://doi.org/10.1046/j.1523-5378.2001.00042.x
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Aiolfi A, Lombardo F, Matsushima K, Sozzi A, Cavalli M, Panizzo V, Bonitta G, Bona D (2021) Systematic review and updated network meta-analysis of randomized controlled trials comparing open, laparoscopic-assisted, and robotic distal gastrectomy for early and locally advanced gastric cancer. Surgery. Sep;170(3):942–951. https://doi.org/10.1016/j.surg.2021.04.014.
Ebihara Y, Okushiba S, Kawarada Y, Kitashiro S, Katoh H (2013) Outcome of functional end-to-end esophagojejunostomy in totally laparoscopic total gastrectomy. Langenbecks Arch Surg 398:475–479. https://doi.org/10.1007/s00423-013-1051-z
van der Wielen N, Straatman J, Daams F, Rosati R, Parise P, Weitz J, Reissfelder C, Diez Del Val I, Loureiro C, Parada-González P, Pintos-Martínez E, Mateo Vallejo F, Medina Achirica C, Sánchez-Pernaute A, Ruano Campos A, Bonavina L, Asti ELG, Alonso Poza A, Gilsanz C, Nilsson M, Lindblad M, Gisbertz SS, van Berge Henegouwen MI, Fumagalli Romario U, De Pascale S, Akhtar K, Jaap Bonjer H, Cuesta MA, van der Peet DL (2020) Open versus minimally invasive total gastrectomy after neoadjuvant chemotherapy: results of a European randomized trial. Gastric Cancer 24:258–271. https://doi.org/10.1007/s10120-020-01109-w
Lee SR, Kim HO, Son BH, Shin JH, Yoo CH (2014) Laparoscopic-assisted total gastrectomy versus open total gastrectomy for upper and middle gastric cancer in short-term and long-term outcomes. Surg Laparosc Endosc Percutan Tech 24:277–282. https://doi.org/10.1097/SLE.0b013e3182901290
Tsunoda S, Okabe H, Obama K, Tanaka E, Hisamori S, Kinjo Y, Sakai Y (2014) Short-term outcomes of totally laparoscopic total gastrectomy: experience with the first consecutive 112 cases. World J Surg 38:2662–2667. https://doi.org/10.1007/s00268-014-2611-2
Yoshida M, Koga S, Ishimaru K, Yamamoto Y, Matsuno Y, Akita S, Kuwabara J, Tanigawa K, Watanabe Y (2017) Laparoscopy-assisted distal gastrectomy is feasible also for elderly patients aged 80 years and over: effectiveness and long-term prognosis. Surg Endosc 31:4431–4437. https://doi.org/10.1007/s00464-017-5493-1
Tanaka R, Lee SW, Imai Y, Honda K, Matsuo K, Tashiro K, Kawai M, Uchiyama K (2021 May 21) Advantages of laparoscopic surgery for gastric cancer in elderly patients aged over 80 years: a propensity score matching analysis. World J Surg. https://doi.org/10.1007/s00268-021-06157-6
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver 3). Gastric Cancer 14:113–123. https://doi.org/10.1007/s10120-011-0042-4
Japanese Society for Endoscopic Surgery (2014) Guidelines for the management of endoscopic surgery. Japanese Society for Endoscopic Surgery, Tokyo
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161. https://doi.org/10.1002/pst.433
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR, Winchester DP (2017) The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging, 8th ed.. CA: Cancer J Clin 67:93–99. https://doi.org/10.3322/caac.21388
Endo S, Dousei T, Yoshikawa Y, Hatanaka N, Kamiike W, Nishijima J (2013) Prognosis of gastric carcinoma patients aged 85 years or older who underwent surgery or who received best supportive care only. Int J Clin Oncol 18:1014–1019. https://doi.org/10.1007/s10147-012-0482-9
Kim EJ, Seo KW, Yoon KY (2012) Laparoscopy-assisted distal gastrectomy for early gastric cancer in the elderly. J Gastric Cancer 12:232–236. https://doi.org/10.5230/jgc.2012.12.4.232
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107:931–936. https://doi.org/10.1038/bjc.2012.350
Shen Y, Hao Q, Zhou J, Dong B (2017) The impact of frailty and sarcopenia on postoperative outcomes in older patients undergoing gastrectomy surgery: a systematic review and meta-analysis. BMC Geriatr 17:188. https://doi.org/10.1186/s12877-017-0569-2
Tanaka T, Suda K, Inaba K, Umeki Y, Gotoh A, Ishida Y, Uyama I (2019) Impact of frailty on postoperative outcomes for laparoscopic gastrectomy in patients older than 80 years. Ann Surg Oncol 26:4016–4026. https://doi.org/10.1245/s10434-019-07640-0
Murthy BL, Thomson CS, Dodwell D, Shenoy H, Mikeljevic JS, Forman D, Horgan K (2007) Postoperative wound complications and systemic recurrence in breast cancer. Br J Cancer 97:1211–1217. https://doi.org/10.1038/sj.bjc.6604004
Kressner U, Graf W, Mahteme H, Påhlman L, Glimelius B (2002) Septic complications and prognosis after surgery for rectal cancer. Dis Colon Rectum 45:316–321. https://doi.org/10.1007/s10350-004-6174-4
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH (2015) Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg 261:497–505. https://doi.org/10.1097/SLA.0000000000000854
Cho JY, Han HS, Yoon YS, Hwang DW, Jung K, Kim YK (2013) Postoperative complications influence prognosis and recurrence patterns in periampullary cancer. World J Surg 37:2234–2241. https://doi.org/10.1007/s00268-013-2106-6
Jiang N, Deng JY, Ding XW, Zhang L, Liu HG, Liang YX, Liang H (2014) Effect of complication grade on survival following curative gastrectomy for carcinoma. World J Gastroenterol 20:8244–8252. https://doi.org/10.3748/wjg.v20.i25.8244
Li QG, Li P, Tang D, Chen J, Wang DR (2013) Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol 19:4060–4065. https://doi.org/10.3748/wjg.v19.i25.4060
Kawase H, Ebihara Y, Shichinohe T, Nakamura F, Murakawa K, Morita T, Okushiba S, Hirano S (2017) Long-term outcome after laparoscopic gastrectomy: a multicenter retrospective study. Langenbecks Arch Surg 402:41–47. https://doi.org/10.1007/s00423-017-1559-8
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, Nashimoto A, Fujii M, Nakajima T, Ohashi Y (2011) Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol 29:4387–4393. https://doi.org/10.1200/JCO.2011.36.5908
Noh SH, Park SR, Yang HK, Chung HC, Chung IJ, Kim SW, Kim HH, Choi JH, Kim HK, Yu W, Lee JI, Shin DB, Ji J, Chen JS, Lim Y, Ha S, Bang YJ, CLASSIC trial investigators, (2014) Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (Classic): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol 15:1389–1396. https://doi.org/10.1016/S1470-2045(14)70473-5
Yoshida K, Kodera Y, Kochi M, Ichikawa W, Kakeji Y, Sano T, Nagao N, Takahashi M, Takagane A, Watanabe T, Kaji M, Okitsu H, Nomura T, Matsui T, Yoshikawa T, Matsuyama J, Yamada M, Ito S, Takeuchi M, Fujii M (2019) Addition of docetaxel to Oral fluoropyrimidine improves efficacy in patients with stage III gastric cancer: interim analysis of JACCRO GC-07, a randomized controlled trial. J Clin Oncol 37:1296–1304. https://doi.org/10.1200/JCO.18.01138
Rausei S, Boni L, Rovera F, Dionigi G (2013) Locally advanced gastric cancer: a new definition to standardise. J Clin Pathol 66(2):164–165. https://doi.org/10.1136/jclinpath-2012-201176
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D (2016) ESMO Guidelines Committee. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 27(suppl 5):v38-v49. https://doi.org/10.1093/annonc/mdw350
Acknowledgements
The author is grateful to our colleagues (Dr. Hiroshi Kawase, Noriaki Kyogoku, and Mamoru Miyasaka) and the interdisciplinary surgical team. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
Study conception and design: Yuma Ebihara and Yo Kurashima.
Acquisition of data: Yuma Ebihara.
Analysis and interpretation of data: Yuma Ebihara and Yo Kurashima.
Drafting of manuscript: Yuma Ebihara.
Critical revision of the manuscript: Yuma Ebihara, Yo Kurashima, Yusuke Watanabe, Kimitaka Tanaka, Aya Matsui, Yoshitsugu Nakanishi, Toshimichi Asano, Takehiro Noji, Toru Nakamura, Soichi Murakami, Takahiro Tsuchikawa, Keisuke Okamura, Yoshihiro Murakami, Katsuhiko Murakawa, Fumitaka Nakamura, Takayuki Morita, Shunichi Okushiba, Toshiaki Shichinohe, and Satoshi Hirano.
Corresponding author
Ethics declarations
Ethics approval
Hokkaido University Hospital Institutional Review Board approved the data collection and analysis (No. 016–0151).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ebihara, Y., Kurashima, Y., Watanabe, Y. et al. Outcomes of laparoscopic total gastrectomy in elderly patients: a propensity score matching analysis. Langenbecks Arch Surg 407, 1461–1469 (2022). https://doi.org/10.1007/s00423-022-02447-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02447-2