Abstract
Purpose
The use of a mesh with good biocompatibility properties is of decisive importance for the avoidance of recurrences and chronic pain in endoscopic hernia repair surgery. As we know from numerous experiments and clinical experience, large-pore, lightweight polypropylene meshes possess the best biocompatibility. However, large-pore meshes of different polymers may be used as well and might be an alternative solution.
Methods
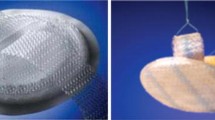
Utilizing a totally extraperitoneal technique in an established animal model, 20 domestic pigs were implanted with either a lightweight large-pore polypropylene (PP) mesh (Optilene® LP) or a medium-weight large-pore knitted polytetrafluorethylene (PTFE) mesh (GORE® INFINIT® mesh). After 94 days, the pigs were sacrificed and postmortem diagnostic laparoscopy was performed, followed by explantation of the specimens for macroscopic, histological and immunohistochemical evaluation.
Results
The mean mesh shrinkage rate was 14.2% for Optilene® LP vs. 24.7% for INFINIT® mesh (p = 0.017). The partial volume of the inflammatory cells was 11.2% for Optilene® LP vs. 13.9% for INFINIT (n.s.). CD68 was significantly higher for INFINIT (11.8% vs. 5.6%, p = 0.007). The markers of cell turnover, namely Ki67 and the apoptotic index, were comparable at 6.4% vs. 12.4% (n.s.) and 1.6% vs. 2.0% (n.s.). In the extracellular matrix, TGF-β was 35.4% for Optilene® LP and 31.0% for INFINIT® (n.s.). Collagen I (pos/300 μm) deposits were 117.8 and 114.9, respectively.
Conclusion
In our experimental examinations, Optilene® LP and INFINIT® showed a comparable biocompatibility in terms of chronic inflammatory reaction; however, the shrinkage rate was significantly higher for INFINIT® after 3 months. The higher shrinkage rate of INFINIT® should be taken into account when choosing the mesh size for an adequate hernia overlap.



Similar content being viewed by others
References
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev (4): CD002197.
van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J (2007) Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 94(4):506–10
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1): CD001785.
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12(1):63–9
Greca FH, de Paula JB, Biondo-Simoes ML, da Costa FD, da Silva AP, Time S, Mansur A (2001) The influence of differing pore sizes on the biocompatibility of two polypropylene meshes in the repair of abdominal defects. Experimental study in dogs. Hernia 5(2):59–64
Junge K, Rosch R, Bialasinski L, Klinge U, Klosterhalfen B, Schumpelick V (2003) Persistent extracellular matrix remodelling at the interface to polymers used for hernia repair. Eur Surg Res 35(6):497–504
Klosterhalfen B, Klinge U, Schumpelick V (1998) Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials 19(24):2235–46
Schug-Pass C, Tamme C, Sommerer F, Tannapfel A, Lippert H, Kockerling F (2008) A lightweight, partially absorbable mesh (Ultrapro) for endoscopic hernia repair: experimental biocompatibility results obtained with a porcine model. Surg Endosc 22(4):1100–6
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V (2002) Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 103(2):208–14
Schumpelick V, Klinge U, Welty G, Klosterhalfen B (1999) Meshes within the abdominal wall. Chirurg 70(8):876–87
Klinge U, Conze J, Klosterhalfen B, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1996) Changes in abdominal wall mechanics after mesh implantation. Experimental changes in mesh stability. Langenbecks Arch Chir 381(6):323–32
Scheidbach H, Tamme C, Tannapfel A, Lippert H, Kockerling F (2004) In vivo studies comparing the biocompatibility of various polypropylene meshes and their handling properties during endoscopic total extraperitoneal (TEP) patchplasty: an experimental study in pigs. Surg Endosc 18(2):211–20
Schopf S, von Ahnen T, von Ahnen M, Schardey H (2010) Chronic pain after laparoscopic transabdominal preperitoneal hernia repair: a randomized comparison of light and extralight titanized polypropylene mesh. World J Surg.
Agarwal BB, Agarwal S, Mahajan KC (2009) Laparoscopic ventral hernia repair: innovative anatomical closure, mesh insertion without 10-mm transmyofascial port, and atraumatic mesh fixation: a preliminary experience of a new technique. Surg Endosc 23(4):900–5
Bringman S, Wollert S, Osterberg J, Heikkinen T (2005) Early results of a randomized multicenter trial comparing Prolene and VyproII mesh in bilateral endoscopic extraperitoneal hernioplasty (TEP). Surg Endosc 19(4):536–40
Heikkinen T, Wollert S, Osterberg J, Smedberg S, Bringman S (2006) Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10(1):34–40
Horstmann R, Hellwig M, Classen C, Rottgermann S, Palmes D (2006) Impact of polypropylene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg 30(9):1742–9
Langenbach MR, Schmidt J, Zirngibl H (2006) Comparison of biomaterials: three meshes and TAPP for inguinal hernia. Surg Endosc 20(10):1511–7
Langenbach MR, Schmidt J, Ubrig B, Zirngibl H (2008) Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc 22(8):1790–7
Agarwal BB, Agarwal KA, Sahu T, Mahajan KC (2010) Traditional polypropylene and lightweight meshes in totally extraperitoneal inguinal herniorrhaphy. Int J Surg 8(1):44–7
Koch A, Bringman S, Myrelid P, Smeds S, Kald A (2008) Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg 95(10):1226–31
Akolekar D, Kumar S, Khan LR, de Beaux AC, Nixon SJ (2008) Comparison of recurrence with lightweight composite polypropylene mesh and heavyweight mesh in laparoscopic totally extraperitoneal inguinal hernia repair: an audit of 1,232 repairs. Hernia 12(1):39–43
Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Heikkinen TJ (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 93(9):1056–9
Champault G, Bernard C, Rizk N, Polliand C (2007) Inguinal hernia repair: the choice of prosthesis outweighs that of technique. Hernia 11(2):125–8
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194(3):394–400
Tamme C, Garde N, Klingler A, Hampe C, Wunder R, Kockerling F (2005) Totally extraperitoneal inguinal hernioplasty with titanium-coated lightweight polypropylene mesh: early results. Surg Endosc 19(8):1125–9
Weyhe D, Belyaev O, Muller C, Meurer K, Bauer KH, Papapostolou G, Uhl W (2007) Improving outcomes in hernia repair by the use of light meshes—a comparison of different implant constructions based on a critical appraisal of the literature. World J Surg 31(1):234–44
Pascual G, Rodriguez M, Gomez-Gil V, Garcia-Honduvilla N, Bujan J, Bellon JM (2008) Early tissue incorporation and collagen deposition in lightweight polypropylene meshes: bioassay in an experimental model of ventral hernia. Surgery 144(3):427–35
Weyhe D, Schmitz I, Belyaev O, Grabs R, Muller KM, Uhl W, Zumtobel V (2006) Experimental comparison of monofile light and heavy polypropylene meshes: less weight does not mean less biological response. World J Surg 30(8):1586–91
Jonas J (2009) The problem of mesh shrinkage in laparoscopic incisional hernia repair. Zentralbl Chir 134(3):209–13
Deeken CR, Abdo MS, Frisella MM, Matthews BD (2011) Physicomechanical evaluation of polypropylene, polyester, and polytetrafluoroethylene meshes for inguinal hernia repair. J Am Coll Surg 212(1):68–79. doi:10.1016/j.jamcollsurg.2010.09.012
Schug-Pass C, Tamme C, Tannapfel A, Kockerling F (2006) A lightweight polypropylene mesh (TiMesh) for laparoscopic intraperitoneal repair of abdominal wall hernias: comparison of biocompatibility with the DualMesh in an experimental study using the porcine model. Surg Endosc 20(3):402–9
Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, Mittal T (2010) Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 24(12):3073–9
Chui LB, Ng WT, Sze YS, Yuen KS, Wong YT, Kong CK (2010) Prospective, randomized, controlled trial comparing lightweight versus heavyweight mesh in chronic pain incidence after TEP repair of bilateral inguinal hernia. Surg Endosc 24(11):2735–8
Khan LR, Liong S, de Beaux AC, Kumar S, Nixon SJ (2010) Lightweight mesh improves functional outcome in laparoscopic totally extra-peritoneal inguinal hernia repair. Hernia 14(1):39–45
Agarwal BB, Agarwal KA, Mahajan KC (2009) Prospective double-blind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. Surg Endosc 23(2):242–7
Melman L, Jenkins ED, Hamilton NA, Bender LC, Brodt MD, Deeken CR, Greco SC, Frisella MM, Matthews BD (2011) Histologic and biomechanical evaluation of a novel macroporous polytetrafluoroethylene knit mesh compared to lightweight and heavyweight polypropylene mesh in a porcine model of ventral incisional hernia repair. Hernia: the journal of hernias and abdominal wall surgery. doi:10.1007/s10029-011-0787-z
Junge K, Rosch R, Krones CJ, Klinge U, Mertens PR, Lynen P, Schumpelick V, Klosterhalfen B (2005) Influence of polyglecaprone 25 (Monocryl) supplementation on the biocompatibility of a polypropylene mesh for hernia repair. Hernia 9(3):212–7
Weyhe D, Belyaev O, Buettner G, Mros K, Mueller C, Meurer K, Papapostolou G, Uhl W (2008) In vitro comparison of three different mesh constructions. ANZ J Surg 78(1–2):55–60
Schug-Pass C, Sommerer F, Tannapfel A, Lippert H, Kockerling F (2009) The use of composite meshes in laparoscopic repair of abdominal wall hernias: are there differences in biocompatibily?: experimental results obtained in a laparoscopic porcine model. Surg Endosc 23(3):487–95
Langer C, Schwartz P, Krause P, Mohammadi H, Kulle B, Schaper A, Fuzesi L, Becker H (2005) In-vitro study of the cellular response of human fibroblasts cultured on alloplastic hernia meshes. Influence of mesh material and structure. Chirurg 76(9):876–85
Weyhe D, Hoffmann P, Belyaev O, Mros K, Muller C, Uhl W, Schmitz F (2007) The role of TGF-beta1 as a determinant of foreign body reaction to alloplastic materials in rat fibroblast cultures: comparison of different commercially available polypropylene meshes for hernia repair. Regul Pept 138(1):10–4
Conze J, Krones CJ, Schumpelick V, Klinge U (2007) Incisional hernia: challenge of re-operations after mesh repair. Langenbecks Arch Surg 392(4):453–7
Schoenmaeckers EJ, van der Valk SB, van den Hout HW, Raymakers JF, Rakic S (2009) Computed tomographic measurements of mesh shrinkage after laparoscopic ventral incisional hernia repair with an expanded polytetrafluoroethylene mesh. Surg Endosc 23(7):1620–3
Saberski ER, Orenstein SB, Novitsky YW (2011) Anisotropic evaluation of synthetic surgical meshes. Hernia 15(1):47–52
Acknowledgement
This study was supported by a research grant from W.L. Gore & Associates, Inc. (Flagstaff, AZ, USA) and BBD Aesculap GmbH (Tuttlingen, Germany).
Authors' contributions
D.J. was responsible for analysis and interpretation of data and drafting of manuscript. C.S-P. was responsible for study conception and design, acquisition of data, analysis and interpretation of data, and drafting of manuscript. F.S. and A. T. were responsible for acquisition, analysis and interpretation of data. H.L was responsible for study conception and critical revision of manuscript. F.K. was responsible for study conception and design, acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacob, D.A., Schug-Paß, C., Sommerer, F. et al. Comparison of a lightweight polypropylene mesh (Optilene® LP) and a large-pore knitted PTFE mesh (GORE® INFINIT® mesh)—Biocompatibility in a standardized endoscopic extraperitoneal hernia model. Langenbecks Arch Surg 397, 283–289 (2012). https://doi.org/10.1007/s00423-011-0858-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0858-8