Abstract
Background
Laparoscopic inguinal hernia repair requires the use of prosthetic material. This prospective, single-center study was intended to investigate the impact of the amount of polypropylene (PP) mesh used in hernia repair on functional results and quality of life.
Methods
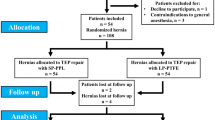
For this series, 672 consecutive patients with primary inguinal hernia undergoing transabdominal preperitoneal hernia repair (TAPP) using a heavyweight PP mesh (Prolene 10 × 15 cm, 1.5 g, group I, n = 232), a mixed PP- and Polyglactin mesh (Vypro II, 10 × 15 cm, 0.53 g, group II, n = 217), or a light-weight titanized PP mesh (Ti-Mesh, 10 × 15 cm, 0.24 g, group III, n = 223) were compared in terms of postoperative complications (seroma, wound healing disorders), quality of life score (pain development, physical condition, urologic disorders), and hernia recurrence.
Results
During a 12-month follow-up there were no significant differences in the recurrence rate (1.3%-1.7%). Patients with a pure PP mesh (group I) showed significantly more postoperative seromas (12.1% versus 4.1%/1.8%), foreign body sensations (9.1% versus 5.5%/3.5%), and sensitivity to weather changes (5.6% versus 3.2%/2.2%) compared to groups II and III. In all groups, the quality of life score was improved postoperatively. However, among those patients in our series with few preoperative complaints, the postoperative quality of life was worsened when heavy-weight PP meshes (group I+II) were used but significantly improved when light-weight titanized PP meshes were used.
Conclusions
Comparable functional results, fewer postoperative complications, and improved quality of life can be achieved by reducing the amount of PP in meshes used for laparoscopic hernia repair by TAPP procedure.



Similar content being viewed by others
References
Klinge U, Junge K, Stumpf M, et al. Functional and morphological evaluation of a lowweight, monofilament polypropylene mesh for hernia repair. J Biomed Mater Res 2002;63:129–136
Junge K, Klinge U, Rosch R, et al. Functional and morphologic properties of a modified mesh for inguinal hernia repair. World J Surg 2002;26:1472–1480
Bittner R, Kraft K, Schmedt CG, et al. Risks and benefits of laparoscopic hernioplasty (TAPP)—5 years of experience in 3,400 hernia repairs. Chirurg 1998;69:854–858
Tamme C, Scheidbach H, Hampe C, et al. Totally extraperitoneal endoscopic inguinal hernia repair (TEP): results of 5,203 hernia repairs. Surg Endosc 2003;17:190–195
Avtan L, Avci C, Bulut T, et al. Mesh infections after laparoscopic inguinal hernia repair. Surg Laparosc Endosc 1997;7:192–195
EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: metaanalysis of randomized controlled trials. Ann Surg 2002;235:322–332
Hume RH, Bour J. Mesh migration following laparoscopic inguinal hernia repair. J Laparoendosc Surg 1996;6:333–335
McCormack K, Scott NW, Go PM, et al. EU Hernia Trialists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 2003;1:CD001785
Klosterhalfen B, Klinge U, Hermanns B, et al. Pathology of traditional surgical nets for hernia repair after long-term implantation in humans. Chirurg 2000;71:43–51
Schumpelick V, Klosterhalfen B, Muller M, et al. Minimized polypropylene mesh for preperitoneal net plasty (PNP) of incisional hernias. Chirurg 1999;70:422–430
Schultz L, Graber J, Pietrafitta J, et al. Laser laparoscopic herniorraphy: a clinical trial preliminary results. J Laparoendosc Surg 1990;1:41–45
Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon Volume and Operative Mortality in the United States. N Engl J Med 2003;22:2117–2127
Koninger J, Redecke J, Butters M. Chronic pain after hernia repair: a randomized trial comparing Shouldice, Lichtenstein and TAPP. Langenbecks Arch Surg 2004;389:361–365
Kumar S, Wilson RG, Nixon SJ, et al. Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 2002;89:1476–1479
Awad SS, Fagan SP. Current approaches to inguinal hernia repair. Am J Surg 2004;188:9S–16S
Bay-Nielsen M, Nilsson E, Nordin P, et al. Swedish Hernia Data Base the Danish Hernia Data Base. Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 2004;91:1372–1376
Bringman S, Heikkinen TJ, Wollert S, et al. Early results of a single-blinded, randomized, controlled, Internet-based multicenter trial comparing Prolene and Vypro II mesh in Lichtenstein hernioplasty. Hernia 2004;8:127–134
Schardey HM, Schopf S, Rudert W, et al. Titanised polypropylene meshes: first clinical experience with the implantation in TAPP technique and the results of a survey in 22 German surgical departments (German). Zentralbl Chir 2004;129:363–368
Schmidbauer S, Ladurner R, Hallfeldt KK, et al. Heavy-weight versus low-weight polypropylene meshes for open sublay mesh repair of incisional hernia. Eur J Med Res 2005;10:247–253
Heikkinen T, Wollert S, Osterberg J, et al. Early results of a randomised trial comparing Prolene and VyproII mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 2005;9:1–7
McCormack K, Wake BL, Fraser C, et al. Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia 2005;9:109–114
Eypasch E, Wood-Dauphinee S, Williams JI, et al. The Gastrointestinal Quality of Life Index. A clinical index for measuring patient status in gastroenterologic surgery. Chirurg 1993;64:264–274
Scheidbach H, Tamme C, Tannapfel A, et al. In vivo studies comparing the biocompatibility of various polypropylene meshes and their handling properties during endoscopic total extraperitoneal (TEP) patchplasty: an experimental study in pigs. Surg Endosc 2004;18:211–220
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horstmann, R., Hellwig, M., Classen, C. et al. Impact of Polypropylene Amount on Functional Outcome and Quality of Life after Inguinal Hernia Repair by the TAPP Procedure Using Pure, Mixed, and Titanium-coated Meshes. World J. Surg. 30, 1742–1749 (2006). https://doi.org/10.1007/s00268-005-0242-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0242-3