Abstract
Purpose
To classify macular neovascularization (MNV) based on pachychoroid and drusen features and to examine the aqueous humor cytokine signatures of each group.
Methods
In total, 106 consecutive eyes with treatment-naïve MNV and 104 control eyes were examined. The aqueous humor concentrations of 15 cytokines were compared among the MNV groups classified based on the presence of drusen and/or pachychoroid features. Multidimensional scaling analysis was used to visualize the similarity level of the MNV subtypes according to their cytokine profiles.
Results
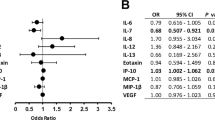
Thirty-one, 18, 43, and 10 eyes were classified into the pachychoroid-associated, drusen-associated, pachychoroid/drusen-associated, and non-drusen/non-pachychoroid MNV groups, respectively. Compared with the control group, cytokines were differently upregulated among the MNV groups. CRP and CXCL12 were significantly upregulated in all MNV groups, whereas CXCL13 and IL-8 were significantly upregulated in three MNV groups, excluding the non-pachychoroid/non-drusen-associated MNV group. Ang-2 was significantly upregulated in three MNV groups except the drusen-associated MNV group. PlGF was significantly upregulated in the pachychoroid-associated and drusen-associated MNV groups. CCL-2 was significantly upregulated in the pachychoroid-associated and pachychoroid/drusen-associated MNV groups. VEGF was downregulated in the pachychoroid-associated and drusen-associated MNV groups, respectively. Multidimensional scaling analysis showed a distinct cytokine profile for each MNV group.
Conclusion
All MNV groups showed distinct cytokine profiles. Eyes with “neovascular age-related macular degeneration with drusen and concomitant pachychoroid” may share a similar etiology to those with “pachychoroid neovasculopathy” and “choroidal neovascularization with drusen,” but have a distinct etiology to those without these. These findings suggest the importance of evaluating drusen and the choroid during the diagnosis of neovascular age-related macular degeneration.




Similar content being viewed by others
References
Maruko I, Iida T, Saito M, Nagayama D, Saito K (2007) Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 144:15–22. https://doi.org/10.1016/j.ajo.2007.03.047
Liu Y, Wen F, Huang S, Luo G, Yan H, Sun Z, Wu D (2007) Subtype lesions of neovascular age-related macular degeneration in Chinese patients. Graefe’s Arch Clin Exp Ophthalmol. 245:1441–1445. https://doi.org/10.1007/s00417-007-0575-8
Takahashi K, Ishibashi T, Ogura Y, Yuzawa M, Working Group for Establishing Diagnostic Criteria for Age-Related Macular Degeneration (2008) Classification and diagnostic criteria of age-related macular degeneration [in Japanese]. Nippon Ganka Gakkai Zasshi. 112:1076–1084
Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, de Jong PTVM, Kalver CCW, Klein BEK, Klein R, Mitchell P, Sarks JP, Sarks SH, Soubrane G, Taylor HR, Vingerling JR, The International ARM Epidemiological study group (1995) An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv Ophthalmol. 39:367–374. https://doi.org/10.1016/s0039-6257(05)80092-x
Warrow DJ, Hoang QV, Freud KB (2013) Pachychoroid pigment epitheliopathy. Retina. 33:1659–1672. https://doi.org/10.1097/IAE.0b013e3182953df4
Balaratnasingam C, Lee WK, Koizumi H, Dansingani K, Inoue M, Freund KB (2016) Polypoidal choroidal vasculopathy: a distinct disease or manifestation of many? Retina. 36:1–8. https://doi.org/10.1097/IAE.0000000000000774
Pang CE, Freund KB (2015) Pachychoroid neovasculopathy. Retina. 35:1–9. https://doi.org/10.1097/IAE.0000000000000331
Fung AT, Yannuzzi LA, Freund KB (2012) Type 1 (sub-retinal pigment epithelial) neovascularization in central serous chorioretinopathy masquerading as neovascular age-related degeneration. Retina. 32:1892–1837. https://doi.org/10.1097/IAE.0b013e3182680a66
Miyake M, Ooto S, Yamashiro K, Takahashi A, Yoshikawa M, Akagi-Kurashige Y, Ueda-Arakawa N, Oishi A, Nakanishi H, Tamura H, Tsujikawa A, Yoshimura N (2015) Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep. 5:16204. https://doi.org/10.1038/srep16204
Matsumoto H, Hiroe T, Morimoto M, Mimura K, Ito A, Akiyama H (2018) Efficacy of treat-and-extend regimen with aflibercept for pachychoroid neovasculopathy and type 1 neovascular age-related macular degeneration. Jpn J Ophthalmol. 62:144–150. https://doi.org/10.1007/s10384-018-0562-0
Terao N, Koizumi H, Kojima K, Yamagishi T, Yamamoto Y, Yoshii K, Kitazawa K, Hiraga A, Toda M, Kinoshita S, Sotozono C, Hamuro J (2018) Distinct aqueous humour cytokine profiles of patients with pachychoroid neovasculopathy and neovascular age-related macular degeneration. Sci Rep. 8:10520. https://doi.org/10.1038/s41598-018-28484-w
Spaide RF (2018) Disease expression in nonexudative age-related macular degeneration varies with choroidal thickness. Retina. 38:708–716. https://doi.org/10.1097/IAE.0000000000001689
Lee J, Byeon SH (2019) Prevalence and clinical characteristics of pachydrusen in polypoidal vasculopathy: Multimodal image study. Retina. 39:670–678. https://doi.org/10.1097/IAE.0000000000002019
Yanagi Y (2020) Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol. 64:323–337. https://doi.org/10.1007/s10384-020-00740-5
Takahashi A, Ooto S, Yamashiro K, Tamura H, Oishi A, Miyata M, Hata M, Yoshikawa M, Yoshimura N, Tsujikawa A (2018) Pachychoroid geographic atrophy: clinical and genetic characteristics. Ophthalmol Retina. 2:295–305. https://doi.org/10.1016/j.oret.2017.08.016
Zweifel SA, Imamura Y, Spaide TC, Fujiwara T, Spaide RF (2010) Prevalence and significance of subretinal drusenoid deposits (reticular pseudodrusen) in age-related macular degeneration. Ophthalmology. 117(9):1775–1781. https://doi.org/10.1016/j.ophtha.2010.01.027
Dansingani KK, Perlee LT, Hamon S, Lee M, Shah VP, Spaide RF, Sorenson J, Klancnik JM Jr, Yannuzzi LA, Barbezetto IA, Cooney MJ, Engelbert M, Chen C, Hewitt AW, Freund KB (2016) Risk alleles associated with neovascularization in a pachychoroid phenotype. Ophthalmology. 123:2628–2630. https://doi.org/10.1016/j.ophtha.2016.06.060
Hata M, Yamashiro K, Ooto S, Oishi A, Tamura H, Miyata M, Ueda-Arakawa N, Takahashi A, Tsujikawa A, Yoshimura N (2017) Intraocular vascular endothelial growth factor levels in pachychoroid neovasculopathy and neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 58:292–298. https://doi.org/10.1167/iovs.16-20967
Zhang ZX, Wang YS, Shi YY, Hou HY, Zhang C, Cai Y, Dou GR, Yao LB, Li FY (2011) Hypoxia specific SDF-1 expression by retinal pigment epithelium initiates bone marrow-derived cells to participate in Choroidal neovascularization in a laser-induced mouse model. Curr Eye Res. 36:838–849. https://doi.org/10.3109/02713683.2011.593107
Kikuchi M, Nakamura M, Ishikawa K, Suzuki T, Nishihara H, Tamakoshi T, Nishio K, Taki K, Niwa T, Hamajima N, Terasaki H (2007) Elevated C-reactive protein levels in patients with polypoidal choroidal vasculopathy and patients with neovascular age-related macular degeneration. Ophthalmology. 114:1722–1727. https://doi.org/10.1016/j.ophtha.2006.12.021
Seddon JM, George S, Rosner B, Rifai N (2005) Progression of age-related macular degeneration: prospective assessment of C-reactive protein, interleukin 6, and other cardiovascular biomarkers. Arch Ophthalmol. 123:774–782. https://doi.org/10.1001/archopht.123.6.774
Vine AK, Stader J, Branham K, Musch DC, Swaroop A (2005) Biomarkers of cardiovascular disease as risk factors for age-related macular degeneration. Ophthalmology. 112:2076–2080. https://doi.org/10.1016/j.ophtha.2005.07.004
Seddon JM, Gensler G, Milton RC, Klein ML, Rifai N (2004) Association between C-reactive protein and age-related macular degeneration. JAMA. 291:704–710. https://doi.org/10.1001/jama.291.6.704
Subhi Y, Nielsen MK, Molbech CR, Oishi A, Singh A, Nissen MH, Sørensen TL (2019) Plasma makers of chronic low-grade inflammation in polypoidal choroidal vasculopathy and neovascular age-related macular degeneration. Acta Ophthalmol. 97:99–106
Sakurada Y, Nakamura Y, Yoneyama S, Mabuchi F, Gotoh T, Tateno Y, Sugiyama A, Kubota T, Iijima H (2015) Aqueous humor cytokine levels in patients with polupoidal choroidal vasculopathy and neovascular age-related macular degeneration. Ophtalmic Res. 53:2–7. https://doi.org/10.1159/000365487
Agrawal R, Balne PK, Wei X, Bijin VA, Lee B, Ghosh A, Narayanan R, Agrawal M, Connolly J (2019) Cytokine profiling in patients with exudative age-related macular degeneration and polypoidal choroidal vasculopathy. Invest Ophalomol Vis Sci. 60:376–382. https://doi.org/10.1167/iovs.18-24387
Spindler J, Zandi S, Pfister IB, Gerhardt C, Garweg JG (2018) Cytokine profiles in the aqueous humor and serum of patients with dry and treated wet age-related macular degeneration. PLoS ONE. 13:e0203337. https://doi.org/10.1371/journal.pone.0203337
Sakamoto S, Takahashi H, Tan X, Inoue Y, Nomura Y, Arai Y, Fujino Y, Kawashima H, Yasuo Y (2018) Changes in multiple cytokine concentrations in the aqueous humour of neovascular age-related macular degeneration after 2 months of ranibizumab therapy. Br J Ophthalmol. 102:448–454. https://doi.org/10.1136/bjophthalmol-2017-310284
Khan M, Aziz AA, Shafi NA, Abbas T, Khanani AM (2020) Targeting angiopoietin in retinal vascular diseases: a literature review and summary of clinical trials involving faricimab. Cells. 9:1869. https://doi.org/10.3390/cells9081869
Dong A, Seidel C, Snell D, Ekawardhani S, Ahlskog JKJ, Baumann M, Shen J, Iwase T, Tian J, Stevens R, Hackett SF, Stumpp MT, Campochiaro PA (2014) Antagonism of PDGF-BB suppresses subretinal neovascularization and enhances the effects of blocking VEGF-A. Angiogenesis. 17:553–562. https://doi.org/10.1007/s10456-013-9402-5
Rakic JM, Lambert V, Devy L, Luttun A, Carmeliet P, Claes C, Nguyen L, Foidart JM, Noёl A, Munaut C (2003) Placental growth factor, a member of the VEGF family, contributes to the development of choroidal neovascularization. Invest Ophthalmol Vis Sci. 44:3186–3193. https://doi.org/10.1167/iovs.02-1092
Nguyen QD, De Falco S, Behar-Cohen F, Lam WC, Li X, Reichhart N, Ricci F, Pluim J, Li WW (2018) Placental growth factor and its potential role in diabetic retinopathy and other ocular neovascular diseases. Acta Ophthalmol. 96:e1–e9. https://doi.org/10.1111/aos.13325
Pongsachareonnont P, Mak MYK, Hurst CP, Lam WC (2018) Neovascular age-related macular degeneration: intraocular inflammatory cytokines in the poor responder to ranibizumab treatment. Clin Ophthalmol. 12:1877–1885. https://doi.org/10.2147/opth.s171636
Jaffe GJ, Eliott D, Wells JA, Prenner JL, Papp A, Patel S (2016) A phase 1 study of intravitreous E10030 in combination with ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 123:78–85. https://doi.org/10.1016/j.ophtha.2015.09.004
Jonas JB, Tao Y, Neumaier M, Findeisen P (2012) Cytokine concentration in aqueous humour eyes with exudative age-related macular degeneration. Acta Ophalmol. 90:e381–e388. https://doi.org/10.1111/j.1755-3768.2012.02414.x
Fukuda Y, Sakurada Y, Yoneyama S, Kikushima W, Sugiyma A, Matsubara M, Tanabe N, Iijima H (2019) Clinical and genetic characteristics of pachydrusen in patients with exudative age-related macular degeneration. Sci Rep. 9:11906. https://doi.org/10.1038/s41598-019-48494-6
Spaide RF (2018) Improving the age-related macular degeneration construct: a new classification system. Retina. 38:891–899. https://doi.org/10.1097/iae.0000000000001732
Cheung CMG, Gan A, Yanagi Y, Wong TY, Spaide R (2018) Association between choroidal thickness and drusen subtype in age-related macular degeneration. Ophthalmol Retina. 2:1196–1205. https://doi.org/10.1016/j.oret.2018.06.014
Abdelsalam A, Del Priore L, Zarbin MA (1991) Drusen in age-related macular degeneration: pathogenesis, natural course, and laser photocoagulation-induced regression. Surv Ophthalmol. 44:1–29. https://doi.org/10.1016/s0039-6257(99)00072-7
Cheung CMG, Lee WK, Koizumi H (2019) Dansingani k, Lai TYY, Freund KB. Pachychoroid disease Eye (Lond). 33:14–33. https://doi.org/10.1038/s41433-018-0158-4
Xu H, Zeng F, Shi D, Sun X, Chen X, Bai Y (2014) Focal choroidal excavation complicated by choroidal neovascularization. Ophthalmology. 121:246–250. https://doi.org/10.1016/j.ophtha.2013.08.014
Lim FPM, Wong CW, Loh BK, Chan CM, Yeo I, Lee SY, Mathur R, Wong D, Wong TY, Cheung CMG (2016) Prevalence and clinical correlates of focal choroidal excavation in eyes with age-related macular degeneration, polypoidal choroidal vasculopathy and central serous chorioretinopathy. Br J Ophthalmol. 100:918–923. https://doi.org/10.1136/bjophthalmol-2015-307055
Chung H, Byeon SH, Freund KB (2017) Focal choroidal excavation and its association with pachychoroid spectrum disorders: a review of the literature and multimodal imaging findings. Retina. 37:199–221. https://doi.org/10.1097/IAE.0000000000001345
Acknowledgements
We thank Satoko Tominaga, Ryota Takahashi, and Kosuke Nagaoka for their participation in this study.
Funding
This work was supported by a KAKENHI grant from the Japan Society for the Promotion of Science, Grant Number 15K10899.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by SI, HT, and YY. The first draft of the manuscript was written by SI. All authors provided input on previous versions of the manuscript and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review boards of the Japan Community Healthcare Organization Tokyo Shinjuku Medical Center and Jichi Medical University (CU20-R007, H22-3)
Consent to participate
Informed consent was obtained from all individual participants included in this study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figures 1a, 1b, and 1c.
Conflict of interest
SI, XT, HT, and YA have no relevant financial or non-financial interests to disclose.
HT is a consultant to Kowa Pharmaceutical, Novartis Pharmaceutical, Bayer Pharmaceutical, Senju Pharmaceutical, Pfizer Pharmaceutica, and Santen Pharmaceutical, and a founder of DeepEyeVision Inc.
YI is a consultant to Novartis Pharmaceuticals, Mitsubishi-Tanabe Pharmaceutical, and the Tochigi Prefectural Ophthalmologists Association.
YY is a consultant to Novartis Pharmaceuticals, Bayer Yakuhin, Santen Pharmaceuticals, and Senju Pharmaceutical.
HK is a consultant to Kowa Pharmaceutical, Novartis Pharmaceuticals, Santen Pharmaceutical, Mitsubishi-Tanabe Pharmaceutical, Senju Pharmaceutical, and the Tochigi Prefectural Ophthalmologists Association.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Inoda, S., Takahashi, H., Inoue, Y. et al. Cytokine profiles of macular neovascularization in the elderly based on a classification from a pachychoroid/drusen perspective. Graefes Arch Clin Exp Ophthalmol 260, 747–758 (2022). https://doi.org/10.1007/s00417-021-05445-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05445-0