Abstract
Purpose
To identify the subtype frequency and clinical features of neovascular age-related macular degeneration (AMD) in Chinese patients.
Methods
From January 2003 to August 2006, we investigated prospectively 155 newly diagnosed patients with presumed neovascular AMD. Fundus fluorescein angiography (FFA) and indocyanine green angiography (ICGA) were performed in both eyes of all patients. Subtype frequency and clinical features were recorded according to their angiograms.
Results
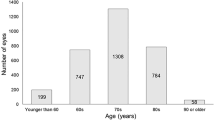
Three subtypes of lesion were noted, which were polypoidal choroidal vasculopathy (PCV), retinal angiomatous proliferation (RAP) and mixed lesions. Of the 155 patients, 105 (67.7%) had choroidal neovascularization (CNV) of the typical type seen in AMD, 38 (24.5%) had PCV and seven (4.5%) had RAP. In five (3.2%) additional cases, mixed lesions were noted. In 38 cases (47 eyes) with PCV, the rates of subfoveal, juxtafoveal and extrafoveal lesion were respectively 29.8% (14 eyes), 8.5% (four eyes), and 61.7% (29 eyes), compared with 75.6%, 14.6% and 9.8% for CNV lesion (P < 0.01). The percentage of subfoveal lesion in PCV group was significantly lower than that in the CNV group (P < 0.01). The location of the RAP lesion was subfoveal in two (28.6%) eyes, juxtafoveal in three (42.9%) eyes and extrafoveal in two (28.6%) eyes. The five eyes with mixed lesions were all PCV coexisting with CNV at the same eye, and in all of the five cases, CNV was subfoveal while PCV was extrafoveal.
Conclusions
In this hospital-based study, PCV accounts for 24.5% of neovascular AMD and is the most common subtype, RAP is less frequent (4.5%), and mixed lesions are much less common in Chinese patients. PCV is least likely to involve the fovea in neovascular AMD.



Similar content being viewed by others
References
Ciardella AP, Donsoff IM, Huang SJ, Costa DL, Yannuzzi LA (2004) Polypoidal choroidal vasculopathy. Surv Ophthalmol 49:25–37
Donati MC, Carifi G, Virgili G, Menchini U (2006) Retinal angiomatous proliferation: association with clinical and angiographic features. Ophthalmologica 220:31–36
Fernandes LH, Freund KB, Yannuzzi LA, Spaide RF, Huang SJ, Slakter JS, Sorenson JA (2002) The nature of focal areas of hyperfluorescence or hot spots imaged with indocyanine green angiography. Retina 22:557–568
Gross NE, Aizman A, Brucker A, Klancnik JM Jr, Yannuzzi LA (2005) Nature and risk of neovascularization in the fellow eye of patients with unilateral retinal angiomatous proliferation. Retina 25:713–718
Hartnett ME, Weiter JJ, Garsd A, Jalkh AE (1992) Classification of retinal pigment epithelial detachments associated with drusen. Graefes Arch Clin Exp Ophthalmol 230:11–19
Hartnett ME, Weiter JJ, Staurenghi G, Elsner AE (1996) Deep retinal vascular anomalous complexes in advanced age-related macular degeneration. Ophthalmology 103:2042–2053
Kuerzinger GR, Lang GK, Lang GE (2006) Retinal angiomatous proliferation in age-related macular degeneration. Klin Monatsbl Augenheilkd 223:691–695
Kuhn D, Meunier I, Soubrane G, Coscas G (1995) Imaging of chorioretinal anastomoses in vascularized retinal pigment epithelium detachments. Arch Ophthalmol 113:1392–1398
Schneider U, Gelisken F, Inhoffen W (2005) Natural course of occult choroidal neovascularization in age-related macular degeneration: development of classic lesions in fluorescein angiography. Acta Ophthalmol Scand 83:141–147
Sho K, Takahashi K, Yamada H, Wada M, Nagai Y, Otsuji T, Nishikawa M, Mitsuma Y, Yamazaki Y, Matsumura M, Uyama M (2003) Polypoidal choroidal vasculopathy: incidence, demographic features, and clinical characteristics. Arch Ophthalmol 121:1392–1396
Slakter JS, Yannuzzi LA, Schneider U, Sorenson JA, Ciardella A, Guyer DR, Spaide RF, Freund KB, Orlock DA (2000) Retinal choroidal anastomoses and occult choroidal neovascularization in age-related macular degeneration. Ophthalmology 107:742–754
Wen F, Chen C, Wu D, Li H (2004) Polypoidal choroidal vasculopathy in elderly Chinese patients. Graefes Arch Clin Exp Ophthalmol 242:625–629
Yannuzzi LA, Negrao S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J, Freund KB, Sorenson J, Orlock D, Borodoker N (2001) Retinal angiomatous proliferation in age-related macular degeneration. Retina 21:416–434
Acknowledgement
This study was supported by the Natural Science Foundation of Guangdong Province (grant no. 04009333) and the Research Fund of Guangdong Bureau of Chinese Medicine (grant no.20030086).
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary interest. This study was supported by the Natural Science Foundation of Guangdong Province (grant no. 04009333) and the Research Fund of Guangdong Bureau of Chinese Medicine (grant no.20030086).
Rights and permissions
About this article
Cite this article
Liu, Y., Wen, F., Huang, S. et al. Subtype lesions of neovascular age-related macular degeneration in Chinese patients. Graefes Arch Clin Exp Ophthalmol 245, 1441–1445 (2007). https://doi.org/10.1007/s00417-007-0575-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-007-0575-8