Abstract
Background
As a secreted protein, cystatin C is assumed to play its role in the extracellular compartment, where it can inhibit virtually all cysteine proteases of families C1 (cathepsin B, L, S) and C13 (mammalian legumain-related proteases). Since many of its potential target enzymes in the eye reside in intracellular compartments, we sought evidence for a cellular uptake of the inhibitor in ocular tissues.
Methods
Fluorescence-labeled human cystatin C was injected intravitreally into normal rat eyes. Ocular tissues were subsequently examined using ELISA, fluorescence microscopy, and immunohistochemistry. Cystatin C uptake was additionally studied in an in vitro retina model.
Results
Cystatin C administered intravitreally in vivo is taken up into cells of the corneal endothelium and epithelium, the epithelial cells lining the ciliary processes, and into cells in the neuroretina (mostly ganglion cells) and the retinal pigment epithelium. The uptake is demonstrable also in vitro and was, in the neuroretina, found to be a high-affinity system, inhibited by cooling the specimens or by adding the microfilament polymerization inhibitor, cytochalasin D, to the medium.
Conclusions
There is an active, temperature-dependent uptake system for cystatin C into several cell types in the cornea, ciliary body, and retina. The cell types that take up cystatin C are generally the same that contain endogenous cystatin C, suggesting that much or all cystatin C seen intracellularly in the normal eye may have been taken up from the surrounding extracellular space. The uptake indicates that the inhibitor may exert biological functions in intracellular compartments. It is also possible that this uptake system may regulate the extracellular levels of cystatin C in the eye.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystatins are important inhibitors regulating papain-like cysteine proteases belonging to enzyme family C1 (see the MEROPS database at http://merops.sanger.ac.uk), such as cathepsins B, H, L, and S and legumain-related proteases in family C13 [2, 11]. All known mammalian cystatins are composed of at least one 100- to 120-amino-acid-residue domain with conserved sequence motifs [25]. Of the 12 human cystatins known, cystatin C is the most extensively studied one, showing a wide-spectrum inhibition profile and high-affinity binding to most C1 cysteine proteases [2].
Cystatin C and other type 2 cystatins (cystatins D, E/M, F, G, S, SN, and SA) are synthesized with 19- to 26-amino-acid-residue-long signal peptides, mediating secretion into the extracellular space [2]. Many different tissues express cystatin C [5], and, as expected for an excreted protein, cystatin C has been detected in all body fluids examined. It is in fact the dominating cysteine protease inhibitor in most mammalian body fluids, present in amounts sufficiently high to allow it to control the extracellular activities of cathepsin B and other important cysteine proteases of family C1 [3]. However, some results imply that cystatin C can be biologically active also intracellularly. For example, cystatins are able to inhibit intracellular replication of polio, herpes simplex and corona viruses [8, 12, 19] as well as virus-induced apoptosis [9]. It is currently not understood how this is achieved.
Being the most important of the regulators of cysteine proteases, the cystatins are likely to play key roles in several normal and pathological states and reactions [2]. Cystatins not only have the capacity to regulate normal body processes and perhaps cause disease when downregulated, but may also participate in the defense against microbial infections. Little is known about its function in the eye, but cystatin C has been detected at both the RNA and protein levels in several ocular tissues, and expressed sequence tags (ESTs) of cystatin C, as well as the protein itself, are particularly prominent in the retinal pigment epithelium [15, 22–24, 27, 28]. Cystatin C mRNA was in one study also detected with in situ hybridization in the neuroretina and sclera [6], but not in the cornea, ciliary body, iris, lens, or choroid, where the protein occurs at significant levels [27, 28]. The discrepancies between the cellular localization of the cystatin C protein and the reported localization of cystatin C mRNA suggest that cystatin C produced in the retina and in cells of the anterior segment is perhaps secreted by some cells and then taken up by the same or neighboring cells, a previously not explored possibility. Since this might explain intracellular activities of cystatin C, and since we have recently seen a putative cellular uptake system for cystatin C in mouse macrophages [Håkansson, Wassélius, Wallin, Ehinger and Abrahamson, unpublished], we chose to look for such a system also in the eye, as well as in other organs. Our results suggest that there is a previously unrecognized active, high-affinity cystatin C uptake system in several ocular cell types, predominantly epithelial cells.
Materials and methods
Fluorescence-labeled cystatin C
Human and rat cystatin C show extensive sequence and structure homology and can be detected by the same antibodies [16]. Even so, it is possible to distinguish human and rat cystatin C using specific monoclonal antibodies [16, 21], which we took advantage of in the present study.
Isolated recombinant human cystatin C was produced in Escherichia coli and isolated as previously described [4]. It was fluorescence labeled using an Alexa-594 protein labeling kit (#A-10239, Molecular Probes, Eugene, OR, USA). Labeled cystatin C was separated from excess dye by size exclusion chromatography on a FPLC Superdex column (Amersham Pharmacia Biotech, Uppsala, Sweden), in 50 mM ammonium bicarbonate buffer, pH 7.8, at a flow rate of 0.5 ml/min. The cystatin C concentration in the purified fraction of labeled protein was determined by A280 measurement [20], Coomassie binding assay with reagent from Pierce (Rockford, IL, USA) [10], and active-site titration of papain [1] to ascertain that the labeled protein was inhibitorily active. The concentration of the fluorophore was determined as advised by Molecular Probes. The majority of experiments were done with a freshly labeled cystatin C protein fraction with a concentration of 1.8 mg/ml, and the labeled portion was determined to 45%, yielding a concentration of Alexa-594-labeled cystatin C of 0.9 mg/ml.
Animals
The experiments and the animal care were according to the “Principles of laboratory animal care” (NIH publication No. 85-23, revised 1985), the OPRR Public Health Service Policy on the Humane Care and Use of Laboratory Animals (revised 1986), the US Animal Welfare Act, as amended, the ARVO statement for the use of animals in ophthalmic and vision research, and approved by the Swedish Committee for Animal Experimentation Ethics.
Normal adult pigmented standard PVG rats were used in the study. The cystatin C knockout mice used to study the uptake of intraperitoneally delivered cystatin C were originally from the C57BL/SV129 black strain and have been described in detail previously [17].
Intraperitoneal injections
Four cystatin C knockout mice from the same litter were lightly anesthetized using halothane gas and injected with 100 μg of recombinantly produced human cystatin C, diluted in 0.1 M phosphate-buffered saline (PBS) at pH 7.4 at a total volume of 0.5 ml. For control purposes, a fifth littermate was injected with 0.5 ml of 0.1 M PBS at pH 7.4. Blood samples for monitoring plasma concentrations of cystatin C were obtained at 30 min and 2, 6, and 24 h Samples were obtained at the same intervals from a normal mouse of the same background strain. Tissue samples were obtained for ELISA in three different knockout mice at 2, 6, and 24 h after similar injections of 2.5 mg of the same cystatin C. One additional knockout mouse was similarly injected with 500 μg of the same cystatin C, and tissue samples were obtained for immunohistochemistry after 24 h.
The animals were killed by carbon dioxide asphyxiation at 2, 6, and 24 h after the injections. Blood was aspirated from the heart and immediately transferred to EDTA tubes. Tissue samples used for protein analyses were immediately frozen on dry ice and kept at −80°C for further preparation. Tissue samples used for immunohistochemistry were fixed at +4°C for 4 h in 4% formaldehyde in 0.1 M phosphate buffer at pH 7.4 and processed for immunohistochemistry.
Intravitreal injections
Intravitreal injections were performed on normal adult rats under general anesthesia (sodium pentobarbital, 30 mg/kg). A Hamilton syringe with 30-gauge disposable needles was used for the injections. In each eye, 5 μl containing 4.5 ng of fluorescence-labeled cystatin C in PBS at pH 7.4 was injected. For control purposes, similar injections were made on littermates with PBS, as well as with the unconjugated Alexa-594 fluorophore, at a corresponding concentration, in PBS.
The animals were killed by carbon dioxide asphyxiation 1, 6, 24, or 48 h after the injections. At every time point, three eyes were used for immunohistochemistry and three eyes were used for protein analysis. After enucleation, the eyes used for histology were perforated with a needle to enable the fixative to penetrate rapidly into the eyes. Tissues were fixed in darkness at +4°C for 4 h in 4% formaldehyde in 0.1 M PBS at pH 7.4, and further processed for immunohistochemistry. Tissues used for protein analyses were rapidly dissected, and the corneas, the ciliary bodies and the retinas instantly frozen on dry ice and kept at −80°C until further processed.
Retina in vitro experiments
Retinas were cultured as previously described in detail [19]. Freshly enucleated adult eyes were immersed in cold Dulbecco’s modified Eagle’s medium (Sigma-Aldrich, Gillingham, UK) external tissue was removed, and the retinas were explanted onto Millicell-HA 0.45-μm inserts (Millipore, Bedford, MA, USA) with the vitreal side up. Explants of retinas were cultured at +37°C with 95% humidity and 5% CO2. l-Glutamine, penicillin, and streptomycin (Sigma-Aldrich) were added to the medium.
The tissues intended for histology were fixed in darkness at +4°C for 4 h in 4% formaldehyde in 0.1 M phosphate buffer at pH 7.4 and further processed for immunohistochemistry. Tissues used for protein analyses were instantly frozen on dry ice and kept at −80°C awaiting further processing.
Recombinantly produced human cystatin C was added in concentrations between 0.0026 and 0.26 μM to the culture medium. After 24 h, the cystatin C uptake was analyzed by ELISA measurements of washed cells, using lysis buffer as previously described [7]. The results were then plotted in a Lineweaver–Burk plot to determine the maximal uptake rate and the Michaelis constant (KM) for the uptake.
To study whether the uptake of cystatin C by the cells was an active mechanism, retinas were cultured at +4°C for 24 h with cystatin C (0.026 μM) in the medium. Other retinas were preincubated with 100 μM of the actin depolymerizing agent cytochalasin D for 30 min at +37°C before incubating with cystatin C for 24 h at +37°C. This concentration was in pilot experiments found to give significant inhibition of the uptake.
Cystatin C ELISA
Human cystatin C concentrations were determined by a double-sandwich ELISA specific for human cystatin C as previously described [21]. The cystatin C concentration was related to total protein concentration in the homogenates, the latter measured by a dye-binding assay [10].
Immunohistochemistry and antibodies
Cryostat sectioning (12 μm) and immunolabeling were performed with standard procedures. The monoclonal antibody used to specifically detect human cystatin C was raised in mouse against human cystatin C [21]. The monospecific polyclonal rabbit antibody used for species-neutral cystatin C immunohistochemistry was raised in rabbit against human cystatin C [3]. Secondary antibodies conjugated with FITC were obtained from Jackson Immuno Research Laboratories (West Grove, PA, USA), DAKO A/S (Glostrup, Denmark), and Sigma (St. Louis, MO, USA).
Immunohistochemistry control experiments included using different secondary antibodies and primary antibody omission.
Microscopy and image analysis
The specimens were examined using a Nikon Diaphot 300/Bio-Rad MRC1024 confocal laser scanning microscope and a Nikon Eclipse E800 microscope equipped with an Optronix DEI-750 digital image acquisition system. Images were viewed and processed using Confocal Assistant (copyright Todd Clark Brelje) and Adobe Photoshop (Adobe Systems, Mountain View, CA, USA).
Results
Intraperitoneal injections
In the initial exploratory assays of blood concentrations after intraperitoneal injections of cystatin C in mice, plasma levels reached about 33 ng/ml at 30 min and 2 h, then dropped to about 4 ng/ml at 6 h and were undetectable (<0.5 ng/ml) at 24 h, as in the sham-injected control animal. The levels reached are roughly in the same order of magnitude as previously published values for normal mice [16]. The samples were too few to allow a formal statistical evaluation, but the coefficient of variation was in all cases less than 15%. Plasma and tissue levels did not run in parallel. The tissues often showed the highest levels after 2 and 6 h (Fig. 1), whereas plasma levels had decreased at 6 h. The levels reached are in the same order of magnitude as the normal tissue levels in mice, 10–50 ng/mg protein in most tissues and close to 300 ng/mg protein in brain [16]. The observation suggests an efficient systemic distribution and retention of cystatin C in many tissues.
Cystatin C levels in tissues from cystatin C knockout mice injected intraperitoneally with 100 μg recombinant human cystatin C. The bars show mean values from duplicate ELISA measurements. The coefficient of variation (standard deviation/mean) was in all cases below 15%. In all but one of the tissues tested, there was no detectable cystatin C in sham-injected knockout mice (“PB 2h”; note the absence of columns in all tissues except liver, where a very small and most likely insignificant level was seen).
Granular cystatin C immunoreactivity was seen in cells in the retina, kidney, salivary gland, spleen, and thymus (Fig. 2), as well as in the liver, testicles, and brain (not illustrated) of cystatin C knockout mice that had received cystatin C. No cystatin C could be detected by immunohistochemistry (not illustrated) in an animal that had received a control injection of PBS. In the mice that received small doses of cystatin C (100 μg), immunoreactivity was found chiefly in the kidney, located in a pattern similar to that in the high-dose animals (not illustrated).
Cystatin C immunofluorescence in various tissues from a cystatin C knockout mouse, 2 h after an intraperitoneal injection of 2.5 mg recombinant human cystatin C. a The inner retina, where immunoreactivity can be seen in occasional ganglion cells (arrow) and occasional cells in the inner nuclear layer (arrowhead). b The outer retina where the cystatin C immunoreactivity is localized to the retinal pigment epithelial cells. c Kidney. Note the unlabeled glomerulus (G). d Spleen. e A salivary gland. f Thymus. Confocal micrographs, representative for examinations of at least five sections from each of at least two tissue pieces. Scale bars 30 μm.
In the cystatin C knockout mouse eyes into which a high dose of recombinant cystatin C had been injected, cystatin C immunoreactivity was seen in occasional cells in the ganglion cell layer and in the retinal pigment epithelium (Fig. 2b). In the kidney (Fig. 2c), cystatin C immunoreactivity was found in the tubuli, leaving the glomeruli unstained. A large proportion of the cells in the spleen showed cystatin C immunoreactivity (Fig. 2d). In the salivary glands, cystatin C immunoreactivity was seen in cytoplasmic granules in various cells evenly distributed in the glands (Fig. 2e). In the thymus, cystatin C was seen in the cytoplasm of occasional cells. In all cells the immunoreactivity was localized to the cytoplasm, generally in cytoplasmic granules, leaving the nuclei unstained.
Intravitreal injections
In rats, recombinant human cystatin C was injected intravitreally in order to investigate the handling of extracellularly added cystatin C in the eye in vivo. Tissue uptake could be detected and monitored, using a specific human cystatin C ELISA, in the cornea, ciliary body, and retina (Fig. 3).
Generally, the highest levels were measured 1 and 6 h after the injection. For the cornea and ciliary body, the levels were lower after 24 h, but in the retina, the levels were not significantly changed at that time. After 48 h, the levels were markedly reduced at all locations. No human cystatin C was detected in the ocular tissues from control animals injected with PBS (Fig. 3).
In animals that had received Alexa-594-labeled cystatin C by intravitreal injection, only a diffuse and weak specific fluorescence and immunoreactivity was present in the cornea, the ciliary body and the retina after 1 h. However, 6 and 24 h after the injections, Alexa-594 fluorescence was seen in the cytoplasm of cells in the cornea, ciliary body, and retina. The fluorescence was confirmed to emanate from the injected human recombinant cystatin C by using a monoclonal antibody, specific for human cystatin C (Figs. 4 and 5). Except in the Descemet’s membrane, the Alexa-594 fluorescence agreed with the immunohistochemical labeling in all tissue parts.
Tissues from a rat eye injected with 4.5 ng Alexa-594-labeled human cystatin C. Note the labeling of epithelial and endothelial cells in the cornea (a, arrows and arrowheads), epithelial cells lining the ciliary processes (b, examples at the arrows), and in the retina (c) in the cytoplasm of cells in the ganglion cell layer (arrows at examples), the inner nuclear layer (small arrowheads), and the pigment epithelial cells (large arrowheads). The sections were all stained for human cystatin C with FITC immunohistochemistry and also examined for Alexa-594 fluorescence. The two labels coincided precisely, except in the Bowman’s membrane in the cornea (large arrowheads in a), which was labeled by Alexa-594 (not illustrated), but did not show any specific human cystatin C immunoreactivity. Only one of the two labeling types is therefore shown, FITC in a and b, and Alexa-594 in c. Confocal micrographs. Scale bars: a 30, b 50,c 50 μm.
Normal rat retina cultured in vitro for 24 h with addition of Alexa-594-labeled recombinant human cystatin C, at 0.026 μM, in the culture medium. a Human cystatin C immunoreactivity. b Alexa-594 fluorescence. Note that most cells in the ganglion cell layer and in the inner nuclear layer show both human cystatin C immunoreactivity and Alexa-594 fluorescence (arrows), but occasional cells in the ganglion call layer and in the inner nuclear layer show human cystatin C immunoreactivity without any detectable Alexa-594 fluorescence (small arrowheads). Uptake of cystatin C in Müller cells was also detectable (large arrowheads). Confocal micrograph. Scale bars 30 μm.
In the cornea (Fig. 4a), the cytoplasm of the basal layers of epithelial cells was labeled. There was no discernible difference between the center and the periphery. In the endothelium, the cytoplasm of all cells appeared to be labeled. The fluorescence was strongest 6 h after injection, markedly reduced after 24 h, and eliminated after 48 h.
Descemet’s membrane was labeled by Alexa-594 (not illustrated), but most likely this was due to unconjugated Alexa-594 fluorophores bound to the membrane, since this structure was labeled also by the unconjugated fluorophore, injected intravitreally for control purposes. There was no immunohistochemical labeling of this structure using the specific monoclonal antibody for human cystatin C (Fig. 4a).
In the ciliary body, the fluorescence was seen in the cytoplasm of the superficial layer of epithelial cells lining the ciliary processes (Fig. 4b). No other specific fluorescence was seen in the ciliary body or processes. The specific labeling was detectable 6 and 24 h after injection but not after 48 h.
In the retina, fluorescence was seen 6 and 24 h after the injection (Fig. 4c), and after 48 h it had essentially been eliminated. The labeling was localized to cells in the ganglion cell layer, cells in the inner nuclear layer and to most or all retinal pigment epithelial cells. Immunohistochemistry specific for the detection of human cystatin C correlated with the observed fluorescence.
There was no detectable uptake of unconjugated Alexa-594 fluorophores in the ciliary body or in the retina. No specific fluorescence could be detected histologically or immunohistochemically in the ocular tissues of the sham-injected eyes.
In vitro experiments
Retinas of normal adult rats were cultured with human Alexa-594 cystatin C (0.026 μM) added to the medium. There was no fluorescence or cystatin C immunoreactivity seen intracellularly in the retinas cultured for 1 h, but there was a diffuse immunoreactivity present in the entire tissue that was not present in control specimens (not illustrated). After 6, 24, and 48 h, human cystatin C immunoreactivity and Alexa-594 fluorescence was present in the cytoplasm of cells in the ganglion cell layer and in the inner nuclear layer (Fig. 5).
Usually, more cells were labeled in the ganglion cell layer and the inner nuclear layer than in the in vivo experiments. Unlike in the in vivo experiments, Müller cells in the cultured retinas also showed human cystatin C immunoreactivity (Fig. 5).After culture for 48 h, both the direct fluorescence and the immunoreactivity were significantly reduced, but the distribution of the labels were the same.
The results of ELISA measurements on homogenates of retinas cultured with human cystatin C in the medium showed that the cystatin C concentration in the tissue increased with increasing medium concentrations of cystatin C (2.6–260 nM). When plotted in a Lineweaver–Burk plot, the results are compatible with a single uptake mechanism with a maximal uptake rate of about 50 ng cystatin C/mg cellular protein in 24 h, and a Michaelis constant (KM) of 0.04 μM (Fig. 6).
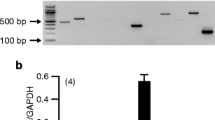
The in vitro cystatin C uptake was significantly inhibited by either cooling the preparation to +4°C or preincubating the retinas in cytochalasin D (Fig. 7).
Effect of cooling and cytochalasin D on the uptake of cystatin C into retina in vitro. Retinas were cultured at +37 and +4°C for 24 h with cystatin C (0,026 μM) in the medium. In the cytochalasin D experiments, retinas were first incubated in 100 μM of the substance for 30 min at +37°C before incubating them with cystatin C for 24 h at +37°C.
Discussion
Human and rat cystatin C show extensive sequence and structure homology and have virtually identical functional properties as cysteine protease inhibitors [16]. They also have similar distribution patterns in the eye [28]. Nevertheless, they are different enough to be distinguishable with specific antibodies. It is thus possible to locate and quantitate human cystatin C accumulated in normal rat tissues, containing endogenous rat cystatin C, and we took advantage of this possibility.
It is unlikely that the cystatin C detected intracellularly in this study is degraded, since the double-sandwich ELISA technique requires each cystatin C molecule to be recognized by two antibodies to generate a signal, and the two antibodies used detect amino acid sequences at the two ends of the molecule. Furthermore, Western blotting experiments have shown that human cystatin C taken up by macrophages is indeed intact [Håkansson, Wassélius, Wallin, Ehinger and Abrahamson, unpublished], as is endogenously produced rat or mouse cystatin C found intracellularly in the normal retina [28].
Our pilot experiments with cystatin C injected intraperitoneally in cystatin C knockout mice suggest that it can be readily transported into the systemic circulation and taken up and retained by cells in various tissues, including the retina. This opens the possibility that the cystatin C present in the retina of wild-type mice might have been taken up from the systemic circulation or other extracellular sources.
Intravitreal administration of cystatin C in the rat eye
Histologically, human cystatin C is directly observable in the tissues without further processing when labeled with Alexa-594. With immunohistochemistry, we could verify that the observed fluorescence was in fact emanating from the labeled human cystatin C, by using a specific monoclonal antibody against human cystatin C (Figs. 2, 4 and 5) that does not cross-react with rat cystatin C [16]. The observation also suggests that the cystatin C detected was not much degraded, because the Alexa-594 label is not likely to sit exclusively at the site detected by the antibody. Furthermore, we used a polyclonal cystatin C antibody that recognizes human as well as rat cystatin C [28], labeling both endogenous and administered cystatin C, allowing us to see whether there were cells containing rat cystatin C that had not taken up the labeled human cystatin C. In the retina, we found only a few such cells, located in the ganglion cell layer and in the inner nuclear layer (Fig. 5). In the cornea and ciliary body no such cells were found.
One hour after intravitreal injection, only a weak, diffuse specific immunoreactivity was seen in the tissues. This suggests that the labeled cystatin C may have diffused to the extracellular space of the tissues, but had not yet been taken up by the cells. Six, twenty-four and forty-eight hours after injection, the injected fluorescence-labeled cystatin C was localized to the cytoplasm of cells in cornea, ciliary body, and retina. The general localization pattern much resembled that seen for cystatin C in the wild-type rat cornea, ciliary body, and retina [27, 28].
In general, the ELISA results correlate well with our histological findings. The high levels detected 1 h after administration correspond to a diffuse immunoreactivity, as expected if the injected cystatin first diffuses into the tissue before being taken up. It is then apparently stored in cytoplasmic granular organelles. Attempts to identify these organelles have given ambiguous results, not presented here. Our experiments thus show that certain cells in the eye have mechanisms for the uptake, retention, and at least short-term storage (several hours) of cystatin C in vivo.
Cystatin C uptake in vitro in the rat retina
Histologically, the results from the in vitro experiments gave results similar to those obtained for in vivo experiments. Generally, there were more labeled cells in the cultured retinas (Fig. 5) than in the retinas exposed to cystatin C injected intravitreally in vivo. This might be an effect of the altered condition of the in vitro system, such as the dissection trauma, factors in the culturing medium, or better accessibility to the cystatin C in the medium than to cystatin C injected in the vitreous body in the in vivo experiments, as well as the activation of cystatin C containing microglial cells that has been demonstrated in the in vitro retina culturing model [14].
Our quantitative results from the in vitro experiments, plotted in a Lineweaver–Burk plot, suggest a single-component uptake system with a Michaelis constant (KM) of 0.04 μM and with a maximal uptake rate of about 50 ng cystatin C/mg cellular protein in 24 h (Fig. 6). Our results further show that the cystatin C uptake into the retina is an active and presumably energy-requiring process, since it can be significantly reduced by lowering the culture temperature to +4°C, or by preincubating the retina with the actin-depolymerizing agent, cytochalasin D (Fig. 7). The cystatin C concentrations in these experiments (0.0026–0.26 μM) is certainly at a physiological level, well below the concentrations of cystatin C in blood plasma, cerebrospinal fluid, and seminal plasma [3].
Concluding remarks
Cystatin C has previously been demonstrated at both the protein and RNA level in rat and mouse retina [15, 22–24, 27, 28] as well as in epithelial cells in the cornea, lens, and ciliary body [27]. We here show that several of the same cell types in the cornea, ciliary body, and retina of the rat eye in vivo have the capability to take up and store recombinant human cystatin C injected into the vitreous body. The uptake is demonstrable by both histochemistry and a double-sandwich ELISA, and since the results with the two methods agree well and the ELISA does not detect cystatin C fragments, we believe it likely that the fluorescence microscopy essentially shows the distribution of unchanged cystatin C.
Assuming a total volume of 50 μl for a rat eye, the concentration of the injected cystatin C equals ∼1.3 μM if distributed in the entire eye, which is slightly above the concentration in cerebrospinal fluid, and well below that in seminal plasma [3]. It is thus within a physiological concentration range. When characterizing the uptake system in a retina in vitro culturing system, we found that the uptake of cystatin C can be inhibited by culturing the retina at +4°C or by preincubating the retina with the microfilament polymerization inhibitor, cytochalasin D. This is as expected for an active uptake system. Furthermore, in a pilot experiment we observed that cystatin C injected into the peritoneal cavity of cystatin C knockout mice can be transferred into the systemic circulation and taken up by other tissues, including the retina. Taken together, the results indicate that a physiologically relevant active cellular uptake system for cystatin C exists in ocular tissues. To our knowledge, no such uptake system has previously been described for cystatins in mammalian cells or tissues.
There are large similarities in localization patterns in the rat retina, cornea, and ciliary body of exogenously administered cystatin C, native cystatin C, and cystatin C mRNA [27, 28]. This raises the possibility that some or all of the cystatin C that can be detected within rat eye cells may have been taken up from the extracellular space. The presence of cystatin C mRNA in the cornea, the ciliary body, and the retina shows that the cystatin C gene is transcribed in these tissues. It is thus possible that cystatin C is secreted and taken up by the same cells that produce it and/or by neighboring cells. We find it worth noting that this is what is actually required for an efficient and tightly regulated control system: cystatin C is released when needed extracellularly, and when no longer needed, it is taken back up into cell stores from which it can be reused.
Another obvious consequence of the transport system described here is that it provides a mechanism allowing intracellular actions of cystatin C. This may explain why cystatin C can inhibit intracellular replication of herpes simplex [8] and corona viruses [12]. It may also be involved in regulating intracellular cathepsin B activity in ailments like keratoconus and acute infectious keratitis, diseases in which mainly intracellular cathepsin B appears to be upregulated [13, 26].
References
Abrahamson M (1994) Cystatins. Methods Enzymol 244:685–700
Abrahamson M, Alvarez-Fernandez M, Nathanson CM (2003) Cystatins. Biochem Soc Symp 70:179–199
Abrahamson M, Barrett AJ, Salvesen G, Grubb A (1986) Isolation of six cysteine proteinase inhibitors from human urine. Their physicochemical and enzyme kinetic properties and concentrations in biological fluids. J Biol Chem 261:11282–11289
Abrahamson M, Dalboge H, Olafsson I, Carlsen S, Grubb A (1988) Efficient production of native, biologically active human cystatin C by Escherichia coli. FEBS Lett 236:14–18
Abrahamson M, Olafsson I, Palsdottir A, Ulvsback M, Lundwall A, Jensson O, Grubb A (1990) Structure and expression of the human cystatin C gene. Biochem J 268:287–294
Barka T, van der Noen H (1994) Expression of the cysteine proteinase inhibitor cystatin C mRNA in rat eye. Anat Rec 239:343–348
Bjarnadottir M, Wulff BS, Sameni M, Sloane BF, Keppler D, Grubb A, Abrahamson M (1998) Intracellular accumulation of the amyloidogenic L68Q variant of human cystatin C in NIH/3T3 cells. Mol Pathol 51:317–326
Björck L, Grubb A, Kjellén L (1990) Cystatin C, a human proteinase inhibitor, blocks replication of herpes simplex virus. J Virol 64:941–943
Bjorklund HV, Johansson TR, Rinne A (1997) Rhabdovirus-induced apoptosis in a fish cell line is inhibited by a human endogenous acid cysteine proteinase inhibitor. J Virol 71:5658–5662
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254
Brown WM, Dziegielewska KM (1997) Friends and relations of the cystatin superfamily—new members and their evolution. Protein Sci 6:5–12
Collins AR, Grubb A (1991) Inhibitory effects of recombinant human cystatin C on human coronaviruses. Antimicrob Agents Chemother 35:2444–2446
Dong Z, Katar M, Linebaugh BE, Sloane BF, Berk RS (2001) Expression of cathepsins B, D and L in mouse corneas infected with Pseudomonas aeruginosa. Eur J Biochem 268:6408–6416
Engelsberg K, Ehinger B, Wasselius J, Johansson K (2004) Apoptotic cell death and microglial cell responses in cultured rat retina. Graefes Arch Clin Exp Ophthalmol 242:229–239
Gieser L, Swaroop A (1992) Expressed sequence tags and chromosomal localization of cDNA clones from a subtracted retinal pigment epithelium library. Genomics 13:873–876
Håkansson K, Huh C, Grubb A, Karlsson S, Abrahamson M (1996) Mouse and rat cystatin C: Escherichia coli production, characterization and tissue distribution. Comp Biochem Physiol, Part B Biochem Mol Biol 114:303–311
Huh CG, Håkansson K, Nathanson CM, Thorgeirsson UP, Jonsson N, Grubb A, Abrahamson M, Karlsson S (1999) Decreased metastatic spread in mice homozygous for a null allele of the cystatin C protease inhibitor gene. Mol Pathol 52:332–340
Johansson K, Bruun A, Grasbon T, Ehinger B (2000) Growth of postnatal rat retina in vitro. Development of neurotransmitter systems. J Chem Neuroanat 19:117–128
Korant BD, Brzin J, Turk V (1985) Cystatin, a protein inhibitor of cysteine proteases alters viral protein cleavages in infected human cells. Biochem Biophys Res Commun 127:1072–1076
Lindahl P, Abrahamson M, Bjork I (1992) Interaction of recombinant human cystatin C with the cysteine proteinases papain and actinidin. Biochem J 281:49–55
Olafsson I, Löfberg H, Abrahamson M, Grubb A (1988) Production, characterization and use of monoclonal antibodies against the major extracellular human cysteine proteinase inhibitors cystatin C and kininogen. Scand J Clin Lab Invest 48:573–582
Paraoan L, Grierson I, Maden BE (2000) Analysis of expressed sequence tags of retinal pigment epithelium: cystatin C is an abundant transcript. Int J Biochem Cell Biol 32:417–426
Paraoan L, Grierson I, Maden BE (2003) Fate of cystatin C lacking the leader sequence in RPE cells. Exp Eye Res 76:753–756
Paraoan L, White MR, Spiller DG, Grierson I, Maden BE (2001) Precursor cystatin C in cultured retinal pigment epithelium cells: evidence for processing through the secretory pathway. Mol Membr Biol 18:229–236
Rawlings ND, Barrett AJ (1990) Evolution of proteins of the cystatin superfamily. J Mol Evol 30:60–71
Sherwin T, Brookes NH, Loh IP, Poole CA, Clover GM (2002) Cellular incursion into Bowman’s membrane in the peripheral cone of the keratoconic cornea. Exp Eye Res 74:473–482
Wassélius J, Håkansson K, Abrahamson M, Ehinger B (2004) Cystatin C in the anterior segment of rat and mouse eyes. Acta Ophthalmol Scand 82:68–75
Wassélius J, Håkansson K, Johansson K, Abrahamson M, Ehinger B (2001) Identification and localization of retinal cystatin C. Invest Ophthalmol Vis Sci 42:1901–1906
Acknowledgements
Supported by The Foundation Fighting Blindness, the Knut and Alice Wallenberg Foundation, The Crafoord Foundation, The Anna-Greta Crafoord Foundation for Rheumatology Research, The Crown Princess Margareta Foundation, The A. Österlund Foundation, ONCE, the Swedish Medical Research Council (projects 13X-09915 and 14X-2321) and the Faculty of Medicine at the University of Lund.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial relationship with the organizations that sponsored the research
Rights and permissions
About this article
Cite this article
Wassélius, J., Johansson, K., Håkansson, K. et al. Cystatin C uptake in the eye. Graefe's Arch Clin Exp Ophthalmol 243, 583–592 (2005). https://doi.org/10.1007/s00417-004-1055-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-1055-z