Abstract
Background
Older general hospital patients, particularly those with cognitive impairment, frequently experience adverse events and other care complications during their stay. As these findings have so far been based on small and selected patient samples, the aim of the present study was to provide reliable data on a) the prevalence of adverse care issues (summarized under the term care challenges) in older general hospital patients and on b) associated patient-related risk factors (e.g. cognitive impairment).
Methods
A cross-sectional representative study comprising 1469 patients aged ≥65 years from 33 randomly selected general hospitals in southern Germany (GHoSt). Data collection included the use of different data sources, e.g. structured interviews with responsible nursing staff concerning care challenges and procedures for determining the patients’ cognitive status.
Results
Care challenges were statistically significantly (p < 0.001) more often reported for patients with dementia and/or delirium (87.5%) and mild cognitive impairment (47.9%) compared to cognitively unimpaired patients (24.6%). Adjusted odds ratios suggested cognitive impairment, impaired activities of daily living, receiving long-term care and unplanned admission as significant patient-related risk factors for care challenges. Furthermore, the occurrence of such issues was associated with the application of physical restraints, support from relatives, prescription of psycholeptics and specialist consultations.
Conclusion
The findings suggest a strong impact of different degrees of cognitive impairment on challenges in care. The results might help to design appropriate training programs for hospital staff and other interventions to prevent or reduce critical situations.
Zusammenfassung
Hintergrund
Für ältere Allgemeinkrankenhauspatienten werden häufig unerwünschte Ereignisse und Probleme in der Versorgung während ihres Aufenthaltes berichtet, v. a. bei kognitiv beeinträchtigten Patienten. Die Befunde basieren jedoch auf kleinen und selektiven Stichproben. Ziel dieser Studie ist es, zuverlässige Daten a) zur Prävalenz solcher Versorgungsprobleme (zusammengefasst als „herausfordernde Pflegesituationen“) und b) zu assoziierten patientenbezogenen Risikofaktoren (v. a. kognitive Beeinträchtigung) zu gewinnen.
Methoden
Die repräsentative Querschnittsstudie umfasst 1469 65-jährige und ältere Patienten in 33 zufällig ausgewählten Allgemeinkrankenhäusern in Süddeutschland (General Hospital Study, GHoSt). Informationsquellen waren u. a. eine standardisierte Befragung der jeweils verantwortlichen Pflegefachkraft und Verfahren zur Feststellung des kognitiven Status.
Ergebnisse
Im Vergleich zu kognitiv unbeeinträchtigten Patienten (24,6 %) wurden herausfordernde Pflegesituationen statistisch signifikant (p < 0,001) häufiger bei Patienten mit Demenz/Delir (87,5 %) und mit leichter kognitiver Beeinträchtigung (47,9 %) berichtet. Adjustierte „odds ratios“ bestätigten kognitive Beeinträchtigung, eingeschränkte Alltagskompetenz, Bezug von Pflegeleistungen und ungeplante Aufnahme als Risikofaktoren. Versorgungsprobleme waren zudem häufiger assoziiert mit freiheitsentziehenden Maßnahmen, Angehörigeneinbindung in die Pflege, Verordnung von Psycholeptika und Konsilien.
Diskussion
Die Befunde belegen den deutlichen Einfluss verschiedener Grade kognitiver Beeinträchtigung auf herausfordernde Pflegesituationen. Die Ergebnisse können dazu beitragen, geeignete Schulungsprogramme und Interventionen zu konzipieren, um kritische Situationen zu vermeiden oder zu minimieren.
Similar content being viewed by others
Background
Adverse events (e.g. falls) and other care complications (e.g. noncompliant behavior) may render hospital stays of older adults distressing and lead to serious consequences, not only for the patients themselves but also for their relatives and hospital staff [9]. While these occurrences are associated with secondary harm to patient health, increased length of stay and other negative consequences [3, 4, 18, 32], they also pose substantial challenges and stress to hospital staff [12, 21]. In particular, wandering, activity disturbances, aggression, sleep disturbances, and fending off help with eating showed a significant impact on staff daily routines [28, 29]. The relevance of these problems seems to increase in the presence of cognitive impairment [13, 28, 32].
Reliable key data about the frequency and distribution of adverse care issues are essential, given the pressing need to improve the quality of hospital care of older patients. As the previous findings were based on international studies with small and highly selected samples, it is unclear how common these care problems really are and whether the available findings also pertain to general hospitals in Germany. In addition, the applied methods and definitions of adverse events, care problems, and care complications varied widely across studies.
The aim of this study was to determine a) the prevalence of care challenges in older general hospital patients and b) the associations of these challenges with different degrees of cognitive impairment and other patient-related risk factors (e.g. demographics, degree of functional impairment). The term care challenges summarizes a variety of adverse events and other care issues on the level of everyday experiences of patients and hospital staff.
Material and methods
Sampling
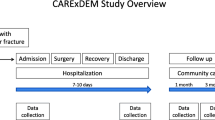
Data were taken from the General Hospital Study (GHoSt), which is a cross-sectional representative study of patients aged ≥65 years in randomly selected general hospitals in southern Germany [2, 19]. There were inclusion and exclusion criteria on the hospital level, ward level and patient level. Small hospitals (<150 beds), specialized hospitals (e.g. psychiatric clinics), rehabilitation and day or night clinics were excluded. On the ward level, intensive care units, isolation, pediatric, geriatric, neurological and psychiatric wards were not considered. Exclusion criteria on the patient level were age under 65 years, critical condition, isolation because of an infectious disease, and insufficient proficiency in the German language.
A multistep sampling procedure was applied. First, all general hospitals meeting the inclusion criteria were put into a random order, contacted according to this order and asked for participation until the previously set number of 33 hospitals were achieved. Second, in each participating hospital five wards and one substitute ward meeting the criteria were randomly chosen. Trained research assistants visited one ward each day in the survey week. They asked all inpatients fulfilling the inclusion criteria or their legal representatives for informed consent to participate in the study.
The ethics committee of the Faculty of Medicine of the Technical University of Munich approved the study protocol (No. 66/14) and the study was registered in the German Registry of Clinical Studies under DRKS00006028. The survey was conducted between June 2014 and May 2015.
Data collection
On the survey day the research assistants a) asked each patient or a respective knowledgeable informant about demographic data, b) conducted a structured bedside examination (for more details see [2]), c) conducted a standardized interview for each participating patient with the responsible nurse concerning the patient’s status of activities of daily living (ADL), psychosocial characteristics (e.g. visits and support from relatives), medical and care features (e.g. anesthesia, application of physical restraints), and care challenges observed since patient admission and d) collected relevant information from each patient’s medical records, e.g. admission reason, prescription of psycholeptics (group N05 according to Anatomic Therapeutic Chemical classification system [ATC]) and analgesics (ATC group N02). The selection of care challenges (see Table 2) was based on previous reports of general hospital staff [12, 24, 29, 31]. As the items were based on the everyday experience of the hospital staff rather than on clinical concepts, the ratings can be assumed to have a higher reliability [26].
Global severity of cognitive impairment was rated with the clinical dementia rating scale (CDR [22]). Patients with a CDR score of 0 were considered to be cognitively unimpaired and patients with a CDR score of 0.5 to have mild cognitive impairment. Patients with CDR score of 1 (mild dementia and/or delirium), 2 (moderate dementia and/or delirium) or 3 (severe dementia and/or delirium) were summarized under the term dementia and/or delirium. Dementia was diagnosed according to Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) criteria and delirium was assessed by means of the confusion assessment method [23].
Statistical analysis
The care challenge items were dichotomized to present vs. not present. The 95% confidence intervals (CI) of the frequencies were calculated according to the Wilson score method [7]. Differences between the examined patient groups were assessed with analyses of variance (ANOVA), Pearson’s χ2-tests or Fisher’s exact tests. Associations between ≥1 reported care challenge and patient-related risk factors, e.g. age, gender, cognitive status, residential situation, receiving long-term care (LTC) benefits, unplanned admission, department and ADL were examined with univariate binary logistic regressions analyses. Multivariate logistic regression analysis was calculated with patient-related risk factors as predictors entered in one block. The statistically significantly predictors from this analysis were then used as covariates in multivariate logistic regression analyses examining the association of severity of cognitive impairment with the occurrence of specific care challenges as individual outcomes. In addition, univariate binary logistic regressions analyses were calculated with care and medical treatment characteristics to examine the associations with ≥1 reported care challenge. Using logistic generalized estimation equation (GEE) models ensured taking the cluster structure of the study into account.
Results
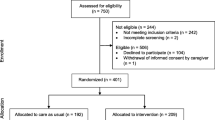
The participation rate of the hospitals was 60% (33 out of 55) and the response rate on the patient level was 68.2%. On the specific days of survey 2534 patients aged 65 years or older were registered on the visited wards: 380 patients could not be asked for participation as they were isolated, repeatedly not present, in a critical condition or out of other reasons and 685 patients refused participation or their legal representative refused or could not be reached. One patient was excluded because there was insufficient information to determine the cognitive status with the CDR. The final sample consisted of 1468 patients aged 65–105 years (mean 78.6 years, SD 7.4 years) and 53.8% were female. The median time of inpatient stay to survey day was 5 days (range 1–95 days, interquartile range 2–9 days). The three cognitive impairment groups differed with respect to age, receiving LTC benefits, need of assistance in basic care, residential situation, unplanned admission, prescription of psycholeptics, application of physical restraints, and support from relatives (Table 1).
Any care challenge was reported for 42% of the total sample (Table 2). The responsible nurses reported needing more time for caring than usual in 20% of the patients. In addition, 18% of the patients showed sleep disturbances and 17.4% were fending off medical nursing or forgot to take their medication. Limited communication ability was reported for 13.7% of the patients, implying that they were not able to understand questions, follow instructions and/or express their needs and wishes.
For half of the patients with mild cognitive impairment and for 87.5% of patients with dementia and/or delirium nursing staff reported at least 1 care challenge compared to 24.6% in the cognitively unimpaired group (Table 2). Prevalence rates and differences in the frequency of single care challenges according to the grade of dementia and/or delirium are shown in Table 3. The number of care challenges significantly increased with the severity of cognitive impairment. Cognitively unimpaired patients had a mean of 0.41 care challenges per hospital stay (SD 0.90, range 0–8), patients with mild cognitive impairment a mean of 1.06 (1.55; 0–9), patients with mild dementia and/or delirium a mean of 2.07 (2.10, 0–9), and patients with moderate dementia and/or delirium a mean of 3.82 (2.56, 0–10). Finally, patients with severe dementia and/or delirium had an average of 5.04 care challenges (2.38, 1–11).
Univariate binary logistic regression analyses revealed statistically significant associations of the presence of ≥1 reported care challenge(s) with dementia and/or delirium, mild cognitive impairment and a lower ADL score (Table 4). With these models the highest proportion (31%) of the variance was explained (Nagelkerke’s R2 = 0.31). For the adjusted model all factors were entered simultaneously. Dementia and/or delirium, mild cognitive impairment, lower ADL, getting long-term care benefits, and unplanned admission remained statistically significant predictors. The adjusted model increased the explained variance to 40%. These factors were selected for analysis to examine associations of the different types of care challenges.
Detailed examination of the impact of dementia and/or delirium on showing ≥1 care challenge(s) revealed a higher risk for patients with mild dementia and/or delirium (odds ratio, OR 4.56, 95% confidence interval, CI 2.68–7.75) and for patients with moderate and severe grades of dementia and/or delirium (OR 25.5; 95% CI 10.1–64.5) compared to the cognitively unimpaired patients. Patients with care challenges showed a high probability for specific care and medical treatment characteristics (Table 5). There was a 70.9 times higher risk for physical restraints and a 4.1 times higher risk for the prescription of psycholeptics. Getting support from relatives in the hospital as well as geriatric/neurological/psychiatric consultations were also more likely for patients with care challenges.
Analyses of the different types of care challenges revealed that all care challenges were associated with cognitive impairment, in particular with dementia and/or delirium (Table 6). When adjusting for ADL score, unplanned admission and receiving LTC benefits, nearly all care challenges remained significantly associated with dementia and/or delirium. Beside dementia and/or delirium only a lower level of ADL remained an independent risk factor for all care challenges. Similar logistic regression analyses for patients with mild cognitive impairment showed weak but significant associations with some care challenges.
Discussion
With respect to the study aims it was found that the prevalence rate of one or more reported care challenge(s) in older general hospital patients was 42.0%. This finding confirms the clinical relevance of the concept of care challenges based on everyday experiences of the hospital staff. Furthermore, care challenges in general were closely related to the severity of cognitive impairment. The overall prevalence rate of care challenges increased from 24.6% among cognitively unimpaired patients up to 100% in the group with severe dementia and/or delirium. This emphasizes the enormous impact of cognitive impairment, in particular advanced dementia (with or without delirium) on the care situation. The results are in line with previous studies reporting high rates of adverse outcomes, ranging from more acute healthcare problems (i.e. delirium, falls, pain) and care problems to elevated rates of mortality and institutionalization after discharge [11, 18, 32]. In addition, the findings suggest that mild cognitive impairment already has a detrimental influence on the care situation. Significant relationships with severity of cognitive impairment could be determined for almost all examined single care challenges even after adjustment for ADL score and other significant patient-related factors. Thereby, the present study adds more reliable and detailed information to the as yet limited knowledge of problems in every day hospital routines concerning patients with cognitive impairment [9, 12, 20, 24, 29, 31].
Needing more caring time than usual was reported for 20% of older patients in general and for 57% of the patients with dementia and/or delirium. These findings may justify programs of adjusted staff allocation for care-intensive patients in general hospitals, especially for those with cognitive impairments. In Germany, a legal prerequisite for such targeted improvement of staffing conditions for the most vulnerable groups in acute hospital settings came into force on January 2019 [5].
Besides cognitive impairment, lower ADL level, unplanned hospital admission, and receiving LTC benefits were related to care challenges. These variables might be easily recognized at hospital admission by using simple screening procedures and could serve as risk indicators for upcoming care challenges and health problems. The strong associations of lower ADL level not only with the presence of any care challenge but also with most of specific challenges illustrate the known feeling among nursing staff of being challenged by patients’ noncompliant behaviour with respect to eating/drinking, washing and taking medication [12].
The persistently low but statistically significant association of unplanned admission with the overall presence of care challenges may be due to the severe medical crisis of emergency patients, which is often associated with distress and anxiety up to acute confusion of the patients leading to subsequent care challenges. Furthermore, the study found significant associations between care and medical treatment factors and care challenges. Patients with reported care challenges had a significantly higher risk of being physically restrained and receiving psycholeptics. The prescription of sedative substances is often the only yet insufficient possibility for hospital staff to manage challenging behaviour [12]. Using physical restraints is an undesirable procedure as it may lead to agitation, confusion, functional decline, pressure ulcer, strangulation, death, and adverse psychological effects [16]. The finding that patients with care challenges received more often help and assistance from relatives in the hospital, highlights the value of the triad of patient, staff, and family carers [1].
In general, the results serve to facilitate the effective and broader implementation of approaches which have been proved in model projects to optimize hospital care of vulnerable patient groups [6, 8, 15, 17, 20, 25, 27, 30], and to establish the knowledge of a more person-centered care culture in nonspecialized hospital settings [9, 10]. Indicating frequent, but unsolved problems in the daily care of cognitive impaired patients provides a basis for development of staff training programs. For example, limited ability of patients to communicate their needs and wishes was reported as a frequent care challenge of patients with dementia and/or delirium. In a previous study, the hospital staff themselves underlined the need to enhance the awareness for nonverbal aspects of communication and to apply special communication tools during medical procedures in order to help patients accept the procedures and to avoid or reduce negative consequences [14].
Strength and limitations
The strength of this study is the large number of older patients from a random sample of general hospitals of two southern states in Germany. In contrast, previous studies examined highly selected groups in single general hospitals, often with special features, such as unplanned hospital stay [13, 32]. A further strength of the study is the use of multiple information sources, including comprehensive interviews with responsible nurses concerning care challenges of each participating patient. In contrast, some previous studies were based on administrative reports of adverse events to the hospital management [32] or expert interviews and staff surveys [12, 24, 31]. Furthermore, interviews were based on the more comprehensive concept of care challenges in everyday care and not only on single adverse events or on the psychiatric concept of behavioral and psychological symptoms of dementia (BPSD) [31].
Generalizability is limited by a priori exclusion of intensive care units, geriatric, neurological, and psychiatric hospitals and units, where reported care challenges may be even more frequent in comparison to other departments. Also, results concerning care challenges are based on the reports of nursing staff and subjected to a number of biases (e.g. social desirability, errors in recognition and judgement).
Practical recommendations
There is an urgent need to strengthen general hospitals in preventing and managing care challenges, for example by targeted allocation of staff, dementia-friendly and delirium-managing interventions, and specific training programs. Knowledge of risk factors for care challenge helps to identify vulnerable patients and to minimize critical events and secondary harm to patients’ health. Patients with milder cognitive impairment constitute a yet barely recognized patient group, which also confronts hospital staff with care challenges.
References
Beardon S, Patel K, Davies B, Ward H (2018) Informal carers’ perspectives on the delivery of acute hospital care for patients with dementia. BMC Geriatr 18:23
Bickel H, Hendlmeier I, Heßler JB, Junge MN, Leonhardt-Achilles S, Weber J, Schäufele M (2018) The prevalence of dementia and cognitive impairment in hospitals. Dtsch Arztebl Int 115:733–740
Bradshaw LE, Goldberg SE, Lewis SA, Whittamore K, Gladman JRF, Jones RG, Harwood RH (2013) Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing 42:582–588
Briggs R, Dyer A, Nabeel S, Collings R, Doherty J, Coughlan T, O’Neill D, Kennelly SP (2017) Dementia in the acute hospital: the prevalence and clinical outcomes of acutely unwell patients with dementia. QJM 110:33–37
Bundesministerium für Gesundheit (2018) Spürbare Verbesserungen seit 1. Januar 2019 – Das ändert sich für gesetzlich Versicherte. www.bundesgesundheitsministerium.de/verbesserungen-2019.html#c14310. Accessed 8 July 2019
Büter K, Motzek T, Dietz B, Hofrichter L, Junge M, Kopf D, von Lutzau-Hohlbein H, Traxler S, Zieschang T, Marquardt G (2017) Dementia-friendly hospital wards. Z Gerontol Geriatr 50:67–72
Dean AG, Sullivan KM, Soe MM (2013) OpenEpi: Open Source Epidemiologic Statistics for Publik Health, Version 2.3.1. www.openepi.com. Accessed 8 July 2019
Deutsche Krankenhausgesellschaft (2019) Best-Practice-Beispiele Demenz. www.dkgev.de/themen/versorgung-struktur/versorgungsformen/demenz/best-practice-beispiele-demenz. Accessed 8 July 2019
Dewing J, Dijk S (2016) What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia (London) 15:106–124
Elvish R, Burrow S, Cawley R, Harney K, Pilling M, Gregory J, Keady J (2018) Getting to know me. Dementia (London) 17:96–109
Fogg C, Meredith P, Bridges J, Could GP, Griffith P (2017) The relationship between cognitive impairment, mortality and discharge characteristics in a lager cohort of older adults with unscheduled admissions to an acute hospital: a retroperspective observational study. Age Ageing 46:794–801
Gladman J, Porock D, Griffiths A, Clissett P, Harwood RH, Knight A, Jurgens FJ, Jones R, Schneider J, Kearney F (2012) Better mental health: care for older people with cognitive impairment in general hospitals (NIHR project 08/1809/227)
Glover A, Bradshaw LE, Watson N, Laithwaite E, Goldberg SE, Whittamore KH, Harwood RH (2014) Diagnoses, problems and healthcare interventions amongst older people with an unscheduled hospital admission who have concurrent mental health problems. BMC Geriatr 14:43
Griffiths A, Knight A, Harwood R, Gladman JRF (2014) Preparation to care for confused older patients in general hospitals: a study of UK health professionals. Age Ageing 43:521–527
Gurlit S, Thiesemann R, Wolff B, Brommer J, Gogol M (2013) Caring for people with dementia in general hospitals: an education curriculum from the Alzheimer’s Society of Lower Saxony, Germany. Z Gerontol Geriatr 46:222–225
Hamers JPH, Huizing AR (2005) Why do we use physical restraints in the elderly? Z Gerontol Geriatr 38:19–25
Handley M, Bunn F, Goodman C (2017) Dementia-friendly interventions to improve the care of people living with dementia admitted to hospitals. BMJ Open 7:e15257
Hartley P, Gibbins N, Saunders A, Alexander K, Conroy E, Dixon R, Lang J, Luckett J, Luddington T, Romero-Ortuno R (2017) The association between cognitive impairment and functional outcome in hospitalised older patients. Age Ageing 46:559–567
Hendlmeier I, Bickel H, Hessler JB, Weber J, Junge MN, Leonhardt S, Schäufele M (2018) Demenzsensible Versorgungsangebote im Allgemeinkrankenhaus. Z Gerontol Geriatr 51:509–516
Hennig A, Geschke K, Landua P (2015) Demenzkompetenz im Krankenhaus. www.lzg-rlp.de/de/multiplikatorenschulungen-demenz-im-krankenhaus-667.html. Accessed 8 July 2019
Hessler JB, Schäufele M, Hendlmeier I, Junge MN, Leonhardt S, Weber J, Bickel H (2017) Behavioural and psychological symptoms in general hospital patients with dementia, distress for nursing staff and complications in care. Epidemiol Psychiatr Sci 27:278–287
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL (1982) A new clinical scale for the staging of dementia. Br J Psychiatry 140:566–572
Inouye SK, Van Dyck CH, Alessi CA, Balkon S, Siegal AP, Horwitz RI (1990) Clarifying confusion—the confusion assessment method—a new method for detection of delirium. Ann Intern Med 113:941–948
Isfort M, Klostermann J et al (2014) Pflege-Thermometer 2014. www.dip.de/fileadmin/data/pdf/projekte/Pflege-Thermometer_2014.pdf. Accessed 8 July 2019
Kirchen-Peters S, Diefenbacher A (2014) Gerontopsychiatrische Konsiliar- und Liaisondienste. Eine Antwort auf die Herausforderung Demenz? Z Gerontol Geriatr 47:595–604
Magaziner J (1997) Use of proxies to measure health and functional outcomes in effectiveness research in persons with Alzheimer disease and related disorders. Alzheimer Dis Assoc Disord 11:168–174
Robert-Bosch Stiftung (2019) Menschen mit Demenz im Akutkrankenhaus. www.bosch-stiftung.de/de/projekt/menschen-mit-demenz-im-akutkrankenhaus/gefoerderte-projekte. Accessed 8 July 2019
Sampson EL, White N, Leurent B, Scott S, Lord K, Round J, Jones L (2014) Behavioural and psychiatric symptoms in people with dementia admitted to the acute hospital. Br J Psychiatry 205:189–196
Schütz D, Füsgen I (2013) Die Versorgungssituation kognitiv eingeschränkter Patienten im Krankenhaus. Z Gerontol Geriatr 46:203–207
Singler K, Thomas C (2017) HELP – Hospital Elder Life Program – ein multimodales Interventionsprogramm zur Delirprävention bei älteren Patienten. Internist 58:125–131
Teschauer W, Hambloch C, Wagner G (2017) Abschlussbericht Menschen mit Demenz im Krankenhaus – Deutsche Alzheimer Gesellschaft Landesverband Bayern. www.dkgev.de/media/file/71281.Abschlussbericht_Phase_III.pdf. Accessed 8 July 2019
Watkin L, Blanchard MR, Tookman A, Sampson EL (2012) Prospective cohort study of adverse events in older people admitted to the acute general hospital: risk factors and the impact of dementia. Int J Geriatr Psychiatry 27:76–82
Acknowledgements
We are grateful to the Robert Bosch Foundation, Stuttgart, for funding the General Hospital Study. Additional support was provided by the Deutsche Alzheimer Gesellschaft, Berlin. The open access publication of this article is supported by Robert Bosch Stiftung. We thank research assistants Magdalena Junge, Sarah Leonhardt-Achilles, and Joshua Weber for recruitment and data collection. Our sincere thanks also go to the general hospitals, staff members, patients and their relatives for participating in the study.
Author information
Authors and Affiliations
Contributions
H. Bickel, M. Schäufele, and I. Hendlmeier were primarily responsible for study design and data preparation. I. Hendlmeier, J.B. Heßler-Kaufmann and research assistants carried out recruitment and data collection. I. Hendlmeier analyzed the data for this study and drafted the manuscript. All authors participated in data interpretation and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
I. Hendlmeier, H. Bickel, J.B. Heßler-Kaufmann and M. Schäufele declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This study was approved by the ethics committee of the Faculty of Medicine of the Technical University of Munich (No. 66/14). The supplement containing this article is not sponsored by industry.
Rights and permissions
Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hendlmeier, I., Bickel, H., Heßler-Kaufmann, J.B. et al. Care challenges in older general hospital patients. Z Gerontol Geriat 52 (Suppl 4), 212–221 (2019). https://doi.org/10.1007/s00391-019-01628-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-019-01628-x