Abstract
Background
Frail older people with mental health problems including delirium, dementia and depression are often admitted to general hospitals. However, hospital admission may cause distress, and can be associated with complications. Some commentators suggest that their healthcare needs could be better met elsewhere.
Methods
We studied consecutive patients aged 70 or older admitted for emergency medical or trauma care to an 1800 bed general hospital which provided sole emergency medical and trauma services for its local population. Patients were screened for mental health problems, and those screening positive were invited to take part. 250 participants were recruited and a sub-sample of 53 patients was assessed by a geriatrician for diagnoses, impairments and disabilities, healthcare interventions and outstanding needs.
Results
Median age was 86 years, median Mini-Mental State Examination score at admission was 16/30, and 45% had delirium. 19% lived in a care home prior to admission. All the patients were complex. A wide range of main admission diagnoses was recorded, and these were usually complicated by falls, immobility, pain, delirium, dehydration or incontinence. There was a median of six active diagnoses, and eight active problems. One quarter of problems was unexplained. A median of 13 interventions was recorded, and a median of a further four interventions suggested by the geriatrician. Those with more severe cognitive impairment had no less medical need.
Conclusions
This patient group, admitted to hospital in the United Kingdom, had numerous healthcare problems, and by implication, extensive healthcare needs. Patients with simpler conditions were not identified, but may have already been rapidly discharged or redirected to non-hospital services by the time assessments were made. To meet the needs of this group outside the hospital would need considerable investment in medical, nursing, therapy and diagnostic facilities. In the meantime, acute hospitals should adapt to deliver comprehensive geriatric assessment, and provide for their mental health needs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
General hospitals may fail to meet all the needs of older people with co-morbid mental and behavioural disorders, including cognitive impairment, mood, alcohol problems and psychosis [1]. Two-thirds of older people in hospital have a mental disorder [2]. Twenty-five per cent of acute hospital beds accommodate someone with dementia, a proportion likely to rise given the ageing population and increasing prevalence of dementia [1, 3]. A third of all patients admitted to general hospitals for acute care have delirium or dementia [4–7]. People with dementia are 1.4–3.6 times more likely to be admitted to hospital than age-matched controls [8, 9]. Delirium is common in hospitalised older patients, especially those with dementia [10]. Both delirium and dementia are associated with excess mortality and the need for institutionalisation [4, 6–8, 11, 12]. Much emphasis has been placed on mental health assessment and the provision of appropriate psychological and emotional care [2, 13]. However, there has been little investigation of medical needs in this population.
Several large studies have looked at reasons for admission in people with dementia, basing their data on discharge or insurance records [8, 9]. Pneumonia, urinary tract infections (UTI), falls and fractures are all common diagnoses [8, 14–16]. It has been suggested that some patients are admitted unnecessarily, with conditions which could have been prevented or treated in primary care. These ‘ambulatory care sensitive conditions’ (ACSC) [17] may represent 40% of admissions of people with dementia [4]. Diagnoses reported to lead to admission are dependent on service configuration and data collection methods, and vary greatly between published studies. There is also a problem in assigning a single reason for admission in frail older adults, for whom comorbidity is common, and presentations often non-specific [18].
There is a debate about where frail older people who have combinations of problems affecting their physical and mental health should be treated [19]. With increasing emphasis on, and provision of, community services giving alternatives to hospital admission, the number and case mix of patients is likely to change over time, making up-to-date information important in providing services. We aimed to document diagnoses, problems, and healthcare interventions undergone by a sample of patients admitted to an acute general hospital who were identified as having a concurrent mental health diagnosis.
Methods
Study population
We recruited participants from two sites of an 1800-bed teaching hospital providing sole general medical and trauma services for a population of approximately 660,000 [5, 20]. Consecutive patients aged over 70 with an unplanned admission lasting two or more days, were screened for inclusion if admitted to one of 12 wards, comprising two trauma orthopaedic, three acute geriatric medical and seven general medical wards. Those with a possible mental health diagnosis were identified by responses on the Abbreviated Mental Test score [21], four-point Geriatric Depression Score [22], CAGE alcoholism questions [23] and a question asking if there was any other reason to suspect a mental health diagnosis, and were invited to take part in the study. Written consent was taken from patients who had mental capacity; otherwise agreement was gained from a personal consultee (a family member or other individual, who, under English Mental Capacity law, can give agreement to a person taking part in research if they lack capacity). Fifty- three patients underwent a clinical assessment by a geriatrician. They were selected opportunistically, depending on availability of the research doctors, and all agreed to take part.
Assessments
Participants, and a family carer where one was available and willing, were interviewed by a researcher, who also examined the case notes. They completed a battery of standardised health status measures, including admission problems, drugs, severity of medical illness (Modified Early Warning Score [24]), cognition (Mini-Mental State Examination, MMSE [25]), delirium (Delirium Rating Scale, DRS-R-98 [26]), mood (Cornell Scale for Depression in Dementia [27]), behavioural and psychological symptoms (Neuropsychiatric Inventory [28]), and physical disability (Barthel Index [29]).
Patients sub-sampled for diagnostic assessment were separately and independently assessed by one of three geriatricians, one consultant and two senior trainees. They were asked to complete a clinical assessment at the level expected for a thorough ward consultation, by examining case notes and investigations, talking to the patient and carers, and undertaking any further clinical examination required. No additional investigations were ordered. Proformas were completed detailing diagnoses, problems, social situation and contextual factors, interventions, including drugs stopped and started, and outstanding healthcare needs. Diagnoses were further classified as active, potentially active or inactive (at any time during the index admission), and level of diagnostic certainty as definite, probably or possible. Problems were defined clinically as issues considered important for the management of the case, and broadly represented risk factors, impairments or functional problems (activity limitations), and were qualified as explained or unexplained. Healthcare interventions undertaken by doctors, nurses and allied health professionals were noted if they were recorded in the case notes.
After hospital discharge professional coders routinely assigned a main admission diagnosis, working to a national coding manual, independently of clinicians and research assessments.
Analysis
The population was described in terms of demographic features and measured health status. Diagnoses were coded according to the International Classification of Diseases 10th edition (ICD-10) [30], function using the International Classification of Functioning, Disability and Health (ICF) [31], and healthcare interventions using a bespoke hierarchical classification system. ACSC were identified using published criteria [17].
We calculated median numbers of diagnoses, problems and interventions, the prevalence of common diagnoses, and differences according to severity of cognitive impairment (MMSE score greater than 15 vs less than or equal to 15).
Ethical approval
The study was approved by a research ethics committee approved for considering research on people lacking mental capacity (Nottingham 1 REC 08/H1302/127).
Results
Recruitment
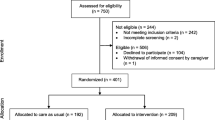
Between April and November 2009 1004 patients were screened; 361 (36%) had no evidence of mental health disorder, 195 declined consent or consultee agreement, 61 had no contactable carer; 108 were excluded as they did not have capacity and we were unable to contact a carer prior to discharge; 8 were too ill and 21 were not recruited for other reasons. Two hundred and fifty were recruited and assessed at baseline for the main study. Fifty- three of these participants underwent a clinical assessment by a geriatrician. Median time after admission to geriatrician assessment was seven days (range 2–15, Inter Quartile Range, IQR, 6–10).
Patient characteristics
Patients who were assessed by a geriatrician were similar to those who were not, apart from a greater proportion presenting with a fall (64% v 42%) and more having become immobile (74% v 58%; Table 1). One hundred and nine patients (44%) had an MMSE of 15 or less.
Coded admission diagnosis
The most common coded diagnosis among the whole cohort was fracture of the femur, followed by UTI, ‘senility’ and pneumonia (Table 2). UTI and pneumonia were more common in patients with lower MMSE scores; heart failure and chronic obstructive pulmonary disease (COPD) were less common.
Thirty (12%) coded admission diagnoses were for ‘ambulatory care sensitive conditions’, and these were more frequent if MMSE ≤15 (relative risk 2.6, 95% CI 1.3–5.3).
Geriatrician-assessed presenting diagnosis and problems
Following geriatrician assessment it was not always possible to assign a single main diagnosis. The main diagnoses were fractured neck of femur 7; other fractures 6; pneumonia 4; multifactorial fall 4; multifactorial functional problem 3; atrial fibrillation with fast ventricular response 3; dehydration/renal failure 3; UTI 1; alcohol intoxication 2; adverse drug reaction 2; seizures 2; unresponsive episode 2; painful hip post fall 2; unexplained delirium 2; cancer 2; exacerbation of COPD 1; infected leg ulcer 1; gastroenteritis 1; stroke 1; ruptured Achilles tendon 1; rheumatoid arthritis 1; progression of vascular dementia 1; acute urinary retention 1; anxiety 1.
Assessed presenting functional problems were immobility 38 (73%), falls 34 (64%), pain 28 (54%), incontinence 24 (46%), breathlessness 12 (23%), increased confusion 11 (21%), and dehydration 11 (21%).
Multiple pathologies
The number of diagnoses per patient ranged from 5 to 19 with a median of 9 (IQR 6–10). Seventy-nine per cent were rated definite, 17% probable and 4% possible. 43% of diagnoses were active, 25% potentially active, and 31% inactive. This did not differ greatly by ward type (Table 3). The total number of active or potentially active diagnoses ranged from 2 to 16 with a median of 6 (IQR 5–8). The most common diagnoses were dementia, falls and musculoskeletal problems (Table 4). The only diagnosis significantly more common in patients with a low MMSE score was dementia.
Problems
Five hundred and seventeen problems were recorded; 418 were abnormalities of body function (ICF b-codes), 5 abnormalities of body structure (s-codes) and 94 activity limitations (d-codes). The median number per patient was 9 (range 5–19). Functional problems were more common on geriatric and orthopaedic wards than general medical wards (median 10 v 7; Table 3). Seventy-five per cent of problems were explained: 89% on geriatric medical, 69% on orthopaedic, 63% on general medical wards. The most common impairments were in cognition (70%), walking (70%), postural stability (58%), transfers (55%), pain (55%) and continence (49%; Table 5). Cognitive impairment, apathy, urinary and faecal incontinence were more common in those with a lower MMSE score.
Interventions
In total 727 interventions were recorded (Table 6). Patients received a median of 13 recorded interventions (range 6–30) with a further four (range 0–26) recommended following geriatrician assessment. Twenty-five patients had medications stopped (mean 2.2 per patient), and 40 patients had new medications started (mean 2.8 per patient).
Discussion
Summary of findings
This study found that the main diagnosis assessed by a geriatrician as causing the hospital admission was varied, and sometimes difficult to assign. Musculoskeletal problems and dementia were very common. Functional problems and complications such as falls, immobility, incontinence and delirium were almost universal, and often multiple. Other than the preponderance of fracture and injury on trauma orthopaedic wards prevalence of both diagnoses and problems did not vary greatly by ward type. Some differences in diagnoses were evident in the group with the most severe cognitive impairment, including a higher proportion categorised as ‘ambulatory care sensitive conditions’, but if anything this group had more, not fewer, functional problems. A wide range of multidisciplinary interventions was delivered in hospital, and further interventions were recommended following assessment by a geriatrician, including starting and stopping medication, nursing and therapist interventions, family discussions, and follow up. Routine coding often differed from that recorded after geriatrician assessment.
Strengths and weaknesses
A strength of this study is that it was based on comprehensive assessment rather than coded discharge diagnoses or insurance records and therefore was able to capture the complexity of the patient cohort. The study was conducted in a single UK National Health Service Hospital Trust, which provided sole emergency medical services for its local population. For practical reasons we recruited from only three of five geriatric medical wards, seven of eleven general medical wards, and two of three trauma orthopaedic wards. The study was relatively small, since assessments were time consuming. We did not recruit from specialist stroke, renal, neurology, cardiology, haematology, oncology or infectious diseases wards. The particular local configuration of these services will have influenced case mix, and limits generalisability, although we attempted to make the study as representative of ‘unselected’ general medical, geriatric and trauma cases as is possible in a modern health service.
Assessments were made about one week into the admission, by which point approximately one-third of participants recruited to the study had been discharged [5]. The time delay allowed an overview of sometimes fast-moving and fluid diagnostic formulations, but patients with simpler or transient problems amenable to alternative care outside the hospital will have been excluded, and trauma and falls were over-represented. We also excluded from recruitment those thought imminently likely to die.
Data predated the introduction of a routine orthogeriatric liaison service. Assessments were made by experienced geriatricians on the basis of clinical opinion, but research diagnostic criteria were not used. Diagnoses and problems were considered important to managing the case, but it was difficult to ascertain all problems without a direct functional assessment, nor to describe problems and interventions to a consistent degree of detail. For example, mobility problems might be broken down into bed mobility, transfers, and walking. Much routine nursing activity was not recorded, such as encouragement to eat or help using the toilet. Complex chains of diagnoses, consequences and complications could arise; for example, pneumonia may be complicated by delirium and a fall which results in a fracture. Any of these might be considered the ‘main’ diagnosis. ICD-10 is mostly a classification of pathologies, but includes some ‘functional diagnoses’ such as falls or incontinence, which also appear in ICF. Classification to one of these diagnoses sometimes depends on whether an alternative pathological diagnosis was available, or whether the problems had been identified and recorded in case notes, which can be inconsistent. For most participants, but not all, a mental health diagnosis was identified by the geriatrician. Those that did not may have recovered from delirium, or have been a false positive on initial screening, for example, due to the overlap between the effects of physical and mental illness. No inter-rater reliability testing was undertaken.
Interpretation and context
It has been suggested that many patients with dementia are admitted with conditions that could have been prevented or managed outside the hospital [19]. This was confirmed by this study according to proposed criteria: ‘conditions for which hospital admission could be prevented by interventions in primary care’ [17]. Typically, however, older people present with non-specific functional problems such as immobility or falls which may be contributed to by several diagnoses, and the functional problems drive admissions rather than individual diagnoses. Functional decline creates acute dependency (sudden need for increased human help) and makes discharge difficult [32]. Patients with memory problems are likely to struggle in proactively managing their own medical conditions. Structured interviews with providers of hospital and community services for older patients have identified ‘internal’ and ‘external’ factors triggering hospital admission. Internal factors included features such as stoicism and reluctance to seek early medical help. External factors included access to alternative provision which tended to be complex making it difficult for patients to know where to seek help [33]. Proactive services such as community matrons (specialist community nurses) can help meet this medical need [34], but identifying all those at risk of hospital admission, and intervening successfully to prevent it, remains difficult [35, 36].
Our findings are not consistent with the suggestion that large numbers of older adults with mental health problems are being admitted with little medical need. In the geographical area and hospital studied this may indicate that systems to avoid unnecessary admission and to enable early discharge were operating successfully. A variety of alternative models to hospital inpatient care has been described, including short stay assessment units, and intermediate care [37–41]. This study was unable to assess if length of hospital stay was appropriate or justified, or if care could have been provided in other settings. But the prevalence of impairments such as immobility, falls, delirium and incontinence implies the need for skilled nursing and rehabilitation, and the number of active medical problems suggests the need for medical diagnosis and management.
The tendency of older patients to present with non-specific and functional problems, to have multiple pathologies, to be prone to complications, lose abilities quickly when ill, and need explicit rehabilitation is well established [42]. Hospitalisation allows for comprehensive geriatric assessment (CGA), which high quality evidence demonstrates increases the chances of survival and regaining independence following illness [43, 44].
Future work
Our findings suggest that alternatives to hospital must have access to clinicians specialising in geriatric medicine and psychiatry, access to diagnostic technology, and the provision of intensive skilled nursing and rehabilitation. This level of care may be difficult to achieve cost-effectively outside of traditional hospitals. If this is the case, hospitals should be reformed to make them better able to meet the needs of elderly service users. For example, systems are needed to provide comprehensive geriatric assessment and multi-disciplinary management, there should be adequate provision of expert mental health care, and the environment and procedures need to be adapted for those with sensory or cognitive impairment. Rehabilitation and end of live care are required as well as acute medical or surgical care. Provision should be made for close communication and working with families and other informal carers [1, 2, 43–50]. Work is needed to define the limits of achievable care provision out of hospital, and to improve both outcomes and experiences of hospital care for frail older people. The study also suggests that routine diagnostic coding and information systems need to change to describe frail elderly patients better, in particular to include non-specific presentations and functional information, if they are to serve the needs of service planning and evaluation.
Conclusions
Older people who are admitted to a general hospital and found to have co-morbid mental health problems also had many physical diagnoses and functional problems, and by implication extensive healthcare needs. Patients with simpler ‘ambulatory sensitive’ conditions were not identified, but may have already been rapidly discharged or redirected to non-hospital services by the time assessments were made. To meet the needs of this group outside the hospital would need considerable investment in medical, nursing, therapy and diagnostic facilities. In the meantime, acute hospitals (and alternative facilities) should adapt to make their environment and systems more appropriate for frail older people, to deliver comprehensive geriatric assessment, and provide for their mental health needs.
Abbreviations
- ACSC:
-
Ambulatory care sensitive condition
- CAGE:
-
(mnemonic) screening tool for alcoholism
- CGA:
-
Comprehensive geriatric assessment
- COPD:
-
Chronic obstructive pulmonary disease
- DRS-R-98:
-
Delirium Rating Scale
- ICD-10:
-
International Classification of Diseases 10th edition
- ICF:
-
International Classification of Functioning, Disability and Health
- IQR:
-
Inter Quartile Range
- MMSE:
-
Mini-Mental State Examination
- NPI:
-
Neuropsychiatric inventory
- UTI:
-
Urinary tract infection.
References
Alzheimer’s Society: Counting the Cost. 2009, London. Available at [http://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=787]
Royal College of Psychiatrists: Who Cares Wins. 2005, London. Available at [http://www.rcpsych.ac.uk/PDF/WhoCaresWins.pdf]
Knapp K, Prince M: Dementia UK. 2007, London, Alzheimer’s Society. Available at [http://alzheimers.org.uk/site/scripts/download_info.php?fileID=2]
Sampson EL, Blanchard MR, Jones L, Tookman A, King M: Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry. 2009, 195: 61-66. 10.1192/bjp.bp.108.055335.
Goldberg SE, Whittamore KH, Harwood RH, Bradshaw LE, Gladman JRF, Jones RG: The prevalence of mental health problems among older adults admitted as an emergency to a general hospital. Age Ageing. 2012, 41: 80-86. 10.1093/ageing/afr106.
Siddiqi N, House AO, Holmes JD: Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006, 35: 350-364. 10.1093/ageing/afl005.
Whittamore KH, Goldberg SE, Gladman J, Bradshaw LE, Jones RG, Harwood RH: The diagnosis, prevalence and outcome of delirium in a cohort of older people with mental health problems on general hospital wards. Int J Geriatr Psychiatry. 2013, in press. doi:10.1002/gps.3961
Pinkert C, Holle B: People with dementia in acute hospitals: literature review of prevalence and reasons for hospital admission. Z Gerontol Geriatr. 2012, 45: 728-734. 10.1007/s00391-012-0319-1.
Mukadam N, Sampson EL: A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr. 2011, 23: 344-355. 10.1017/S1041610210001717.
Fick DM, Agostini JV, Inouye SK: Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002, 50: 1723-1732. 10.1046/j.1532-5415.2002.50468.x.
Fong TG, Jones RN, Marcantonio ER, Tommet D, Gross AL, Habtemariam D, Schmitt E, Yap L, Inouye SK: Adverse outcomes after hospitalization and delirium in persons with Alzheimer disease. Ann Intern Med. 2012, 156: 848-856. 10.7326/0003-4819-156-12-201206190-00005.
Saravay SM, Kaplowitz M, Kurek J, Zeman D, Pollack S, Novik S, Saravay SM, Kaplowitz M, Kurek J, Zeman D, Pollack S, Novik S, Knowlton S, Brendel M, Hoffman L: How do delirium and dementia increase length of stay of elderly general medical inpatients?. Psychosomatics. 2004, 45: 235-242. 10.1176/appi.psy.45.3.235.
Tadd W, Hillman A, Calnan M, Calnan S, Read S, Bayer A: From right place–wrong person, to right place—right person: dignified care for older people. J Health Serv Res Policy. 2012, 17 (Suppl 2): 30-36. 10.1258/jhsrp.2011.011118.
Givens JL, Givens JL, Selby K, Goldfeld KS, Mitchell SL: Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc. 2012, 60: 905-909. 10.1111/j.1532-5415.2012.03919.x.
Phelan EA, Givens JL, Selby K, Goldfeld KS, Mitchell SL: Association of incident dementia with hospitalizations. JAMA. 2012, 307: 165-172. 10.1001/jama.2011.1964.
Albert SM, Albert SM, Costa R, Merchant C, Small S, Jenders RA, Stern Y: Hospitalization and Alzheimer’s disease: results from a community-based study. J Gerontol A Biol Sci Med Sci. 1999, 54: M267-M271. 10.1093/gerona/54.5.M267.
Purdy S, Griffin T, Salisbury C, Sharp D: Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Publ Health. 2009, 123: 169-173. 10.1016/j.puhe.2008.11.001.
Formiga F, Ferrer A, Sanz H, Marengoni A, Alburquerque J, Pujol R, Octabaix study members: Patterns of comorbidity and multimorbidity in the oldest old: the Octabaix study. Eur J Intern Med. 2013, 24: 40-44. 10.1016/j.ejim.2012.11.003.
Hawkes N: Alternatives to hospital for older people must be found, says NHS chief. BMJ. 2013, 346: f453-10.1136/bmj.f453.
Gladman JRF, Harwood RH, Jones RJ, Porock D, Griffiths A, Schneider J, Lewis S: Medical and Mental Health/Better Mental Health Development Study Protocol. 2012, Nottingham. Available at [http://nottingham.ac.uk/mcop/documents/papers/issue10-mcop-issn2044-4230.pdf]
Hodkinson HM: Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972, 1: 233-238. 10.1093/ageing/1.4.233.
Shah A, Herbert R, Lewis S, Mahendran R, Platt J, Bhattacharyya B: Screening for depression among acutely ill geriatric inpatients with a short geriatric depression scale. Age Ageing. 1997, 26: 217-221. 10.1093/ageing/26.3.217.
Ewing JA: Detecting alcoholism: the CAGE questionnaire. JAMA. 1984, 252: 1905-1907. 10.1001/jama.1984.03350140051025.
Subbe CP, Kruger M, Gemmel L: Validation of a modified early warning score in medical admissions. Q J Med. 2001, 94: 521-526. 10.1093/qjmed/94.10.521.
Folstein MF, Folstein SE, McHugh PR: Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975, 12: 189-198. 10.1016/0022-3956(75)90026-6.
Trzepacz PT, Mittal D, Torres R, Kanary K, Norton J, Jimerson N: Validation of the delirium rating scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001, 13: 229-242. 10.1176/appi.neuropsych.13.2.229.
Alexopoulos GA, Abrams RC, Young RC, Shamoian CA: Cornell scale for depression in dementia. Biol Psychiatry. 1988, 23: 271-284. 10.1016/0006-3223(88)90038-8.
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J: The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994, 44: 2308-2314. 10.1212/WNL.44.12.2308.
Mahoney FI, Barthel DW: Functional evaluation: the barthel index. Md State Med J. 1965, 14: 56-61.
World Health Organisation: International Classification of Diseases (ICD-10). 2010, Geneva, 10
World Health Organisation: International Classification of Disability, Function and Health (ICF). 2001, Geneva
Chin JJ, Sahadevan S, Tan CY, Ho SC, Choo PW: Critical role of functional decline in delayed discharge from an acute geriatric unit. Ann Acad Med Singapore. 2001, 30: 593-599.
Longman JM, Singer JB, Gao Y, Barclay LM, Passey ME, Pirotta JP, Heathcote KE, Ewald DP, Saberi V, Corben P, Morgan GG: Community based service providers’ perspectives on frequent and/or avoidable admission of older people with chronic disease in rural NSW: a qualitative study. BMC Health Serv Res. 2011, 11: 265-10.1186/1472-6963-11-265.
Procter S, Wilson PM, Brooks F, Kendall S: Success and failure in integrated models of nursing for long term conditions: multiple case studies of whole systems. Int J Nurs Stud. 2012, 50: 632-643.
Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, Parker S, Roland M: Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ. 2007, 334: 31-10.1136/bmj.39020.413310.55.
Walker L, Jamrozik K: Effectiveness of screening for risk of medical emergencies in the elderly. Age Ageing. 2005, 34: 238-242. 10.1093/ageing/afi055.
Pareja T, Pareja T, Hornillos M, Rodríguez M, Martínez J, Madrigal M, Mauleón C, Alvarez B: Medical short stay unit for geriatric patients in the emergency department: clinical and healthcare benefits. Rev Esp Geriatr Gerontol. 2009, 44: 175-179. 10.1016/j.regg.2009.01.007.
Lau L, Chong CP, Lim WK: Hospital treatment in residential care facilities is a viable alternative to hospital admission for selected patients. Geriatr Gerontol Int. 2013, 13: 378-383.
Department of Health: Halfway Home. 2009, London
Huss A, Stuck AE, Rubenstein LZ, Matthias Egger M, Clough-Gorr KM: Multidimensional geriatric assessment: back to the future. Multidimensional preventative home visit programs for community-dwelling older adults: a systematic review and meta analysis of randomised controlled trials. J Gerontol A Biol Sci Med Sci. 2008, 63: 298-307. 10.1093/gerona/63.3.298.
Parker G, Bhakta P, Katbamna S, Lovett C, Paisley S, Parker S, Phelps K, Baker R, Jagger C, Lindesay J, Shepperdson B, Wilson A: Best place of care for older people after acute and during subacute illness: a systematic review. J Health Serv Res Policy. 2000, 5: 176-189.
Evans JG: How are the elderly different?. Improving the Health of Older People: a World View. Edited by: Evans JG, Kane RL, Macfadyen D. 1990, Oxford: OUP, 50-68.
Stuck AE, Siu AL, Wieland D, Adams J, Rubenstein LZ: Comprehensive geriatric assessment: a meta analysis of randomised controlled trials. Lancet. 1993, 342: 1032-1036. 10.1016/0140-6736(93)92884-V.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P: Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011, 343: d6553-10.1136/bmj.d6553.
Tadd W, Calnan S, Calnan M, Bayer T, Read S: Dignity in Practice: An Exploration of the Care of Older Adults in Acute NHS Trusts. 2013, NIHR SDO Programme report. Available at: [http://www.netscc.ac.uk/hsdr/files/project/SDO_ES_08-1819-218_V01.pdf]
George J, Adamson J, Woodford H: Joint geriatric and psychiatric wards: a review of the literature. Age Ageing. 2011, 40: 543-548. 10.1093/ageing/afr080.
Holmes J, Montana C, Powell G, Hewison J, House A, Mason J, Farrin A, McShane P, McParland L, Gilbody , Young J: Liaison Mental Health Services for Older People: A Literature Review, Service Mapping and in-Depth Evaluation of Service Models. NIHR SDO Programme report. Available at [http://www.sdo.nihr.ac.uk/files/project/100-final-report.pdf]
Harwood RH, Porock D, King N, Edwards G, Hammond S, Howe L, Russell C, Howard S, Jones RG, Morrant JD: Development of a Specialist Medical and Mental Health Unit for Older People in an Acute General Hospital. University of Nottingham Medical Crises in Older People discussion paper series. Issue 5, November 2010. ISSN 2044-4230. Available at [http://www.nottingham.ac.uk/mcop/index.aspx]
Harwood RH: Dementia for the hospital physician. Clin Med. 2012, 12: 35-39. 10.7861/clinmedicine.12-1-35.
Goldberg SE, Bradshaw LE, Kearney FC, Russell C, Whittamore KH, Foster PER, Mamza J, Gladman JRF, Jones RG, Lewis SA, Porock D, Harwood RH: Comparison of a specialist Medical and Mental Health Unit with standard care for older people with cognitive impairment admitted to a general hospital: a randomised controlled trial (NIHR TEAM trial). BMJ. 2013, 347: f4132-10.1136/bmj.f4132. doi:10.1136/bmj.f4132
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2318/14/43/prepub
Acknowledgements
This article presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407-10147).
We thank the NIHR Mental Health Research Network, and Trent Dementia Research Network, for support in recruitment. The Medical Crises in Older People study group also included John Gladman, Davina Porock, Sarah Lewis, Rob Jones, Justine Schneider, Simon Conroy, Anthony Avery, Judi Edmans, Adam Gordon, Bella Robbins, Jane Dyas, Pip Logan, Rachel Elliott, Matt Franklin.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conception and design: RH; literature review AG, RH; recruitment and data collection SG, KW, NW, EL, RH; analysis LB, AG, RH, KW; interpretation, drafting of paper RH, AG; all authors contributed to editing and approved the final text.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Glover, A., Bradshaw, L.E., Watson, N. et al. Diagnoses, problems and healthcare interventions amongst older people with an unscheduled hospital admission who have concurrent mental health problems: a prevalence study. BMC Geriatr 14, 43 (2014). https://doi.org/10.1186/1471-2318-14-43
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2318-14-43