Abstract
Objectives
Although the use of specific MRI criteria has significantly increased the diagnostic accuracy of multiple sclerosis (MS), reaching a correct neuroradiological diagnosis remains a challenging task, and therefore the search for new imaging biomarkers is crucial.
This study aims to evaluate the incidence of one of the emerging neuroradiological signs highly suggestive of MS, the central vein sign (CVS), using data from Fabry disease (FD) patients as an index of microvascular disorder that could mimic MS.
Methods
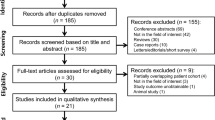
In this retrospective study, after the application of inclusion and exclusion criteria, MRI scans of 36 FD patients and 73 relapsing–remitting (RR) MS patients were evaluated. Among the RRMS participants, 32 subjects with a disease duration inferior to 5 years (early MS) were also analyzed. For all subjects, a Fazekas score (FS) was recorded, excluding patients with FS = 0. Different neuroradiological signs, including CVS, were evaluated on FLAIR T2-weighted and spoiled gradient recalled echo sequences.
Results
Among all the recorded neuroradiological signs, the most striking difference was found for the CVS, with a detectable prevalence of 78.1% (57/73) in RRMS and of 71.4% (25/32) in early MS patients, while this sign was absent in FD (0/36).
Conclusions
Our results confirm the high incidence of CVS in MS, also in the early phases of the disease, while it seems to be absent in conditions with a different etiology. These results corroborate the possible role of CVS as a useful neuroradiological sign highly suggestive of MS.
Key Points
• The search for new imaging biomarkers is crucial to achieve a correct neuroradiological diagnosis of MS.
• The CVS shows an incidence superior to 70% in MS patients, even in the early phases of the disease, while it appears to be absent in FD.
• These findings further corroborate the possible future central role of CVS in distinguishing between MS and its mimickers.



Similar content being viewed by others
Abbreviations
- APS:
-
Antiphospholipid syndrome
- CVS:
-
Central vein sign
- DMT:
-
Disease-modifying therapy
- EDSS:
-
Expanded Disability Status Scale
- ERT:
-
Enzymatic replacement therapy
- FD:
-
Fabry disease
- FLAIR:
-
Fluid attenuated inversion recovery
- MPRAGE:
-
Magnetization prepared rapid gradient echo
- MS:
-
Multiple sclerosis
- RRMS:
-
Relapsing-remitting multiple sclerosis
- SLE:
-
Systemic lupus erythematosus
- SPGR:
-
Spoiled gradient recalled echo
- WM:
-
White matter
- WMLs:
-
White matter lesions
References
Aliaga ES, Barkhof F (2014) MRI mimics of multiple sclerosis. Handb Clin Neurol 122:291–316
Gelfand JM (2014) Multiple sclerosis: diagnosis, differential diagnosis, and clinical presentation. Handb Clin Neurol 122:269–290
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173
Solomon AJ, Naismith RT, Cross AH (2019) Misdiagnosis of multiple sclerosis: Impact of the 2017 McDonald criteria on clinical practice. Neurology 92:26–33
Solomon AJ, Pettigrew R, Naismith RT, Chahin S, Krieger S, Weinshenker B (2021) Challenges in multiple sclerosis diagnosis: misunderstanding and misapplication of the McDonald criteria. Mult Scler 27:250–258
van der Vuurst de Vries RM, Mescheriakova JY, Wong YYM, et al (2018) Application of the 2017 revised McDonald criteria for multiple sclerosis to patients with a typical clinically isolated syndrome. JAMA Neurol 75:1392–1398
Absinta M, Rocca MA, Colombo B et al (2012) Patients with migraine do not have MRI-visible cortical lesions. J Neurol 259:2695–2698
Arrambide G, Tintore M, Auger C et al (2017) Lesion topographies in multiple sclerosis diagnosis: a reappraisal. Neurology 89:2351–2356
Calabrese M, Oh MS, Favaretto A et al (2012) No MRI evidence of cortical lesions in neuromyelitis optica. Neurology 79:1671–1676
Kim SS, Richman DP, Johnson WO, Hald JK, Agius MA (2014) Limited utility of current MRI criteria for distinguishing multiple sclerosis from common mimickers: primary and secondary CNS vasculitis, lupus and Sjogren’s syndrome. Mult Scler 20:57–63
Lapucci C, Saitta L, Bommarito G et al (2019) How much do periventricular lesions assist in distinguishing migraine with aura from CIS? Neurology 92:e1739–e1744
Sinnecker T, Clarke MA, Meier D et al (2019) Evaluation of the central vein sign as a diagnostic imaging biomarker in multiple sclerosis. JAMA Neurol 76:1446–1456
Maggi P, Absinta M, Grammatico M et al (2018) Central vein sign differentiates Multiple Sclerosis from central nervous system inflammatory vasculopathies. Ann Neurol 83:283–294
Charcot JM (1868) Histology of “sclerose en plaque.” Gazette Hosp (Paris) 41:554–566
Ge Y, Law M, Herbert J, Grossman RI (2005) Prominent perivenular spaces in multiple sclerosis as a sign of perivascular inflammation in primary demyelination. AJNR Am J Neuroradiol 26:2316–2319
Tallantyre EC, Brookes MJ, Dixon JE, Morgan PS, Evangelou N, Morris PG (2008) Demonstrating the perivascular distribution of MS lesions in vivo with 7-Tesla MRI. Neurology 70:2076–2078
Clarke MA, Pareto D, Pessini-Ferreira L et al (2020) Value of 3T susceptibility-weighted imaging in the diagnosis of multiple sclerosis. AJNR Am J Neuroradiol 41:1001–1008
Absinta M, Sati P, Schindler M et al (2016) Persistent 7-tesla phase rim predicts poor outcome in new multiple sclerosis patient lesions. J Clin Invest 126:2597–2609
Dal-Bianco A, Grabner G, Kronnerwetter C et al (2017) Slow expansion of multiple sclerosis iron rim lesions: pathology and 7 T magnetic resonance imaging. Acta Neuropathol 133:25–42
Metz I, Gavrilova RH, Weigand SD et al (2021) MRI correlates of multiple sclerosis immunopathological patterns. Ann Neurol. https://doi.org/10.1002/ana.26163
Elliott C, Wolinsky JS, Hauser SL et al (2019) Slowly expanding/evolving lesions as a magnetic resonance imaging marker of chronic active multiple sclerosis lesions. Mult Scler 25:1915–1925
Harrison DM, Li X, Liu H et al (2016) Lesion heterogeneity on high-field susceptibility MRI is associated with multiple sclerosis severity. AJNR Am J Neuroradiol 37:1447–1453
Absinta M, Sati P, Masuzzo F et al (2019) Association of chronic active multiple sclerosis lesions with disability in vivo. JAMA Neurol 76:1474–1483
Elliott C, Belachew S, Wolinsky JS et al (2019) Chronic white matter lesion activity predicts clinical progression in primary progressive multiple sclerosis. Brain 142:2787–2799
Reich DS, Arnold DL, Vermersch P et al (2021) Safety and efficacy of tolebrutinib, an oral brain-penetrant BTK inhibitor, in relapsing multiple sclerosis: a phase 2b, randomised, double-blind, placebo-controlled trial. Lancet Neurol 20:729–738
Germain DP (2010) Fabry disease. Orphanet J Rare Dis 5:30
Cocozza S, Olivo G, Riccio E et al (2017) Corpus callosum involvement: a useful clue for differentiating Fabry disease from multiple sclerosis. Neuroradiology 59:563–570
Ugga L, Cocozza S, Pontillo G et al (2018) Absence of infratentorial lesions in Fabry disease contributes to differential diagnosis with multiple sclerosis. Brain Behav 8:e01121
Böttcher T, Rolfs A, Tanislav C et al (2013) Fabry disease - underestimated in the differential diagnosis of multiple sclerosis? PLoS One 8:e71894
Saip S, Uluduz D, Erkol G (2007) Fabry disease mimicking multiple sclerosis. Clin Neurol Neurosurg 109:361–363
Colomba P, Zizzo C, Alessandro R et al (2018) Fabry disease and multiple sclerosis misdiagnosis: the role of family history and neurological signs. Oncotarget 9:7758–7762
Shribman SE, Shah AR, Werring DJ, Cockerell OC (2015) Fabry disease mimicking multiple sclerosis: lessons from two case reports. Mult Scler Relat Disord 4:170–175
Cennamo G, Di Maio LG, Montorio D et al (2019) Optical coherence tomography angiography findings in Fabry disease. J Clin Med 8(4):528
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Thompson AJ, Baranzini SE, Geurts J, Hemmer B, Ciccarelli O (2018) Multiple sclerosis. Lancet 391:1622–1636
Lublin FD, Reingold SC, Cohen JA et al (2014) Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology 83:278–286
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149:351–356
Fazekas F, Enzinger C, Schmidt R et al (2015) Brain magnetic resonance imaging findings fail to suspect Fabry disease in young patients with an acute cerebrovascular event. Stroke 46:1548–1553
Esposito R, Russo C, Santoro C et al (2020) Association between left atrial deformation and brain involvement in patients with Anderson-Fabry disease at diagnosis. J Clin Med 9(9):2741
Mistry N, Abdel-Fahim R, Samaraweera A et al (2016) Imaging central veins in brain lesions with 3-T T2*-weighted magnetic resonance imaging differentiates multiple sclerosis from microangiopathic brain lesions. Mult Scler 22:1289–1296
Adams CW, Poston RN, Buk SJ, Sidhu YS, Vipond H (1985) Inflammatory vasculitis in multiple sclerosis. J Neurol Sci 69:269–283
Dawson JW (1916) The histology of disseminated sclerosis. Edinb Med J 17:229–241
Gaitán MI, Maggi P, Wohler J et al (2014) Perivenular brain lesions in a primate multiple sclerosis model at 7-tesla magnetic resonance imaging. Mult Scler 20:64–71
Filippi M, Bar-Or A, Piehl F et al (2018) Multiple sclerosis Nat Rev Dis Primers 4:43
Cocozza S, Russo C, Pontillo G, Pisani A, Brunetti A (2018) Neuroimaging in Fabry disease: current knowledge and future directions. Insights Imaging 9:1077–1088
Solomon AJ, Weinshenker BG (2013) Misdiagnosis of multiple sclerosis: frequency, causes, effects, and prevention. Curr Neurol Neurosci Rep 13:403
Hametner S, Wimmer I, Haider L, Pfeifenbring S, Brück W, Lassmann H (2013) Iron and neurodegeneration in the multiple sclerosis brain. Ann Neurol 74:848–861
Sati P, Oh J, Constable RT et al (2016) The central vein sign and its clinical evaluation for the diagnosis of multiple sclerosis: a consensus statement from the North American Imaging in Multiple Sclerosis Cooperative. Nat Rev Neurol 12:714–722
Albrecht J, Dellani PR, Müller MJ et al (2007) Voxel based analyses of diffusion tensor imaging in Fabry disease. J Neurol Neurosurg Psychiatry 78:964–969
Enzinger C, Barkhof F, Ciccarelli O et al (2015) Nonconventional MRI and microstructural cerebral changes in multiple sclerosis. Nat Rev Neurol 11:676–686
Fellgiebel A, Mazanek M, Whybra C et al (2006) Pattern of microstructural brain tissue alterations in Fabry disease: a diffusion-tensor imaging study. J Neurol 253:780–787
Pontillo G, Cocozza S, Lanzillo R et al (2019) Determinants of deep gray matter atrophy in multiple sclerosis: a multimodal MRI study. AJNR Am J Neuroradiol 40:99–106
Schiavi S, Petracca M, Sun P et al (2021) Non-invasive quantification of inflammation, axonal and myelin injury in multiple sclerosis. Brain 144:213–223
Paavilainen T, Lepomäki V, Saunavaara J et al (2013) Diffusion tensor imaging and brain volumetry in Fabry disease patients. Neuroradiology 55:551–558
Sbardella E, Tona F, Petsas N, Pantano P (2013) DTI Measurements in multiple sclerosis: evaluation of brain damage and clinical implications. Mult Scler Int 2013:671730
Dineen RA, Vilisaar J, Hlinka J et al (2009) Disconnection as a mechanism for cognitive dysfunction in multiple sclerosis. Brain 132:239–249
Petracca M, Schiavi S, Battocchio M et al (2020) Streamline density and lesion volume reveal a postero-anterior gradient of corpus callosum damage in multiple sclerosis. Eur J Neurol 27:1076–1082
Roosendaal SD, Geurts JJ, Vrenken H et al (2009) Regional DTI differences in multiple sclerosis patients. Neuroimage 44:1397–1403
Cocozza S, Pontillo G, Quarantelli M et al (2018) Default mode network modifications in Fabry disease: a resting-state fMRI study with structural correlations. Hum Brain Mapp 39:1755–1764
Cocozza S, Schiavi S, Pontillo G et al (2020) Microstructural damage of the cortico-striatal and thalamo-cortical fibers in Fabry disease: a diffusion MRI tractometry study. Neuroradiology 62:1459–1466
Ulivi L, Kanber B, Prados F et al (2020) White matter integrity correlates with cognition and disease severity in Fabry disease. Brain 143:3331–3342
Inglese M, Petracca M (2018) MRI in multiple sclerosis: clinical and research update. Curr Opin Neurol 31:249–255
Wattjes MP, Ciccarelli O, Reich DS et al (2021) 2021 MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol 20:653–670
Calvi A, Haider L, Prados F, Tur C, Chard D, Barkhof F (2020) In vivo imaging of chronic active lesions in multiple sclerosis. Mult Scler 23;1352458520958589
Samaraweera AP, Clarke MA, Whitehead A et al (2017) The central vein sign in multiple sclerosis lesions is present irrespective of the T2* sequence at 3 T. J Neuroimaging 27:114–121
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is S.C.
Conflict of interest
S.C. received speaker fees from Sanofi and Amicus Therapeutics and a Research Grant from FISM (Fondazione Italiana Sclerosi Multipla).
The remaining authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (S.C.) has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tranfa, M., Tortora, M., Pontillo, G. et al. The central vein sign helps in differentiating multiple sclerosis from its mimickers: lessons from Fabry disease. Eur Radiol 32, 3846–3854 (2022). https://doi.org/10.1007/s00330-021-08487-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08487-4