Abstract
Background
Gallstones are known to occur quite frequently after gastrectomy. Most of the studies about postoperative cholelithiasis have focused on open gastrectomy, whereas laparoscopic gastrectomy has recently gained popularity as a type of minimally invasive surgery (MIS). Hence, the efficacy of MIS in preventing post-gastrectomy gallstone formation remains to be elucidated. This study aimed to evaluate the risk of gallstone formation after MIS for clinical stage I/IIA gastric cancer.
Methods
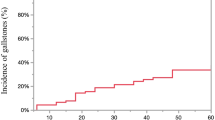
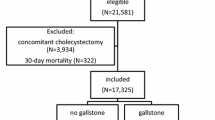
A total of 1166 patients undergoing gastrectomy for clinical stage I/IIA gastric cancer between 2009 and 2016 were included in this study. Gallstones were detected on abdominal ultrasound and/or computed tomography. Multivariate logistic regression analysis was used to determine factors associated with postoperative gallstone formation.
Results
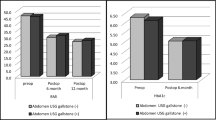
Gallstone formation was observed in 174 patients (15%), of whom 22 (2%) experienced symptomatic cholelithiasis. In multivariate analysis, the following were identified as risk factors for post-gastrectomy gallstone formation: open approach with an odds ratio (OR) of 1.670 and a 95% confidence interval (CI) of 1.110–2.510 (P = 0.014), older age (OR 1.880; 95% CI 1.290–2.730; P < 0.001), high body mass index (OR 1.660; 95% CI 1.140–2.420; P = 0.008), Roux-en-Y (RY) reconstruction (OR 1.770; 95% CI 1.230–2.530; P = 0.002), hepatic branch vagotomy (OR 1.600; 95% CI 1.050–2.440; P = 0.029), and intra-abdominal infectious complications (OR 3.040; 95% CI 1.680–5.490; P < 0.001).
Conclusion
Our study suggested that MIS along with the preservation of the hepatic vagus nerve and non-RY reconstruction could help prevent post-gastrectomy gallstone development.


Similar content being viewed by others
References
Ikeda Y, Shinchi K, Kono S et al (1995) Risk of gallstones following gastrectomy in Japanese men. Surg Today 25:515–518
Chen XJ, Li N, Huang YD et al (2014) Factors for postoperative gallstone occurrence in patients with gastric cancer: a meta-analysis. Asian Pac J Cancer Prev 15:877–881
Chen Y, Li Y (2017) Related factors of postoperative gallstone formation after distal gastrectomy: A meta-analysis. Indian J Cancer 54:43–46
Kim SY, Bang WJ, Lim H, et al. (2019) Increased risk of gallstones after gastrectomy: a longitudinal follow-up study using a national sample cohort in korea. Medicine (Baltimore) 98:e15932.
Lee YW, Kim A, Han M et al (2019) Risk factors for gallbladder stone formation after gastric cancer surgery. J Gastric Cancer 19:417–426
Sakorafas GH, Milingos D, Peros G (2007) Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 years after the introduction of laparoscopic cholecystectomy. Dig Dis Sci 52:1313–1325
Fukagawa T, Katai H, Saka M et al (2009) Gallstone formation after gastric cancer surgery. J Gastrointest Surg 13:886–889
Uyama I, Sakurai Y, Komori Y et al (2005) Laparoscopic gastrectomy with preservation of the vagus nerve accompanied by lymph node dissection for early gastric carcinoma. J Am Coll Surg 200:140–145
Ando S, Tsuji H (2008) Surgical technique of vagus nerve-preserving gastrectomy with D2 lymphadenectomy for gastric cancer. ANZ J Surg 78:172–176
Inokuchi M, Sugita H, Otsuki S et al (2014) Long-term effectiveness of preserved celiac branch of vagal nerve after Roux-en-Y reconstruction in laparoscopy-assisted distal gastrectomy. Dig Surg 31:341–346
Wang CJ, Kong SH, Park JH, et al. (2020) Preservation of hepatic branch of the vagus nerve reduces the risk of gallstone formation after gastrectomy. Gastric Cancer.
Paik KH, Lee JC, Kim HW, et al. (2016) Risk Factors for Gallstone Formation in Resected Gastric Cancer Patients. Medicine (Baltimore) 95:e3157.
Seo GH, Lim CS, Chai YJ (2018) Incidence of gallstones after gastric resection for gastric cancer: a nationwide claims-based study. Ann Surg Treat Res 95:87–93
Inoue K, Fuchigami A, Hosotani R et al (1987) Release of cholecystokinin and gallbladder contraction before and after gastrectomy. Ann Surg 205:27–32
Kobayashi T, Hisanaga M, Kanehiro H et al (2005) Analysis of risk factors for the development of gallstones after gastrectomy. Br J Surg 92:1399–1403
Kodama I, Yoshida C, Kofuji K et al (1996) Gallstones and gallbladder disorder after gastrectomy for gastric cancer. Int Surg 81:36–39
Yi SQ, Ohta T, Tsuchida A et al (2007) Surgical anatomy of innervation of the gallbladder in humans and Suncus murinus with special reference to morphological understanding of gallstone formation after gastrectomy. World J Gastroenterol 13:2066–2071
Yu J, Huang C, Sun Y et al (2019) Effect of laparoscopic vs open distal gastrectomy on 3-Year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA 321:1983–1992
Katai H, Mizusawa J, Katayama H et al (2019) Single-arm confirmatory trial of laparoscopy-assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. Gastric Cancer 22:999–1008
Hyung WJ, Yang HK, Park YK et al (2020) Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol 38:3304–3313
Katai H, Mizusawa J, Katayama H et al (2020) Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol 5:142–151
Brierley JD, Wittekind C (ed) (2017) The TNM classification of malignant tumours, vol 8. Wiley Blackwell, Oxford
Japanese gastric cancer treatment guidelines (2014) ver. 4. Gastric Cancer 20:1–19
Akoglu H (2018) User’s guide to correlation coefficients. Turk J Emerg Med 18:91–93
Krielen P, Stommel MWJ, Pargmae P et al (2020) Adhesion-related readmissions after open and laparoscopic surgery: a retrospective cohort study (SCAR update). Lancet 395:33–41
Li VK, Pulido N, Fajnwaks P et al (2009) Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc 23:1640–1644
Sakuta H, Suzuki T (2005) Plasma total homocysteine and gallstone in middle-aged Japanese men. J Gastroenterol 40:1061–1064
Liu Z, Kemp TJ, Gao YT et al (2018) Association of circulating inflammation proteins and gallstone disease. J Gastroenterol Hepatol 33:1920–1924
Shiffman ML, Sugerman HJ, Kellum JM et al (1992) Changes in gallbladder bile composition following gallstone formation and weight reduction. Gastroenterology 103:214–221
Li X, Gao P (2019) Fatty liver increases gallstone disease risk in younger Chinese patients. Medicine (Baltimore) 98:e15940.
Weng X, Fu F, Ling Y et al (2019) Gallstone disease is an independent predictor for poststroke cognitive impairment in young patients with acute ischemic stroke. Eur Neurol 82:15–22
Emmett DS, Mallat DB (2007) Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc 66:1038–1041
Skinner M, Popa D, Neumann H et al (2014) ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy 46:560–572
Ali MF, Modayil R, Gurram KC et al (2018) Spiral enteroscopy-assisted ERCP in bariatric-length Roux-en-Y anatomy: a large single-center series and review of the literature (with video). Gastrointest Endosc 87:1241–1247
Sawas T, Storm AC, Bazerbachi F et al (2020) An innovative technique using a percutaneously placed guidewire allows for higher success rate for ERCP compared to balloon enteroscopy assistance in Roux-en-Y gastric bypass anatomy. Surg Endosc 34:806–813
Barakos JA, Ralls PW, Lapin SA et al (1987) Cholelithiasis: evaluation with CT. Radiology 162:415–418
Acknowledgements
The authors had no financial support for the research reported.
Funding
The funding sources were not involved in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masanori Terashima has received personal fees from Taiho Pharmaceutical Co. Ltd., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan, Ono Pharmaceutical Co. Ltd., Bristol Myers Squibb Japan, and Yakult Honsha Co. Ltd. Etsuro Bando has received personal fees from the Eizo Corporation, Kanehara-Shuppan, Terumo Corporation, and Eisai. All other authors declare no conflicts of interest.
Informed consent
Informed consent was waived by the ethical committee owing to the retrospective nature of the study.
Human and animal rights
This study was approved by the institutional review board of the Shizuoka Cancer Center (Approval No. J2020-95-2020-1-2).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ikegame, K., Hikage, M., Fujiya, K. et al. The Effect of Minimally Invasive Gastrectomy for Gastric Cancer on Postoperative Gallstone Formation. World J Surg 45, 3378–3385 (2021). https://doi.org/10.1007/s00268-021-06270-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06270-6