Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP) is technically challenging in Roux-en-Y gastric bypass (RYGB). Current approaches either have high failure rate, are resource intensive, or invasive.
Objective
To describe successful adoption of an old technique for performance of ERCP in patients with RYGB anatomy employing enteroscopy with the assistance of a percutaneously placed guidewire, which facilitates both reaching and cannulating the major papilla.
Method
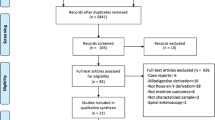
A retrospective cohort study in a tertiary-care center. We included patients with RYGB from 2015 to 2017 who underwent ERCP. We compared success rate and adverse events between rendezvous guidewire-assisted (RGA) and balloon-assisted enteroscopy (BAE) ERCP techniques.
Results
Thirty patients with RYGB underwent 62 ERCPs. The mean age was 62.2 ± 11 years with female predominance 83.3%. The procedures were performed using BAE 43/62 (69.3%), RGA 13/62 (21%), gastrostomy tube 5/62 (8.1%), and colonoscope 1/62 (1.6%). In patients with a native papilla (n = 37 ERCPs), clinical success rate with BAE was 36.8% compared to 100% with RGA (P < 0.001). There was no significant difference in bleeding (P = 0.17), post-ERCP pancreatitis (P = 0.4), or luminal perforation (P = not estimated) between the two techniques in native papilla. The mean procedure time with the RGA was significantly shorter than successful BAE with mean difference: 33 min (95% CI 8–57 min, P = 0.01). Twenty-five ERCPs were performed in eight patients with non-native papilla. BAE success rate in non-native papilla was 95.8%. The mean procedure time of the BAE in non-native papilla was 111 ± 60 min. Native papillae were associated with a significantly higher BAE failure rate compared to non-native papillae (OR: 12; 95% CI 1.44–99.7, P = 0.02).
Conclusion
In patients with RYGB, RGA appears to be highly successful and safe in achieving clinical success for patients with native papilla as compared to BAE.



Similar content being viewed by others
Abbreviations
- AEs:
-
Adverse events
- BAE:
-
Balloon-assisted enteroscopy
- ERCP:
-
Endoscopic Retrograde Cholangiopancreatography
- PEP:
-
Post-ERCP pancreatitis
- RGA:
-
Rendezvous guidewire assisted
- RYGB:
-
Roux-en-Y gastric bypass
References
Johnson EE, Simpson AN, Harvey JB et al (2016) Trends in bariatric surgery, 2002-2012: do changes parallel the obesity trend? Surg Obes Relat Dis 12:398–404
Kindel TL, Lomelin D, McBride C et al (2016) Plateaued national utilization of adolescent bariatric surgery despite increasing prevalence of obesity-associated co-morbidities. Surg Obes Relat Dis 12:868–873
Nguyen NT, Root J, Zainabadi K et al (2005) Accelerated growth of bariatric surgery with the introduction of minimally invasive surgery. Arch Surg 140:1198–1202 discussion 1203
Everhart JE (1993) Contributions of obesity and weight loss to gallstone disease. Ann Intern Med 119:1029–1035
Miller K, Hell E, Lang B et al (2003) Gallstone formation prophylaxis after gastric restrictive procedures for weight loss: a randomized double-blind placebo-controlled trial. Ann Surg 238:697–702
Shiffman ML, Sugerman HJ, Kellum JH et al (1993) Gallstones in patients with morbid obesity. Int J Obes Relat Metab Disord 17:153–158
Tekola B, Wang AY, Ramanath M et al (2011) Percutaneous gastrostomy tube placement to perform transgastrostomy endoscopic retrograde cholangiopancreaticography in patients with Roux-en-Y anatomy. Dig Dis Sci 56:3364–3369
Schreiner MA, Chang L, Gluck M et al (2012) Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc 75:748–756
Abu Dayyeh BK, Thompson CC, Gostout C (2015) Endoscopic retrograde cholangiopancreatography after Roux-en-Y gastric bypass: challenges and cautions. Gastroenterology 148:858–859
Kedia P, Sharaiha RZ, Kumta NA et al (2014) Internal EUS-directed transgastric ERCP (EDGE): game over. Gastroenterology 147:566–568
Shah RJ, Smolkin M, Yen R et al (2013) A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc 77:593–600
Saleem A, Baron TH, Gostout CJ et al (2010) Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy 42:656–660
Committee ASoP, Chandrasekhara V, Khashab MA et al (2017) Adverse events associated with ERCP. Gastrointest Endosc 85:32–47
Gostout CJ, Bender CE (1988) Cholangiopancreatography, sphincterotomy, and common duct stone removal via Roux-en-Y limb enteroscopy. Gastroenterology 95:156–163
Neumann H, Fry LC, Meyer F et al (2009) Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion 80:52–57
Wang AY, Sauer BG, Behm BW et al (2010) Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointest Endosc 71:641–649
Azeem N, Tabibian JH, Baron TH et al (2013) Use of a single-balloon enteroscope compared with variable-stiffness colonoscopes for endoscopic retrograde cholangiography in liver transplant patients with Roux-en-Y biliary anastomosis. Gastrointest Endosc 77:568–577
Inamdar S, Slattery E, Sejpal DV et al (2015) Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc 82:9–19
Abu Dayyeh B (2015) Single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy: getting there. Gastrointest Endosc 82:20–23
Yane K, Katanuma A, Maguchi H et al (2017) Short-type single-balloon enteroscope-assisted ERCP in postsurgical altered anatomy: potential factors affecting procedural failure. Endoscopy 49:69–74
Abbas AM, Strong AT, Diehl DL et al (2018) Multicenter evaluation of the clinical utility of laparoscopy-assisted ERCP in patients with Roux-en-Y gastric bypass. Gastrointest Endosc 87:1031–1039
Attam R, Leslie D, Freeman M et al (2011) EUS-assisted, fluoroscopically guided gastrostomy tube placement in patients with Roux-en-Y gastric bypass: a novel technique for access to the gastric remnant. Gastrointest Endosc 74:677–682
Baron TH, Song LM, Ferreira LE et al (2012) Novel approach to therapeutic ERCP after long-limb Roux-en-Y gastric bypass surgery using transgastric self-expandable metal stents: experimental outcomes and first human case study (with videos). Gastrointest Endosc 75:1258–1263
Kedia P, Kumta NA, Widmer J et al (2015) Endoscopic ultrasound-directed transgastric ERCP (EDGE) for Roux-en-Y anatomy: a novel technique. Endoscopy 47:159–163
Author information
Authors and Affiliations
Contributions
Study design: TS and BKA. Analysis of data: TS and BKA. Interpretation of data: TS and BKA. Writing and review of the manuscript: TS, ACS, JCA, CJF, FB, EJV, VC, MJL, JAM, BTP, MDT, and BKA.
Corresponding author
Ethics declarations
Disclosures
Drs. Tarek Sawas, Andrew C. Storm, Fateh Bazerbachi, Chad J. Fleming, Eric J. Vargas, James C. Andrews, Michael J. Levy, and John A. Martin have no conflicts of interest or financial ties to disclose. Dr. Vinay Chandrasekhara is on the advisory Board Member for Interpace Diagnostics and shareholder of Nevakar Corporation. Dr. Mark D. Topazian has a grant funding from Celgene not relevant to this publication. Dr. Bret T. Petersen is a consultant for Boston scientific and Olympus America, Medical Advisory Board for Advanced Sterilization Products—J and J. Dr Barham K. Abu Dayyeh has research support and consultant for Boston Scientific and Speaker for Olympus and Johnson and Johnson.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sawas, T., Storm, A.C., Bazerbachi, F. et al. An innovative technique using a percutaneously placed guidewire allows for higher success rate for ERCP compared to balloon enteroscopy assistance in Roux-en-Y gastric bypass anatomy. Surg Endosc 34, 806–813 (2020). https://doi.org/10.1007/s00464-019-06832-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06832-9