Abstract
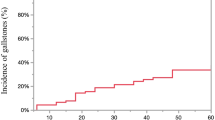
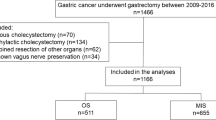
Sleeve gastrectomy (SG) is a widely accepted procedure that has gained popularity among both bariatric surgeons and patients. There is still limited data in the literature on the formation of gallstones following laparoscopic sleeve gastrectomy, and so the present study determines the incidence of and potential risk factors related to the development of gallstones following laparoscopic sleeve gastrectomy. The data of patients who underwent laparoscopic sleeve gastrectomy at a single center due to morbid obesity between January 2014 and December 2017 was retrospectively reviewed and analyzed. The patients were divided into two groups, as those with gallstones detected on ultrasound at 12 months and those without gallstones. Data of the two groups was compared. BMI did not differ significantly between patients with positive (+) and negative (−) ultrasound findings (p > 0.05). Aside from age, hypertension, and coronary artery disease, other preoperative parameters showed no significant association with the development of gallstones in USG (−) and USG (+) patients. The present study identified no significant relationship between a decrease in BMI following LSG and the postoperative development of gallstones. Preoperative hypertension and coronary artery disease were found to be significantly related to the development of gallstones after surgery. The authors suggest that patients with preexisting CAD and hypertension in the preoperative period must be followed-up with ultrasound more meticulously.

Similar content being viewed by others
References
Almogy G, Crookes PF, Anthone GJ. Longitudinal gastrectomy as a treatment for the high-risk super-obese patient. Obes Surg. 2004;14:492–7. https://doi.org/10.1381/096089204323013479.
Raziel A, Sakran N, Szold A, et al. Concomitant cholecystectomy during laparoscopic sleeve gastrectomy. Surg Endosc. 2015; https://doi.org/10.1007/s00464-014-4010-z.
Gunkova P, Gunka I, Zonca P, et al. Laparoscopic sleeve gastrectomy for morbid obesity with natural orifice specimen extraction (NOSE). Bratisl Med J. 2015;116(7):422–5.
Li VK, Pulido N, Fajnwaks P, et al. Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 2009;23:1640–4. https://doi.org/10.1007/s00464-008-0204-6.
Quesada BM, Kohan G, Roff HE, et al. Management of gallstones and gallbladder disease in patients undergoing gastric bypass. World J Gastroenterol. 2010;16:2075–9.
Villegas L, Schneider B, Provost D, et al. Is routine cholecystectomy required during laparoscopic gastric bypass? Obes Surg. 2004;14:206–11.
Dhabuwala A, Cannan RJ, Stubbs RS. Improvement in comorbidities following weight loss from gastric bypass surgery. Obes Surg. 2000;10:428–35.
Shiffman ML, Sugerman HJ, Kellum JM, et al. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 1991;86(8):1000–5.
Portenier DD, Grant JP, Blackwood HS, et al. Expectant management of the asymptomatic gallbladder at Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3(4):476–9.
Amaral JF, Thompson WR. Gall bladder disease in the morbidly obese. Am J Surg. 1985;149:551–7.
Festi D, Dormi A, Capodicasa S, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008;14(34):5282–9.
Attili AF, Carulli N, Roda E, et al. Epidemiology of gallstone disease in Italy: prevalence data of the multicenter Italian study on cholelithiasis (M.I.COL.). Am J Epidemiol. 1995;141(2):158–65.
LJJr W, Wright JK, Debelak JP, et al. Prevention of gallstone formation in morbidly obese patients under going rapid weight loss: results of randomized controlled pilot study. J Surg Res. 2002;102(1):50–6.
Hasan MY, Lomanto D, Loh LL, et al. Gallstone disease after laparoscopic sleeve gastrectomy in an Asian population—what proportion of gallstones actually becomes symptomatic? Obes Surg. 2017;27:2419–23. https://doi.org/10.1007/s11695-017-2657-y.
Kiewiet RM, Durian MF, van Leersum M, et al. Gallstone formation after weight loss following gastric banding in morbidly obese Dutch patients. Obes Surg. 2006;16(5):592–6.
Sioka E, Zacharoulis D, Zachari E, Papamargaritis D, Pinaka O, Katsogridaki G, Tzovaras G Complicated gallstones after laparoscopic sleeve gastrectomy. J Obes, 2014. 468203
Adams LB, Chang C, Pope J, et al. Randomized, prospective comparison of ursodeoxycholic acid for the prevention of gallstones after sleeve gastrectomy. Obes Surg. 2016;26(5):990–4.
D’Hondt M, Sergeant G, Deylgat B, et al. Prophylactic cholecystectomy, a mandatory step in morbidly obese patients undergoing laparoscopic Roux-en-Y gastric bypass? J Gastrointest Surg. 2011;15:1532–6.
Moon RC, Teixeira AF, DuCoin C, et al. Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Surg Obes Relat Dis. 2014;10(1):64–8.
Aridi HD, Sultanem S, Abtar H, et al. Management of gallbladder disease after sleeve gastrectomy in a selected Lebanese population. Surg Obes Relat Dis. 2016;12:1300–4.
Nagem R, Lazaro-da-Silva A. Cholecystolithiasis after gastric bypass: a clinical, biochemical, and ultrasonographic 3-year follow-up study. ObesSurg. 2012;22:1594–9.
Méndez-Sánchez N, Bahena-Aponte J, Chávez-Tapia NC, et al. Strong association between gallstones and cardiovascular disease. Am J Gastroenterol. 2005;100(4):827–30.
Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Obesity (Silver Spring). 2009;17(1):1–70.
Tarantino I, Warschkow R, Steffen T, et al. Is routine cholecystectomy justified in severely obese patients undergoing a laparoscopic Roux-en-Y gastric bypass procedure? A comparative cohort study. Obes Surg. 2011;21:1870–8.
Author information
Authors and Affiliations
Contributions
All of the authors participated in the design, execution, and analysis of the paper and approved the final version.
Corresponding author
Ethics declarations
Board of ethics approval for this study was obtained from the ethics commission of Adiyaman University. Approval no. 2019/2-10. Approval date 20.03.2019. This study is retrospective and therefore no consent form is needed.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Özdaş, S., Bozkurt, H. Factors Affecting the Development of Gallstones Following Laparoscopic Sleeve Gastrectomy. OBES SURG 29, 3174–3178 (2019). https://doi.org/10.1007/s11695-019-03946-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03946-w