Abstract
Purpose
The main challenges in revision total hip arthroplasty (rTHA) are the treatment of the bone loss and the pre-operative planning. 3D-printed models may enhance pre-operative planning. The aim of the study is to compare the intra- and peri-operative results and costs for Paprosky type 3 rTHAs planned with 3D-printed models to ones accomplished with the conventional imaging techniques (X-rays and CT scan).
Methods
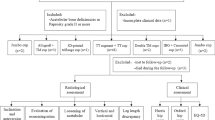
Seventy-two patients with Paprosky type 3 defect underwent rTHA between 2014 and 2021. Fifty-two patients were treated with standard planning and 20 were planned on 3D-printed models. Surgical time, intra-operative blood loss, number of transfused blood units, number of post-operative days of hospitalization, and use of acetabular rings were compared between the two groups. A costs comparison was also performed.
Results
The 3D-printed group showed reduced operative time (101.8 min (SD 27.7) vs. 146.1 min (SD 49.5), p < 0.001) and total days of hospitalization (9.3 days (SD 3.01) vs. 12.3 days (SD 6.01), p = 0.009). The cost of the procedures was significantly lower than the control group, with an adjusted difference of 4183 euros (p = 0.004). No significant differences were found for the number of total transfused blood units and blood loss and the number of acetabular rings.
Conclusion
The use of 3D-printed models led to a meaningful cost saving. The 3D-printed pre-operative planning for complex rTHAs seems to be effective in reducing operating time, hospital stay and overall costs.




Similar content being viewed by others
Data Availability
We confirm the data is available for interested people.
References
Bozic KJ, Kurtz SM, Lau E et al (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg 91:128–133. https://doi.org/10.2106/JBJS.H.00155
Ulrich SD, Seyler TM, Bennett D et al (2008) Total hip arthroplasties: what are the reason for revision? Int Orthop 32:597–604. https://doi.org/10.1007/s00264-007-0364-3
Hooper G, Lee AJ, Rothwell A et al (2014) Current trends and projections in the utilisation rates of hip and knee replacement in New Zealand from 2001 to 2026. N Z Med J 127:82–93
Pabinger C, Lothaller H, Portner N, Geissler A (2018) Projections of hip arthroplasty in OECD countries up to 2050. Hip Int 28(5):498–506. https://doi.org/10.1177/1120700018757940
Kummerant J, Wirries N, Derksen A et al (2020) The etiology of revision total hip arthroplasty: current trends in a retrospective survey of 3450 cases. Arch Orthop Trauma Surg 140:1265–1273. https://doi.org/10.1007/s00402-020-03514-3
Barrack RL (2004) Preoperative planning for revision total hip arthroplasty. Clin Orthop Related Res 420:32–38. https://doi.org/10.1097/00003086-200403000-00006
Mancino F, Cacciola G, Di Matteo V et al (2020) Reconstruction options and outcomes for acetabular bone loss in revision hip arthroplasty. Orthop Rev 12(Suppl 1):8655. https://doi.org/10.4081/0r.2020.8655
Froschen FS, Randau TM, Gravius N et al (2022) Risk factors for implant failure of custom-made acetabular implants in patients with Paprosky III acetabular bone loss and combined pelvic discontinuity. Technol Health Care 30:703–711. https://doi.org/10.3233/THC-202236
Friedrich MJ, Schmolders J, Michel RD et al (2014) Management of severe periacetabular bone loss combined with pelvic discontinuity in revision hip arthroplasty. Int Orthop 38:2455–2461. https://doi.org/10.1007/s00264-014-2443-6
Meynen A, Vles G, Zadpoor AA et al (2021) The morphological variation of acetabular defects in revision total hip arthroplasty-a statistical shape modeling approach. J Orthop Res. https://doi.org/10.1002/jor.24995
Fryhofer GW, Ramesh S, Sheth NP (2020) Acetabular reconstruction in revision total hip arthroplasty. J Clin Orthop 11:22–28. https://doi.org/10.1016/j.jcot.2019.11.004
Zhang JW, Liu XL, Zeng YM et al (2021) Comparison of 3D printing rapid prototyping technology with traditional radiographs in evaluating acetabular defects in revision hip arthroplasty: a prospective and consecutive study. Orthop Surg 13:1773–1780. https://doi.org/10.1111/os.13108
Aprato A, Olivero M, Di Benedetto P, Massè A (2020) Decision/therapeutic algorithm for acetabular revisions. Acta Biomed 91(14-S):e2020025. https://doi.org/10.23750/abm.v91i14-S.10999
Perka C, Ascherl R (2022) Pitfalls in revision hip arthroplasty. Orthopadie. https://doi.org/10.1007/s00132-022-04282-1
Kavalerskiy GM, Murylev VY, Rukin YA et al (2018) Three-dimensional models in planning of revision hip arthroplasty with complex acetabular defects. Indian J Orthop 52:625–630. https://doi.org/10.4103/ortho.IJOrtho_556_16
Hughes AJ, DeBuitleir C, Soden P et al (2017) 3D printing aids acetabular reconstruction in complex revision hip arthroplasty. Adv Orthop 2017. https://doi.org/10.1155/2017/8925050
Alemayehu DG, Zhang Z, Tahir E et al (2021) Preoperative planning using 3D printing technology in orthopedic surgery. Biomed Res Int 2021:7940242. https://doi.org/10.1155/2021/7940242
Hasan O, Atif M, Jessar MM, Hashmi P (2019) Application of 3D printing in orthopaedic surgery. A new affordable horizon for cost-conscious care. J Pak Med Assoc 69(Suppl1):S46–S50
Kumar P, Vatsya P, Rajnish RK et al (2020) Application of 3d printing in hip and knee arthroplasty: a narrative review. Indian J Orthop 55(Suppl 1):14–26. https://doi.org/10.1007/s43465-020-00263-8
Bagaria V, Bhansali R, Pawar P (2018) 3D printing- creating a blueprint for the future of orthopedics: current concept review and the road ahead! J Clin Orthop Trauma 9:207–212. https://doi.org/10.1016/j.jcot.2018.07.007
Wong KC (2016) 3D-printed patient-specific applications in orthopedics. Orthop Res Rev 8:57–66. https://doi.org/10.2147/ORR.S99614
Telleria JJM, Gee AO (2013) Classification in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res 471:3725–3730. https://doi.org/10.1007/s11999-013-3264-4
Ballard DH, Mills P, Duszak R Jr et al (2019) Medical 3D printing cost-savings in orthopedic and maxillofacial surgery: cost analysis of operating room time saved with 3D printed anatomic models and surgical guides. Acad Radiol 27:1103–1113. https://doi.org/10.1016/j.acra.2019.08.011
Aprato A, Joeris A, Tosto F et al (2016) Direct and indirect costs of surgically treated pelvic fractures. Arch Orthop Trauma Surg 136:325–330. https://doi.org/10.1007/s00402-015-2373-9
Aprato A, Ghia C, Tosto F et al (2019) How much does saving femoral head cost after acetabular fracture? Comparison between ORIF and THA. Acta Orthop Belg 85(4):502–509
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34(28):3661–3679. https://doi.org/10.1002/sim.6607
Woo SH, Sung MJ, Park KS, Yoon TR (2020) Three-dimensional-printing Technology in Hip and Pelvic Surgery: Current Landscape. Hip Pelvis 32(1):1–10. https://doi.org/10.5371/hp.2020.32.1.1
Aprato A, Olivero M, Iannizzi G et al (2020) Pelvic discontinuity in acetabular revisions: does CT scan overestimate it? A comparative study of diagnostic accuracy of 3D-modeling and traditional 3D CT scan. Musculoskelet Surg 104(171):177. https://doi.org/10.1007/s12306-019-00608-z
Yang L, Grottkau B, He Z, Ye C (2017) Three dimensional printing technology and materials for treatment of elbow fractures. Int Orthop 41:2381–2387. https://doi.org/10.1007/s00264-017-3627-7
Ozturk AM, Suer O, Derin O et al (2020) Surgical advantages of using 3D patient-specific models in high-energy tibial plateau fractures. Eur J Trauma Emerg Surg 46:1183–1194. https://doi.org/10.1007/s00068-020-01378-1
Garbarino LJ, Gold PA, Sodhi N et al (2019) The effect of operative time on in-hospital length of stay in revision total knee arthroplasty. Ann Transl Med 7:66. https://doi.org/10.21037/atm.2019.01.54
Tack P, Victor J, Gemmel P, Annemans L (2021) Do custom 3D-printed revision acetabular implants provide enough value to justify the additional costs? The health-economic comparison of a new porous 3D-printed hip implant for revision arthroplasty of Paprosky type 3B acetabular defects and its closest alternative. Orthop Traumatol Surg Res 107(1):102600.https://doi.org/10.1016/j.otsr.2020.03.012
Carling MS, Jeppsson A, Eriksson BI, Brisby H (2015) Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res 10:48. https://doi.org/10.1186/s13018-015-0188-6
Loppini M, Cannata R, Pisano A et al (2021) Incidence and predictors of blood transfusions in one stage bilateral total hip arthroplasty: a single center prospective cohort study. Arch Orthop Trauma Surg 142:3549–3554. https://doi.org/10.1007/s00402-021-04255-7
Sizer SC, Cherian JJ, Elmallah RD et al (2015) Predicting blood loss in total knee and hip arthroplasty. Orthop Clin North Am 46:445–459. https://doi.org/10.1016/j.ocl.2015.06.002
Assink N, Reininga IHF, Ten Duis K et al (2022) Does 3D assisted surgery of tibial plateau fractures improve surgical and patient outcome? A systematic review of 1074 patients. Eur J Trauma Emerg Surg 48:1737–1749. https://doi.org/10.1007/s00068-021-01773-2
Fadero PE, Shah M (2014) Three dimensional (3D) modelling and surgical planning in trauma and orthopaedics. Surgeon 12:328–333. https://doi.org/10.1016/j.surge.2014.03.008
Author information
Authors and Affiliations
Contributions
All authors have equally contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is divided into a retrospective part and a prospective one. The authors certify that the study was performed in accordance with ethical standards of Declaration of Helsinki. The study was approved by local Ethics Committee of the University.
Consent for publication
Verbal informed consent was obtained from all individual participants regarding publishing their data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giachino, M., Aprato, A., Limone, B. et al. Impact of three-dimensional printed planning in Paprosky III acetabular defects: a case–control and cost-comparison analysis. International Orthopaedics (SICOT) 47, 1465–1472 (2023). https://doi.org/10.1007/s00264-023-05763-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05763-4