Abstract
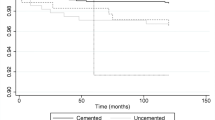
Primary total hip arthroplasties have reported success rates of greater than 95% in many series with a longer than 10-year follow-up. Revision total hip arthroplasty due to such factors as increased high-activity levels, younger patients undergoing the procedure and increasing life expectancy has become more prevalent. An understanding of the mechanisms and timing of total hip arthroplasty failure can direct efforts aimed at reducing revision rates. This study was conducted to evaluate the indications for revision hip arthroplasty and relate these to the time after the index primary hip arthroplasty. A review of all revision hip arthroplasties at two centres over a 6-year time period identified 225 patients who underwent 237 revisions. The overall mean time to revision was 83 months (range: 0–360 months). The cause of failure was aseptic loosening in 123 hips (51.9%), instability in 40 hips (16.9%) and infection in 37 hips (5.5%). When stratified into two groups (less than 5 years, more than 5 years after the index primary hip arthroplasty), 118 of 237 (50%) revisions occurred in less than 5 years, with 33% due to instability and 24% resulting from infection. The majority of the causes of failure within 5 years in these early revisions were instability and deep infection. The success of hip arthroplasty is likely to be compromized if technical aspects of the surgery for appropriate component positioning and critical protocols to minimise complications such as infection are not given the proper attention.
Résumé
A dix ans de recul moyen les prothèses totales de hanches ont un taux de 95% de réussite dans la plupart des séries. Les facteurs ayant entraînés une réintervention, de type révision dépendent du niveau d’activité des sujets, de leurs jeunes âges, et de l’augmentation de la durée de vie. La compréhension des mécanismes d’échecs des prothèses totales de hanche devrait permettre de réduire le taux de révision. Cette étude a pour but d’évaluer les indications de révisions des prothèses totales de hanche. Pour cela, ont été revus, dans deux centres, avec six ans de recul moyen 225 patients qui ont bénéficié de 237 révisions. Le temps moyen pour la révision a été de 83 mois (0 à 360 mois). La cause de l’échec a été le descellement aseptique 123 hanches (51.9%), instabilité sur 40 hanches (16.9%) et infection sur 37 hanches (5.5%). Si l’on reclasse ces patients en deux groupes à moins et plus de 5 ans, 118 des 237 révisions (50%) surviennent dans une période de moins de 5 ans, 33% sont dues à l’instabilité, 24% à l’infection. Les causes d’échecs majeures avant 5 ans avec révisions, sont donc l’instabilité de la hanche et les infections profondes. Le succès d’une arthroplastie totale de hanche passe donc par le bon positionnement des implants et le respect du protocole de façon à éviter les complications infectieuses.




Similar content being viewed by others
References
Mahomed NN, Barrett JA, Katz JN et al (2003) Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Jnt Surg Am 85-A(1):27–32
Eisler T, Svensson O, Tengstrom A et al (2002) Patient expectation and satisfaction in revision total hip arthroplasty. J Arthroplasty 17(4):457–462
Wroblewski BM (1984) Current trends in revision of total hip arthroplasty. Int Orthop 8(2):89–93
Furnes O, Lie SA, Espehaug B et al (2001) Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Jnt Surg Br 83(4):579–586
Older J (2002) Charnley low-friction arthroplasty: a worldwide retrospective review at 15 to 20 years. J Arthroplasty 17(6):675–680
Kuster MS (2002) Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med 32(7):433–445
Seyler TM, Mont MA, Ragland PS et al (2006) Sports activity after total hip and knee arthroplasty: specific recommendations concerning tennis. Sports Med 36(7):571–583
Mont MA, LaPorte DM, Mullick T et al (1999) Tennis after total hip arthroplasty. Am J Sports Med 27(1):60–64
Meek RM, Allan DB, McPhillips G et al (2006) Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res 447:9–18
Berry DJ, Harmsen WS, Cabanela ME et al (2002) Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Jnt Surg Am 84-A(2):171–177
Ong A, Wong KL, Lai M et al (2002) Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Jnt Surg Am 84-A(5):786–792
Sarvilinna R, Huhtala HS, Puolakka TJ et al (2003) Periprosthetic fractures in total hip arthroplasty: an epidemiologic study. Int Orthop 27(6):359–361
Bohm P, Bischel O (2001) Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Jnt Surg Am 83-A(7):1023–1031
Vichinsky EP, Neumayr LD, Haberkern C et al (1999) The perioperative complication rate of orthopedic surgery in sickle cell disease: report of the National Sickle Cell Surgery Study Group. Am J Hematol 62(3):129–138
Kobayashi S, Saito N, Horiuchi H et al (2000) Poor bone quality or hip structure as risk factors affecting survival of total-hip arthroplasty. Lancet 355(9214):1499–1504
Phillips CB, Barrett JA, Losina E et al (2003) Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Jnt Surg Am 85-A(1):20–26
Alberton GM, High WA, Morrey BF (2002) Dislocation after revision total hip arthroplasty : an analysis of risk factors and treatment options. J Bone Jnt Surg Am 84-A(10):1788–1792
Parvizi J, Wade FA, Rapuri V et al (2006) Revision hip arthroplasty for late instability secondary to polyethylene wear. Clin Orthop Relat Res 447:66–69
Ibrahim T, Hobson S, Beiri A et al (2005) No influence of body mass index on early outcome following total hip arthroplasty. Int Orthop 29(6):359–361
Malik MH, Gray J, Kay PR (2004) Early aseptic loosening of cemented total hip arthroplasty: the influence of non-steroidal anti-inflammatory drugs and smoking. Int Orthop 28(4):211–213
McLaughlin JR, Lee KR (2006) The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Jnt Surg Br 88(10):1286–1292
Espehaug B, Havelin LI, Engesaeter LB et al (1997) Patient-related risk factors for early revision of total hip replacements. A population register-based case-control study of 674 revised hips. Acta Orthop Scand 68(3):207–215
Meldrum RD, Wurtz LD, Feinberg JR et al (2005) Does smoking affect implant survivorship in total hip arthroplasty? A preliminary retrospective case series. Iowa Orthop J 25:17–24
Persson PE, Nilsson OS, Berggren AM (2005) Do non-steroidal anti-inflammatory drugs cause endoprosthetic loosening? A 10-year follow-up of a randomized trial on ibuprofen for prevention of heterotopic ossification after hip arthroplasty. Acta Orthop 76(6):735–740
Crawford SA, Siney PD, Wroblewski BM (2000) Revision of failed total hip arthroplasty with a proximal femoral modular cemented stem. J Bone Jnt Surg Br 82(5):684–688
Templeton JE, Callaghan JJ, Goetz DD et al (2001) Revision of a cemented acetabular component to a cementless acetabular component. A ten to fourteen-year follow-up study. J Bone Jnt Surg Am 83-A(11):1706–1711
Lind M, Krarup N, Mikkelsen S et al (2002) Exchange impaction allografting for femoral revision hip arthroplasty: results in 87 cases after 3.6 years’ follow-up. J Arthroplasty 17(2):158–164
Weeden SH, Paprosky WG (2002) Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty 17[4 Suppl 1]:134–137
Ullmark G, Hallin G, Nilsson O (2002) Impacted corticocancellous allografts and cement for revision of the femur component in total hip arthroplasty. J Arthroplasty 17(2):140–149
Lachiewicz PF, Soileau ES (2005) Changing indications for revision total hip arthroplasty. J Surg Orthop Adv 14(2):82–84
Khatod M, Barber T, Paxton E et al (2006) An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res 447:19–23
Clohisy JC, Calvert G, Tull F et al (2004) Reasons for revision hip surgery: a retrospective review. Clin Orthop Relat Res (429):188–192
Sharkey PF, Hozack WJ, Rothman RH et al (2002) Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res (404):7–13
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ulrich, S.D., Seyler, T.M., Bennett, D. et al. Total hip arthroplasties: What are the reasons for revision?. International Orthopaedics (SICO 32, 597–604 (2008). https://doi.org/10.1007/s00264-007-0364-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-007-0364-3