Abstract
Purpose
This review discusses the current state of prostate-specific membrane antigen (PSMA)-based alpha therapy of metastatic castration-resistant prostate cancer (mCRPC). With this in-depth discussion on the growing field of PSMA-based alpha therapy (PAT), we aimed to increase the interactions between basic scientists and physician–scientists in order to advance the field.
Methods
To achieve this, we discuss the potential, current status, and opportunities for alpha therapy and strategies, attempted to date, and important questions that need to be addressed. The paper reviews important concepts, including whom to treat, how to treat, what to expect regarding treatment outcome, and toxicity, and areas requiring further investigations.
Results
There is much excitement about the potential of this field. Much of the potential exists because these therapies utilize unique mechanisms of action, difficult to achieve with other conventional therapies.
Conclusion
A better understanding of the strengths and limitations of PAT may help in creating an effective therapy for mCRPC and design a rational combinatorial approach to treatment by targeting different tumor pathways.
Similar content being viewed by others
Introduction
Prostate cancer is a biologically and clinically heterogeneous disease that is a leading cause of cancer death among men globally. Treatment for early-stage prostate cancer is radical prostatectomy or external beam radiotherapy. Prostate-specific antigen (PSA) levels rapidly fall to an undetectable level after treatment and can then be used as a tumor marker for disease surveillance [1]. More than half of these patients treated with curative radical prostatectomy or external beam radiotherapy will eventually have disease recurrence within a few years. Androgen blockade is a therapeutic option available in the treatment of recurrent prostate cancer. This is done to starve the prostate cancer cells of androgen, which it requires for growth. Effective androgen blockade halts disease progression but only temporarily as most patients become castration-resistant within a few years [2].
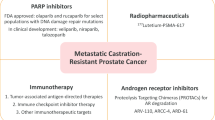
Therapy agents acting on different pathways, including taxane-based chemotherapy, next-generation anti-androgen, and radionuclide therapy with radium dichloride, have been found to prolong survival when applied in the treatment of mCRPC [2,3,4]. Despite the widespread utilization of these agents, mCRPC has remained a highly fatal disease. This, therefore, calls for continued effort in developing novel therapies to improve mCRPC-related mortality and morbidity. Prostate-specific membrane antigen (PSMA) is a membrane-expressed glycoprotein that is overexpressed on prostate cancer cells. The level of PSMA expression by prostate cancer cells is accentuated in metastatic and castration-resistant stages of the disease. This property of PSMA makes it an attractive target for imaging and therapy of the lethal forms of prostate cancer, metastatic, castration-resistant stage of the disease. PSMA-based radioligand therapy (PRLT) of mCRPC has been more commonly done using lutetium-177 (177Lu), a beta emitter complexed to PSMA ligand. The safety and efficacy of 177Lu-PSMA RLT for mCRPC treatment have been widely reported by many groups worldwide [5,6,7]. Most recently, the Thera-P trial, which is the first randomized phase 2 study of 177Lu-PSMA-617 compared with cabazitaxel in men with mCRPC, provides evidence that 177Lu-PSMA-617 is a potential alternative to cabazitaxel in men with mCRPC [8]. The trial results showed a greater PSA response rate and fewer toxicities in the 177Lu-PSMA-617 arm than the cabazitaxel arm [8].
Despite this remarkable response of mCRPC to 177Lu-PSMA-617, a significant proportion of patients may not respond to treatment [5,6,7]. Most patients who demonstrate a response to 177Lu-PSMA-617 initially may also experience disease progression. This has, therefore, led to an interest in the evaluation of the safety and efficacy of PSMA-based alpha therapy (PAT) as a therapeutic alternative for mCRPC patients who may be unsuitable for or resistant to 177Lu-PSMA-617.
Prostate-specific membrane antigen (PSMA)
The evolution of knowledge on the biology of PSMA and its translation to therapy began with the development of the prostate cancer cell line LNCaP by Horoszewicz et al. in 1983 [9]. To date, several PSMA ligands have been developed for imaging and therapy of prostate cancer. The detailed discussion on these ligands is beyond the scope of this paper but has been recently presented by O’Keefe and colleagues [10]. PSMA, a type II 750-amino acid transmembrane protein (100–120 kDa), functions as a folate hydrolase I or glutamate carboxypeptidase II enzyme in the epithelial cells of the prostate gland [11,12,13]. Low-level diffuse physiologic PSMA expression occurs in the normal human prostate tissue, which is mainly localized to the cytoplasm and the apical side of the epithelial lining of the prostatic ducts but not basal epithelium, neuroendocrine, or stromal cells [14]. In dysplastic or frankly neoplastic prostate tissue, PSMA expression transfers from the apical membrane to the luminal surface of the ducts [15]. The main attraction for the use of PSMA for targeted therapy is its high level of expression that is increased by about 100- to 1000-folds higher in prostate cancer tissue compared with normal prostate tissue and the direct correlation between its level of expression and androgen independence, metastasis, and disease progression [16, 17]. As against what the name would suggest, PSMA expression is not specific for prostate cancer as it is overexpressed in the neovasculature of solid tumors but not in normal tissue vasculature. PSMA expression also occurs in several normal tissues, including the enterocytes of the small bowel, ductal cells of the proximal convoluted renal tubules, and salivary glands [18]. Following binding by PSMA radioligand, membrane-expressed PSMA undergoes clathrin-based internalization and, as such, can serve not only as an imaging biomarker but also as a target for radioligand therapy [6]. These characteristics make PSMA an appealing molecular target for theranostics of mCRPC [19].
Alpha-emitting radionuclides for PSMA therapy
Alpha-emitting radionuclides have shown promising results as radiotherapeutic agents for the treatment of mCRPC. A detailed discussion on alpha emitters for radionuclide cancer therapy is discussed in detail in another article in this issue. Alpha particles for endo-radionuclide therapy have two distinct advantages over conventional therapies. Alpha particles are highly energetic and have a short-range in tissue (< 0.1 mm) corresponding to a few cell diameter. This combination ensures the deposition of a large amount of energy within a short radius leading to the effective killing of the targeted tumor with sparing of contiguous normal tissues. Also, the high linear energy transfer of alpha particles causes direct double-stranded deoxyribonucleic acid (DNA) damage and DNA cluster breaks that occur independent of the cell cycle phase or tissue oxygenation, which are also difficult to repair [20, 21]. Because of these attributes of alpha particles, therapy with alpha-emitting radionuclides has the potential to overcome resistance to PRLT with beta-emitting radionuclide or treatment with chemotherapeutic drugs [22, 23]. Despite the multitude of available alpha-emitting radionuclides, only a few of them have desirable characteristics that make them suitable for clinical application in targeted alpha therapy [24].
When applied in the treatment of mCRPC, the desired alpha-emitting radionuclide should target the entire spectrum of metastases, micrometastases, and overt metastatic disease in lymph nodes, the skeleton, and visceral organs. Accordingly, a couple of alpha-emitting radionuclides, including 225Ac, 213Bi, 149 Tb, 212Pb/212Bi, 211At, 223Ra, and 227Th, have been complexed to PSMA inhibitors and evaluated in preclinical and clinical studies for their efficacy and safety in the treatment of mCRPC (Table 1) [25]. Of the limited alpha-emitting radionuclides that are suitable for clinical application, 225Ac (physical half-life, T1/2 = 9.9d) and its short-lived daughter radionuclide, 213Bi (T1/2 = 46 min), have been most extensively studied [26] and will be discussed in detail. While the clinical translation of the preclinical work of the rest of the alpha-emitting PSMA targeting inhibitors appears promising based on the demonstrated antitumor activity, there are still some challenges associated with their use, as briefly highlighted below.
149 Tb is a rare-earth element with a physical half-life of 4.1 h. It decays by emitting different particle, and non-particle radiations include α particles (3.97 MeV, 16.7%), electron capture (76.2%), positron emission (7.1%), gamma rays (165 keV, 26.4%), and X-rays. Therefore, it can be used for targeted alpha therapy (TAT), single-photon emission tomography (SPECT) imaging, and positron emission tomography (PET) imaging [25, 27]. The most striking limitation to the clinical application of this highly promising radionuclide relates to its limited available supply. The production and chemical separation of 149 Tb is fraught with many difficulties, a setback that may limit its clinical translation [28]. Long-lived daughter radionuclides in the decay scheme of 149 Tb complicate dosimetry and may contribute to radiation dose to patients. Alpha particle emission from 149 Tb is associated with high recoil energy that is sufficient to cause bond breakage leading to the systemic dissemination of daughter radionuclides and consequently whole-body radiation in general and bone marrow damage from the long-term accumulation of these free daughter radionuclides in the functional bone marrow [29].
212Pb decays by beta emission (physical half-life = 10.6 h) via its short-lived daughter radionuclides, 212Bi (T1/2 = 60.6 min) and 212Po (T1/2 = 0.3 µs) [25]. Two major limitations with the clinical application of 212Pb for targeted radioligand therapy relate to the high initial kidney uptake and consequently imparting a high renal dose as well as the high recoil energy, which is high enough to cause to up to 36% of 212Bi, one of its daughter radionuclides, to dissociate from the complexes [25, 30, 31].
211At has a physical half-life of 7.2 h. It decays by electron capture (58.3%) to 211Po (T1/2 = 0.52 s). Moreover, 211Po emits K X-rays that allow for the quantification of 211At radioactivity and scintigraphic imaging of 211At in vivo [32]. The challenge with 211At-PSMA is the high uptake in renal proximal tubules and late nephrotoxicity, as well as its limited availability [32, 33].
A detailed discussion of the radiochemistry and clinical evidence derived from 223Ra is presented in another article in this issue. Briefly, 223Ra is an alkaline earth metal, which forms very weak complexes [34]. To overcome this limitation, one study investigates the encapsulation of 223Ra into functionalized nanozeolites for TAT, with no definite results yet [35].
227Th has a physical half-life of 18.7 days and decays through radioactive 223Ra, which subsequently decays to stable 207Pb. During this decay scheme, five alpha particles are emitted [36]. Although 227Th-PSMA has been shown to have antitumor effect, reports on its impact on survival and its long-term toxicity are being awaited.
Recoil effect
Alpha emission is a highly energetic process. Following the emission of an alpha particle, the resultant daughter radionuclide experiences recoil energy like the recoil effect felt when firing a gun. The energy of the recoil effect may be significant enough to cause the breakage of the bond between the daughter radionuclide and the ligand. When this happens, the released daughter radionuclide may be retained within the tumor and contribute to the overall cytotoxicity if the radioligand was internalized before bond breakage or circulate freely and be transported to other organs where it can accumulate and cause off-target damage of healthy organs [37]. The recoil effect in TAT may be mitigated by ensuring a fast tumor uptake of the radioligand and rapid renal excretion of unbound radioligand, intra-tumoral injection of the radioligand, or by encapsulation in a nano-carrier.
The rapid tumor uptake approach of the radiopharmaceutical has been used for targeting agents like PSMA as it is suitable for this strategy [38]. An excellent example of this strategy for PSMA-based TAT is the use of 225Ac as an atomic in vivo nanogenerator, in which 225Ac (T1/2 = 9.9 days) is administered for therapy leading to in vivo decay to 213Bi, its daughter radionuclide. This approach has overcome the limitation of the short physical half-life of 213Bi (T1/2 = 46 min). The higher number of alpha particles when the parent radionuclide is used for therapy (e.g., net α-energy of 28 MeV for 225Ac) compared with the daughter radionuclide ensures more significant tumoral cytotoxicity, constituting another attraction for the use of in vivo nanogenerators [26, 39]. Figure 1 from the paper by Roscher and colleagues shows the nuclear recoil effect during α-decay within radioligand for TAT [37].
Schematic representation of two hypothetical scenarios describing the fate of the recoiling daughter radionuclide that gets released from the chelating moiety of TAT-P in vivo. The upper section labelled “No TAT-P internalization” depicts a daughter radionuclide that is released into the blood stream while causing either unspecific local damage to healthy tissue or travels further with the blood stream and causes analogical damage distantly elsewhere. The lower section labelled “TAT-P internalization” depicts TAT-P that specifically internalizes into the targeted tumor cell. The daughter radionuclide is then released with a high probability inside the tumor cell or to a minor extent might escape the tumor cell and cause damage not only to the target tumor cell but, depending on the traveled distance, to other cells as well
Current clinical experience with targeted alpha therapy of prostate cancer
213 Bi-PSMA
213Bi (T1/2 = 46 min) is a mixed alpha/beta emitter that decays via beta emission to 213Po, an ultra-short-lived pure alpha emitter (T1/2 = 4.2 µs, Eα = 8.375 MeV, branching ratio = 97.8%). Alternatively, 213Bi decays to 209Tl via alpha particle emission (Eα = 5.549 MeV, 0.16%, Eα = 5.869 MeV, 2.01%, branching ratio = 2.2%). Both 213Po and 209Tl decay to 209Pb (a beta emitter with T1/2 of 3.25 h), which eventually decays to 209Bi (T1/2 = 1.9 × 1019 year). The alpha particle emitted by 213Po (with a path length in the tissue of 85 µm) [26] is the main driver of the cytotoxicity caused by 213Bi-based TAT as it contributes about 98% of the total energy due to all alpha particle emissions by 213Bi. The particle energy contributed by beta emission in the decay scheme of 213Bi is minimal (7.3%) [40]. The gamma photon emitted during 213Bi decay (440 keV, emission probability of 26.1%) is useful for SPECT imaging for biodistribution and dosimetric studies [26].
In the preclinical assessment of the efficacy of 213Bi-labelled PSMA inhibitor, effective cytotoxicity in cell lines overexpressing PSMA was demonstrated with 213Bi-J591 [41]. The radioimmunoconjugate was also found capable of determining effective cytotoxicity in cell lines overexpressing PSMA and in animal models of prostate cancer [41, 42]. No clinical studies demonstrating the efficacy and safety of 213Bi-J591 in the treatment of mCRPC have been reported yet.
Progress was made when Sathekge and colleagues presented the first-in-human treatment with two cycles and a cumulative activity of 592 MBq of 213Bi-PSMA-617 in a patient with mCRPC, with disease progression under conventional therapy [43]. TAT with 213Bi-PSMA-617 achieved a significant biochemical and imaging response [43]. Continued clinical application of 213Bi-PSMA-617 for the treatment of mCRPC has been limited. This has mainly been due to a preliminary dosimetric report, calculated in three patients with mCRPC submitted to PET/CT with 68 Ga-PSMA and extrapolated to the half-life of 213Bi, providing a therapeutic index for 213Bi-PSMA-617 that is inferior compared to 225Ac-PSMA-617 [44].
225 Ac-PSMA
225Ac (T1/2 = 9.9 days) decays via a cascade of six short-lived daughter radionuclides to near-stable 209Bi (T1/2 = 1.9 × 1019 year) [45, 46]. The predominant decay path of 225Ac yields a net of 4 alpha particles (Eα of 5.8 MeV to 8.4 MeV, tissue range of 47 to 85 µm) and two beta particles (energy ranges of 0.6 to 1.6 MeV) [40]. Two gamma photons emitted during 225Ac decay (221Fr disintegration, 218 keV, 11.6% emission probability, and 213Bi disintegration, 440 keV, 26.1% emission probability) may provide a limited opportunity for imaging the in vivo distribution of the radionuclide [47,48,49].
The practice of 225Ac-PSMA radioligand therapy
Much of the clinical practice of 225Ac-PSMA TAT is derived from lessons learned from the clinical application of 177Lu-PSMA for PSMA-based radioligand therapy (PRLT) of mCRPC. Practice guidelines on the application of 177Lu-PSMA-617 for PRLT of mCRPC have been published by many professional societies and groups [50,51,52,53,54,55].
Patient selection for 225 Ac-PSMA therapy
The typical patient selected to undergo TAT with 225Ac-PSMA will be a patient with histologically confirmed prostate cancer whose disease has become castration-resistant and has progressed on conventional therapies. The decision to treat a patient with 225Ac-PSMA should be made in a multidisciplinary setting where the disease history, prior therapies, patient’s comorbid conditions and health state, available alternative treatments, and the patient’s wishes are thoroughly discussed. After this discussion, the multidisciplinary team must agree that 225Ac-PSMA therapy is the most suitable therapy option for the patient. Based on the known toxicity of 225Ac-PSMA therapy, sufficient vital organ reserve, especially of the bone marrow and kidneys, must be present before submitting a patient to TAT with 225Ac-PSMA. Acceptable organ reserve commonly applied in routine clinical practice is as follows:
-
Bone marrow function: hemoglobin level > 8 g/dL; platelet count > 75 × 109/L, white cell count > 3 × 109/L
-
Renal function: serum creatinine < 2 times the upper limit of normal
Prostate cancer becomes highly heterogeneous in the advanced stage of the disease, especially after multiple lines of therapy of mCRPC. Successful application of PSMA-based radioligand therapy, with alpha- or beta-emitting radionuclide, is based on sufficient expression of PSMA in all lesions. Therefore, a baseline imaging to demonstrate sufficient PSMA expression in tumor foci is vital in selecting patients for TAT with 225Ac-PSMA. A sufficient PSMA expression has traditionally been described as uptake above the physiologic PSMA uptake in the normal liver tissue. The level of PSMA expression is a significant predictor of response to 225Ac-PSMA therapy [56]. It is important to note that certain PSMA ligands such as PSMA-1007 have high hepatic background activity compared with most other PSMA ligands [57]. In the situation where 18F-PSMA-1007 PET/CT is obtained for baseline imaging, caution must be exercised in using hepatic background activity as reference standard to define sufficient PSMA expression in mCRPC lesions. Mediastinal blood-pool activity may be used as alternative internal reference in this situation. Given the known heterogeneity of PSMA expression within and between lesions [56], a determination must be made of the sufficient PSMA expression in all lesions. This determination becomes more critical in TAT considering the shorter tissue range of alpha particles which may fail to induce a significant crossfire effect in a tumor lesion with a widely dispersed pattern of PSMA expression.
Except in the circumstances where there is a failure of response to 177Lu-PSMA therapy, or mCRPC has progressed after an initial response to 177Lu-PSMA, in most instances, patients who qualify to receive 225Ac-PSMA may be found suitable for 177Lu-PSMA as well. It, therefore, becomes pertinent to design a rational approach to determine the more suitable of the two therapy options for each patient. The red marrow is a common site of prostate cancer metastases. It is not unusual to encounter diffuse metastases of prostate cancer to the axial skeleton in a manner typical of superscan [58]. In such instances, it may be prudent to treat such patients with 225Ac-PSMA due to its shorter tissue range to preserve the functional marrow [59]. Baseline PSMA imaging with either SPECT or PET technique helps make this selection [57, 60, 61].
Another factor that may be of paramount consideration in selecting between alpha- and beta-emitting radioligand for targeted therapy of mCRPC is the size of lesions. The dose delivered to a tumor mass by radionuclide therapy is directly proportional to the size [62]. Due to the limited radiation dose delivered to tissue per micron of tissue traversed by beta particles, 177Lu-PSMA is, therefore, unlikely to be effective in eliminating small lesions due to mCRPC [63]. These patients with suspected or confirmed sub-centimeter lesions or micrometastases of mCRPC may be more effectively treated with 225Ac-PSMA than 177Lu-PSMA.
Recent prospective trials of 177Lu-PSMA-617 in mCRPC have shown the value of adding 18F-fluorodeoxyglucose (18F-FDG) PET/CT to the initial assessment of patients being worked up for PRLT [7, 8]. In one of those trials, 16% of patients failed eligibility due to discordance between 18F-FDG PET and 68 Ga-PSMA PET; metastatic lesions visualized on 18F-FDG PET were not PSMA-avid on 68 Ga-PSMA PET [7]. Superselection of patients for PRLT in this manner appears to result in a better PSA response rate and should be performed if available resources are permitting [7, 8, 55]. No published evidence is available currently on the impact of the addition of 18F-FDG PET/CT in the assessment of patient suitability for 225Ac-PSMA. In our practice and in most other centers administering 225Ac-PSMA for therapy of mCRPC across the world, 18F-FDG PET is not routinely used in the selection of patients for TAT.
Preparation for therapy administration
225Ac-PSMA should be administered following national regulations on the safe use of unsealed radiation sources in a facility that is suitably equipped and staff trained in administering radionuclide therapy and managing accidental radiation contamination of persons and site. In preparation for therapy administration, baseline blood tests should be obtained for efficacy and toxicity monitoring. These baseline blood tests should include the following:
-
Serum PSA.
-
Full blood count.
-
Serum electrolyte, urea, and creatinine.
-
Estimated glomerular filtration rate (eGFR).
-
Liver function tests.
-
Dynamic renal scintigraphy is indicated to demonstrate dilatation or obstruction in the renal collecting system. Procedures to relieve obstruction are indicated in patients with obstruction in their renal collecting system to prevent an undue increase in renal dose.
Consenting forms an essential aspect of patient preparation for radionuclide therapy. Consenting includes but is not limited to providing comprehensive information regarding 225Ac-PSMA in terms of efficacy and side effects, the goal of treatment, and alternative therapy options available to the patient. It must be made clear to the patients that 225Ac-PSMA is not yet an approved agent for therapy of mCRPC and is applied on a compassionate ground or as part of a clinical trial in qualifying patients.
To prevent additive toxicity on the functional bone marrow, all myelotoxic therapies must be discontinued for a minimum of 6 weeks, and hematologic indices return to an acceptable threshold as indicated above before 225Ac-PSMA administration. No contraindication exists to co-administration of androgen deprivation therapy (ADT) with 225Ac-PSMA. Continued use of ADT should be based on clinical indication. There is no indication to discontinue bone-supporting agents such as bisphosphonates and RANK ligand inhibitor (denosumab).
Therapy administration
225Ac-PSMA is administered intravenously via a free-hand slow bolus injection given over 20 to 30 s. To enhance renal excretion of unbound radioligand, 1 to 2 l of an intravenous physiologic solution such as Ringer’s lactate or normal saline should be administered for 4 h, commencing 30 min before 225Ac-PSMA administration. This rate and volume of fluid administration must be tailored towards the prevailing medication conditions in the patient. Certain conditions such as congestive cardiac failure, when present, may preclude the generous hydration of the patient. Urethral catheterization for 48 h may be indicated in the incontinent patient to prevent radiation contamination of self and environment.
225Ac-PSMA presents no significant radiation burden to people in close contact with the treated patients due to the low activity of the radioligand administered for treatment (one-thousandth times lower than the activity of 177Lu-PSMA). Therefore, the decision to treat a patient with 225Ac-PSMA on either an in- or outpatient basis should be in accordance with the national laws. In climes where the national laws are permitting, 225Ac-PSMA therapy can be administered on an outpatient basis.
Follow-up and response assessment
Follow-up visits must be scheduled to monitor toxicities and determine treatment efficacy. Baseline blood tests (serum PSA; serum urea, electrolytes and creatinine levels, creatinine clearance for eGFR, liver function tests) should be performed as required during follow-up for safety and efficacy assessments. Treatment is repeated after 8 weeks. Follow-up blood tests should be done within 2 weeks of the next treatment cycle. Treatment is repeated for up to 6 cycles or more provided there is continued demonstrable efficacy in the absence of severe toxicity.
The assessment of treatment efficacy should be done in three domains: PSA response, radiological response, and clinical response [64]. PSA response is determined as recommended by the Prostate Cancer Clinical Trial Group as follows [65]:
-
PSA response: PSA decline ≥ 50% from baseline measured twice 3 to 4 weeks apart
-
PSA progression: rise in PSA by 25% from the nadir and an increase of at least 2 ng/mL
-
Stable PSA: decline < 50% or rise < 25%
Radiological response is traditionally determined using morphologic imaging with CT or magnetic resonance imaging (MRI) using the Response Evaluation Criteria in Solid Tumors 1.1 (RECIST 1.1). Some recent studies have shown the potential of 68 Ga-PSMA PET/CT for response assessment in patients treated for mCRPC [66,67,68]. 68 Ga-PSMA criteria for response assessment in men treated for prostate cancer have recently been published by a multidisciplinary team of urologists, radiologists, and nuclear medicine physicians [69]. 68 Ga-PSMA PET/CT may find greater application in response assessment of prostate cancer therapy as it has already been shown to outperform conventional imaging with CT and bone scan in localizing prostate cancer lesions [70, 71]. It must be borne in mind, however, that one of the mechanisms by which mCRPC become resistant to PSMA-based radioligand therapy with alpha- or beta-emitting radionuclides is by downregulating PSMA expression [72, 73]. Reliance on imaging findings on 68 Ga-PSMA PET imaging alone may lead to failure to confirm disease progression when lesions downregulate their expression of PSMA.
Clinical response is based on improvement in disease-related symptoms. Clinical assessment should also be done to determine treatment-related toxicities. The clinical impact of prostate cancer therapy is best assessed objectively using validated questionnaires such as the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC-QLQ), Patient-Reported Outcomes Measurement Information System, Brief Pain Inventory, etc.
Current evidence for the efficacy of 225Ac-PSMA therapy in mCRPC
The first set of studies demonstrating the efficacy of 225Ac-PSMA in the treatment of mCRPC came from Heidelberg, Germany. A report of two patients who had exhausted available conventional therapies, one of whom was deemed ineligible for 177Lu-PSMA due to diffuse red marrow metastases of mCRPC and the other experienced disease progression on 177Lu-PSMA therapy, was the first to show the efficacy of 225Ac-PSMA-617 in large volume metastases of mCRPC [38]. In the patient with diffuse marrow metastases of mCRPC, normalization of serum PSA and 68 Ga-PSMA PET/CT imaging findings occurred after four cycles of 225Ac-PSMA-617 with no significant change in hematologic indices. In the other patient with radioresistant to beta-emitting radionuclide therapy with 177Lu-PSMA therapy, a large volume of peritoneal metastases invading into the liver resolved, and serum PSA dropped to below detectable limit after three cycles of 225Ac-PSMA-617 [38]. This report provided the first preliminary insights into the capability of 225Ac-PSMA TAT for mCRPC, including its safety and efficacy in the setting of diffuse red marrow metastases, its effectiveness in the setting of radioresistant to PRLT with a beta-emitting radionuclide, its ability to eradicate large volume metastases, and its efficacy as a last-line therapy in patients who have failed multiple lines of therapy for mCRPC.
In 2017, in collaboration with scientists at the Joint Research Centre of the European Commission, the Heidelberg group published a follow-up dose-escalation study to define the optimum activity required to achieve the maximum antitumor effect and the dose-limiting organs [74]. A group of 14 patients was treated with an escalating activity of 225Ac-PSMA-617, from 50 KBq/Kg body weight to 200 KBq/Kg. Xerostomia was the commonest treatment-related side effects prevalent in patients treated with 100KBq/Kg and above. Based on their findings, the authors arrived at 100 KBq/Kg as the maximum tolerable activity for 225Ac-PSMA-617 and xerostomia as the dose-limiting toxicity [74]. This study has influenced the global practice of TAT of mCRPC as findings from it have been used to guide empirical dosing of 225Ac-PSMA.
The sequencing of agents used in the treatment of mCRPC is critical as agents applied earlier in the disease course achieve better response compared with agents applied later in the treatment sequence. The most recent and the largest study from the Heidelberg group and their collaborators demonstrated superior efficacy of 225Ac-PSMA-617 applied as a last-line therapy agent in heavily pretreated patients compared with approved agents that were applied earlier in the treatment sequence of the patients [75]. Using a swimmer-plot analysis, the group showed the relative durations of tumor control induced by different life-prolonging therapies of mCRPC. The average duration of tumor control induced by any first-, second-, third-, or fourth-line agent, regardless of the agent, was 8.0, 7.0, 6.0, and 4.0, respectively. The average duration of tumor control induced by 223RaCl2, cabazitaxel, enzalutamide, docetaxel, and abiraterone, regardless of the time the particular agent was applied in the treatment sequence, was 4.0, 6.0, 6.5, 6.5, and 10.0 months, respectively. 225Ac-PSMA-617 induced an average duration of tumor control of 9.0 months in a cohort of patients 85, 70, 60, 22.5, and 12.5% of whom had prior therapy with abiraterone, docetaxel, enzalutamide, 223RaCl2, and cabazitaxel, respectively [75]. This study added important insights to the knowledge on 225Ac-PSMA therapy in mCRPC, confirming its antitumor activity in patients who have exhausted or have limited therapy options available for their treatment. In addition, the study showed, perhaps, a better duration of disease control inducible by 225Ac-PSMA therapy compared with the available approved agents with life-prolonging capability.
The largest series so far published on the application of 225Ac-PSMA-617 for mCRPC was from Pretoria, South Africa [76]. In a cohort of 73 men with mCRPC who were treated with a total of 210 cycles of 225Ac-PSMA-617 (median treatment cycle = 3, range = 1–8), PSA response (decline in serum PSA of 50% or more) was seen in 70% of patients, while any decline in serum PSA was seen in 82% of the patients. There was complete normalization of imaging findings assessed by 68 Ga-PSMA PET/CT in 28.8% of the patients. The progression-free survival (PFS) and overall survival (OS) were 15.2 (95% CI, 13.1–17.4) months and 18 (95% CI, 16.2–19.9) months, respectively [76]. This study showed, in a relatively large cohort of patients, the efficacy, durability of disease control, and survival inducible by 225Ac-PSMA-617 therapy of mCRPC (Fig. 2).
The Indian experience with the use of 225Ac-PSMA-617 in mCRPC has recently been reported from New Delhi [77]. In a cohort of 28 patients, 89% of patients had any PSA decline 8 weeks after the first cycle of 225Ac-PSMA-617. After administering a total of 85 cycles of 225Ac-PSMA-617 in the 28 patients, 78.6% of the patients achieved any PSA decline, while 39% of patients achieved a PSA decline of 50% or more. Despite this relatively low PSA response rate, a median PFS and OS of 12 (95% CI, 9–13) months and 17 (16, not reached) months were attained. Clinical response assessed by visual analog score, analgesic score, Eastern Cooperative Oncology Group performance status, and Karnofsky performance status showed significant improvement in favor of clinical benefit of 225Ac-PSMA-617 for mCRPC treatment [77]. This Indian study advanced knowledge by providing evidence to support the clinical benefits of 225Ac-PSMA-617 in mCRPC as it relates to improvement in the severity of pain, a corresponding reduction in the need for analgesic, and an improvement in patients’ performance of the activities of daily living.
A second Indian study from Chandigarh has also shown the impact of 225Ac-PSMA-617 on the health-related quality of life of 11 patients who had failed treatment with two or more lines of approved agents for mCRPC [78]. After a median of 2 cycles of 225Ac-PSMA-617, 46% of patients achieved a PSA decline of 50% or more. Health-related quality of life assessed by a validated questionnaire assessing physical wellbeing, emotional wellbeing, treatment-related side effects, and functional wellbeing showed an overall significantly improvement post-treatment with 225Ac-PSMA-617. Among the four domains evaluated by the questionnaire, significant improvement occurred in the physical and emotional wellbeing domains. The physical symptoms that showed improvement with 225Ac-PSMA-617 therapy were pain, difficulty with urination, fatigue, and restriction in physical activity [78]. The positive impact of 225Ac-PSMA-617 on patients’ quality of life was also demonstrated in a report from Nijmegen, the Netherlands, of Dutch patients treated at Heidelberg, Germany, with 225Ac-PSMA-617 for mCRPC [79]. The patients reported outcome assessed by the EORTC-QLQ-30 and BM-22 questionnaires showed a significant decrease in pain complain and a corresponding decrease in the need for analgesics. There was a progressively increase in the scores for physical and role functioning scales from after therapy completion [79]. Put together, these three studies show a consistent improvement in the quality of life of patients with mCRPC who were treated with 225Ac-PSMA-617.
In the last few years, different groups have reported insightful cases of treatment outcome of mCRPC with 225Ac-PSMA-617, including remarkable response in patients with visceral metastases [80, 81], long-lasting remission [82], and some rare treatment-related side effects [83, 84]. Table 2 summarizes clinical studies reporting the treatment outcome of mCRPC with 225Ac-PSMA TAT.
PSMA-617 is the most commonly applied PSMA inhibitor for PRLT of prostate cancer. PSMA-I&T is a less commonly used PSMA inhibitor with similar biokinetics and excellent binding capacity at a nanomolar concentration as PSMA-617 [11, 85]. Ilhan and colleagues from Munich, Germany, reported a case showing a good antitumor effect of 225Ac-PSMA-I&T in a patient previously treated with 10 cycles of 177Lu-PSMA-617 [86]. The group subsequently published their experience on the use of 225Ac-PSMA-I&T in 14 men with mCRPC. After a total of 34 cycles of 225Ac-PSMA-I&T (median = 7, range = 1–5), 78.6% and 50% of patients had any PSA decline and ≥ 50% PSA decline, respectively [87].
Efficacy of 225Ac-PSMA in the post−177Lu-PSMA therapy setting
177Lu-PSMA is the more commonly applied agent for radionuclide therapy of mCRPC due to its wider availability and a more robust clinical experience with its use. 177LuPSMA is an effective treatment modality for mCRPC. However, a significant proportion of patients will not respond, and of those who respond, many will experience disease progression after several months [5,6,7]. 225Ac-PSMA TAT has been applied as a salvage therapy in patients who do not respond to and experience disease progression after an initial response to 177Lu-PSMA therapy on the background that 225Ac-PSMA can overcome radioresistant to 177Lu-PSMA in mCRPC [38]. Many of the published series on 225Ac-PSMA therapy of mCRPC have included patients with prior history of 177Lu-PSMA therapy. In the Pretoria series by Sathekge et al. [76], patients with a prior history of 177Lu-PSMA therapy had a significantly shorter PFS (5.1 months, 95% CI, 3.8–6.5 months versus 16.5 months, 95% CI, 14.3–18.7 months) compared with 177Lu-PSMA therapy-naïve patients. On multivariate analysis, prior 177Lu-PSMA therapy was significantly associated with shorter PFS [76]. In the Indian series by Yadav and colleagues, PFS and OS were shorter in patients with a history of prior 177Lu-PSMA therapy compared with patients without; the difference did not reach statistical significance, however, probably due to the small study population [77].
To evaluate the efficacy of 225Ac-PSMA in the post-177Lu-PSMA setting further, the authors from Munich, Germany, and their collaborators reported their experience with the use of 225Ac-PSMA-617 therapy in heavily pretreated patients who had failed a median of six prior regimens for mCRPC, including prior 177Lu-PSMA therapy [88]. Any PSA decline and PSA decline of 50% or more were seen in 88.5% (95% CI, 70–97%) and 65.4% (95% CI, 46–81%), respectively. The median PSA-PFS and OS were 3.5 (95% CI, 1.8–11.2) months and 7.7 (95% CI, 4.5–12.1) months. The presence of liver metastases at the initiation of treatment was a significant predictor of a shorter PSA-PFS and OS. Treatment of mCRPC with 225Ac-PSMA in this cohort of patients that had progressed on 177Lu-PSMA therapy did not produce any measurable changes on the quality of life of the patients assessed by the EORTC-QLQ30 questionnaire [88]. The results from this study clearly show a good PSA response to 225Ac-PSMA in the post-177Lu-PSMA setting, albeit for a short duration without a corresponding improvement in the global health status of the patients. Randomized controlled trials will be needed in the future to stratify patients to either 177Lu-PSMA or 225Ac-PSMA so that the better therapy is administered in the treatment sequence when it is likely to have the best impact.
Two interesting studies have been recently published on the efficacy of 225Ac-PSMA in patients with prior history of 177Lu-PSMA therapy. Rather than applying 225Ac-PSMA alone, 177Lu-PSMA and 225Ac-PSMA were applied tandem for mCRPC in the two studies. In the study by Khreish et al. from Homburg, Germany, 20 patients who had demonstrated insufficient response to 177Lu-PSMA monotherapy were treated with one course of 225Ac-PSMA-617/177Lu-PSMA-617 applied in tandem (mostly on consecutive days) [89]. PSA response was achieved in 50% of patients 6 to 8 weeks after tandem therapy. Response to tandem therapy was not significantly different between patients who showed an earlier response to prior 177Lu-PSMA-617 therapy before developing resistance (n = 12) versus those patients who never responded to the prior 177Lu-PSMA-617 therapy (n = 8) [89]. This study highlighted the antitumor activity of 225Ac-PSMA-617 against two patterns of radioresistant to beta-emitting radionuclide therapy of mCRPC. The Homburg group has also reported their experience with one course of 225Ac-PSMA-617/177Lu-PSMA-617 administered in tandem to a different cohort of patients with prior history of response to 177Lu-PSMA-617 therapy [90]. In this latter study, response was assessed by serum PSA and functional parameters derived from 68 Ga-PSMA PET/CT. PSA response and partial response assesses by 68 Ga-PSMA PET/CT was seen in 29.4% of patients, with a 70.6% concordance in response assessed by serum PSA and 68 Ga-PSMA PET/CT [90]. This latter study, in addition to showing the antitumor activity of tandem 225Ac-PSMA-617/177Lu-PSMA-617 in patients with disease progression after an initial response to 177Lu-PSMA-617 monotherapy, demonstrated the potential role of molecular indices derived from 68 Ga-PSMA PET/CT for response assessment and their concordance with response assessment with serum PSA.
225Ac-PSMA: upfront application in the chemotherapy-naïve setting
Despite the availability of multiple life-prolonging therapy options for mCRPC, there is no consensus on the sequence at which to apply them for treatment. It is known that agents applied earlier in the treatment sequence achieve better responses than agents applied later in the sequence. Randomized control trials are needed to determine the rightful place of each agent in the treatment sequence of mCRPC. A couple of studies have shown a better response of PRLT with 177Lu-PSMA in the chemotherapy-naïve patients [6, 91].
Our group in Pretoria, South Africa, published a unique cohort of chemotherapy-naïve men with mCRPC who had upfront treatment with 225Ac-PSMA [92]. These were men who either declined treatment with taxane-based chemotherapy agents or had no access to them. In 88% of patients, serum PSA declined by 50% or more after a median of three cycles of 225Ac-PSMA-617. In 41% of patients, serum PSA declined to below detectable limit and remained so after a median follow-up duration of 12 months. In 65% of the patients, there was normalization of 68 Ga-PSMA PET/CT findings with tracer uptake in all malignant lesions reducing to background activity level (Fig. 3). While this remarkable response is exciting and holds much promise for applying 225Ac-PSMA-617 in treating men with mCRPC, it may also represent a response achieved in less aggressive disease. mCRPC evolves, acquiring more aggressive behavior as different lines of treatments are applied to it.
Toxicity
Treatment-related side effects of 225Ac-PSMA TAT can be direct or indirect. Direct toxicity results from damage induced by alpha particles in organs expressing PSMA or organs involved with the excretion of the radioligand. Organs expressing significant PSMA expression include salivary glands, lachrymal glands, enterocytes of the small bowel, and the epithelial lining of the proximal convoluted tubules [93, 94]. The salivary glands are the dose-limiting organs at the activities administered for 225Ac-PSMA TAT [60]. Salivary gland damage causing xerostomia is, therefore, the commonest treatment-related toxicity of 225Ac-PSMA TAT observed in up to about 72.7% of treated patients [95]. Xerostomia leads to many other indirect side effects of treatment, including dysgeusia, reduced food intake, dyspepsia, weight loss, and constipation [76].
Salivary gland uptake of PSMA radioligand occurs via specific receptor binding and non-specific trapping [96]. The severity of xerostomia and its impact on the quality of life of patients treated with 225Ac-PSMA has led to a lot of interest in designing ways to mitigate against its incidence and severity. None of the currently tested methods is universally effective in addressing xerostomia as a treatment-related side effect of 255Ac-PSMA TAT. The simplest intervention applied for reducing salivary gland toxicity is by external cooling of the gland during therapy administration. This intervention is premised on the theory of reduced radioligand delivery to the major salivary glands due to the vasoconstrictive effect induced by external cooling. The effectiveness of this intervention is still under debate [97, 98]. Competitive inhibition for binding at PSMA receptor expressed in normal organs has been attempted with cold PSMA or PSMA congeners such as monosodium glutamate as another way to reduce off-target PSMA radioligand uptake in the salivary glands [99,100,101,102,103]. While this competitive inhibition may successfully reduce off-target PSMA radioligand in normal organs such as the salivary gland, a reduction in tumor uptake is possible [102]. Ligand modification in which radioligand preferentially binds to tumor-expressed PSMA but not PSMA expressed in normal organs appears exciting and. if successful, may have a great impact on the practice of PRLT of mCRPC [104]. Other pharmacologic interventions that have been tried for their ability to reduce salivary gland uptake of PSMA radioligands are botulinum injection, anti-cholinergic use, and injection of local anesthetic agents [105, 106]. Sialendoscopy with dilatation, saline irrigation, and steroid injection into the ducts of major salivary glands has been attempted to ameliorate the impact of xerostomia in patients treated with 225Ac-PSMA TAT [107].
Treatment de-escalation is an intervention that has been specifically utilized in 225Ac-PSMA TAT to reduce the incidence and severity of treatment-induced xerostomia. In this strategy popularized by our group in Pretoria, treatment commences with 8 MBq of 225Ac-PSMA. 68 Ga-PSMA PET/CT is used to assess for the volume of residual disease and response to therapy. Administered activity is reduced to 6 or 4 MBq in subsequent treatment cycles according to the volume of residual tumor load. This strategy is based on the principle of tumor sink effect in which more radioligand is available for binding in normal organs with reducing tumor bulk induced by successful treatment [108]. This strategy has been successful as none of our patients has experienced grade III xerostomia or discontinued 225Ac-PSMA therapy due to dry mouth [76, 92]. A second specific approach to reduce the incidence and severity of 225Ac-PSMA-induced xerostomia is tandem administration of 225Ac-PSMA and 177Lu-PSMA. This approach popularized by the Homburg group uses a lower activity of 225Ac-PSMA (an average of 5.3 MBq) combined with a standard activity of 177Lu-PSMA to achieve an optimum antitumor effect without the undesirable severe xerostomia inducible by a standard activity of 225Ac-PSMA [89, 90]. In one of their studies reporting the outcome of 225Ac-PSMA-617/177Lu-PSMA-617 tandem therapy, 40% and 25% of patients reported grades I and II xerostomia, respectively [89]. This relatively lower frequency of very mild to mild xerostomia was seen despite a prior history of pretreatment with 177Lu-PSMA-617 in the cohorts (median = 4 cycles, range = 1–13 cycles) [89].
Despite being administered in heavily pretreated patients with limited bone marrow reserve and in patients with predominant diffuse red marrow metastases, 225Ac-PSMA TAT is rarely associated with grades III/IV hematologic toxicities [38, 75, 76]. A recent meta-analysis of 10 studies, including 256 patients treated with 225Ac-PSMA, ≥ grade3 anemia, leucopenia, and thrombocytopenia, was seen in 12.8%, 8.3%, and 6.3%, respectively [95]. The proportions of patients who developed any grade of hematologic toxicity following 177Lu-PSMA RLT are 4–85% for anemia, 3–53% for leucopenia, and 5–47% for thrombocytopenia [5]. The shorter path length of alpha particles compared with beta particles ensured that high energy is deposited within the targeted bone metastases with a limited dose delivered to the surrounding red marrow [109].
Renal toxicity is another potential side effect of 225Ac-PSMA therapy [84]. In the meta-analysis of 10 studies by Satapathy and colleagues, only 3.8% of patients were reported to have ≥ grade III renal toxicity [95].
Resistance and mutation
Several genotypic and phenotypic characteristics have been noted to drive resistance to TAT with 225Ac-PSMA-617. The most used phenotypical characteristic to select patients for PRLT is the level of PSMA expression. Low PSMA expression corresponds to a high tumor proliferative index and poor survival after 225Ac-PSMA TAT [79]. Therapy-induced neuroendocrine differentiation is another histologically determined phenotype that portends poor treatment outcomes [79]. Visceral metastases occur at a very advanced stage of mCRPC. Metastases to soft tissue visceral, especially to the liver, are poor prognostic indicators [88].
Early evidence from genomic and proteomic studies has shown a prevalence of mutations in the DNA damage repair machinery in the tumor cells of prostate cancer resistant to TAT with 225Ac-PSMA. The p53 gene, acting via cyclin and cyclin-dependent kinases, functions as the guardian of the genome by halting cell cycle progression in response to DNA damage. In the preclinical study by Stuparu and colleagues, loss of TP53 was associated with poor response to TAT with 225Ac-PSMA-617 [110]. In the earlier clinical study by Kratochwil et al., patients with mCRPC resistant to 225Ac-PSMA-617 harbor at least one deleterious mutations (average of 2.2 per patient) in genes involved in DNA repair, including ATM, CHEK2, TP53, and BRCA2 [111]. The knowledge of these deleterious mutations is crucial for patient selection for TAT and for designing rational combination therapy that will exploit these genetic mutations for a better treatment outcome. Olaparib is a poly-[ADP-ribose]-polymerase 1 (PARP-1) inhibitor, a group of enzymes involved in repairing DNA breaks. Olaparib monotherapy was shown to prolong imaging-based PFS in men with mCRPC harboring alterations in at least one of BRCA1, BRCA2, or ATM genes [112]. The ability of olaparib to potentiate the antitumor effect of 177Lu-PSMA is currently being evaluated (NCT03874884). Immunotherapy with immune checkpoint inhibitors is a new addition to the armamentarium of cancer therapy options. Limited success has been achieved with the use of immunotherapy agents in the treatment of mCRPC. This limited success has been adduced to the immunological coldness (lack of immune cell invasion into the tumor) of prostate cancer resulting from poor expression of neoantigens [113]. Cytocidal effect of radionuclide therapy with alpha or beta-emitting radionuclide may be useful in releasing tumor neoantigen, thereby sensitizing host cellular immunity [114]. Czernin and colleagues showed, in a mouse model of mCRPC, that a combination of 225Ac-PSMA-617 and an inhibitor of PD-1 (program death-1) achieved better tumor control than monotherapy with either agent alone [115]. More research is needed to develop rational combinatorial therapies with synergistic effects and without overlapping toxicities for mCRPC.
Rechallenge options
Disease progression may occur in patients who initially show satisfactory response to 225Ac-PSMA therapy. As therapy alternative options may be limited or already exhausted in such patients, a rechallenge with 225Ac-PSMA may be considered. This consideration for rechallenge should be done within the context of a multidisciplinary tumor board. For patients to be considered suitable for rechallenge, such patients must have shown demonstrable response with no prohibitive severe treatment-induced toxicities to the earlier 225Ac-PSMA RLT. As part of the consideration for rechallenge, a determination must be made of the cumulative dose already delivered to target organs, especially the salivary glands, bone marrow, and the kidneys, so that the maximum tolerable doses to these organs are not exceeded. This caution becomes essential, especially in patients with a good prognosis and expectation for prolonged survival.
Where next?
Issues that are essential for the development of 225Ac-PSMA RLT are as follows:
-
Increased production capacity by creating multiple sustainable suppliers of 225Ac to cater for a global demand that is likely to increase tremendously in the near future. Morgenstern and colleagues recently reviewed the current issues around supply and efforts to expand production capacity [116].
-
Standardization of the techniques for GMP (good manufacturing practice) production of 225Ac-PSMA.
-
Development and standardization of imaging techniques to allow for in vivo biodistribution studies in humans for accurate dosimetry.
-
Performance of prospective multicenter studies followed by randomized control trials to validate the efficacy and safety of 225Ac-PSMA RLT against the current standard of care and define its place in the treatment algorithm of mCRPC. This should be with the eventual goal of securing regulatory approval for routine clinical applications.
Conclusion
This review paper sought to describe the current global experience with the application of 225Ac-PSMA RLT in the treatment of mCRPC. We provided a brief background to the most promising alpha-emitting radionuclides for potential application in TAT of mCRPC and the factors militating against the clinical translation of some of them. Importantly, we presented a detailed discussion on the practicality of patient selection, therapy administration, and patient follow-up for response assessment and detection of treatment-related side effects. The currently available evidence suggests that 225Ac-PSMA RLT is safe and efficacious in the treatment of mCRPC, even when applied in particularly challenging clinical situations. It is suitable for salvage therapy in patients who have failed other lines of therapy, including PSMA-based RLT with 177Lu-PSMA. These promising results have created the much-deserved excitement for the widespread clinical application of this novel therapy and for designing rational combinatorial approaches in its application alongside other agents for more effective therapy. Achieving these visions will require integration across many disciplines, including urology, oncology, radiology, radiochemistry, and nuclear medicine. Quality prospective data accrued in trial settings will be needed to validate the efficacy of PSMA-based TAT and to situate it in the treatment sequence of mCRPC.
Data availability
Not applicable.
Change history
17 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00259-021-05531-9
References
Velonas VM, Woo HH, dos Remedios CG, Assinder SJ. Current status of biomarkers for prostate cancer. Int J Mol Sci. 2013;14:11034–60.
Gillessen S, Omlin A, Attard G. Management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC). Ann Oncol. 2015;26:1589–604.
Basch E, Loblaw DA, Oliver TK, Carducci M, Chen RC, Frame JN, et al. Systemic therapy in men with metastatic castration-resistant prostate cancer: American Society of Clinical Oncology and Cancer Care Ontario clinical practice guideline. J Clin Oncol. 2014;32:3436–48.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu KN, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005.
Yadav MP, Ballal S, Sahoo RK, Dwivedi SN, Bal C. Radioligand therapy with 177Lu-PSMA for metastatic castration-resistant prostate cancer: a systematic review and meta-analysis. AJR Am J Roentgenol. 2019;213:275–85.
Ahmadzadehfar H, Rahbar K, Baum RP, Seifert R, Kessel K, Bögemann M, et al. Prior therapies as prognostic factors of overall survival in metastatic castration-resistant prostate cancer patients treated with [177Lu]Lu-PSMA-617. A WARMTH multicenter study (the 617 trial). Eur J Nucl Med Mol Imaging. 2021;48:113–22.
Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, et al. [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19:825–33.
Hofman MS, Emmett L, Sandhu S, Iravani A, Joshua AM, Goh JC, et al. [177Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): a randomised, open-label, phase 2 trial. Lancet. 2021;397:797–804.
Horoszewicz JS, Leong SS, Kawinski E, Karr JP, Rosenthal H, Chu TM, et al. LNCaP model of human prostatic carcinoma. Cancer Res. 1983;43:1809–18.
O’Keefe DS, Bacich DJ, Huang SS, Heston WDW. A perspective on the evolving story of PSMA biology, PSMA-based imaging, and endoradiotherapeutic strategies. J Nucl Med. 2018;59:1007–13.
Benesová M, Schäfer M, Bauder-Wüst U, Afshar-Oromieh A, Kratochwil C, Mier W, et al. Preclinical evaluation of a tailor-made DOTA-conjugated PSMA inhibitor with optimized linker moiety for imaging and endoradiotherapy of prostate cancer. J Nucl Med. 2015;56:914–20.
Foss CA, Mease RC, Fan H, Wang Y, Ravert HT, Dannals RF, et al. Radiolabeled small-molecule ligands for prostate-specific membrane antigen: in vivo imaging in experimental models of prostate cancer. Clin Cancer Res. 2005;11:4022–8.
Eder M, Eisenhut M, Babich J, Haberkorn U. PSMA as a target for radiolabelled small molecules. Eur J Nucl Med Mol Imaging. 2013;40:819–23.
DeMarzo AM, Nelson WG, Isaacs WB, Epstein JI. Pathological and molecular aspects of prostate cancer. Lancet. 2003;361:955–64.
Wright GL Jr, Haley C, Beckett ML, Schellhammer PF. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol Oncol. 1995;1:18–28.
Santoni M, Scarpelli M, Mazzucchelli R, Lopez-Beltran A, Cheng L, Cascinu S, et al. Targeting prostate-specific membrane antigen for personalized therapies in prostate cancer: morphologic and molecular backgrounds and future promises. J Biol Regul Homeost Agents. 2014;28:555–63.
Akhtar NH, Pail O, Saran A, Tyrell L, Tagawa ST. Prostate-specific membrane antigen-based therapeutics. Adv Urol. 2012;2012:973820.
Troyer JK, Beckett ML, Wright GL Jr. Detection and characterization of the prostate-specific membrane antigen (PSMA) in tissue extracts and body fluids. Int J Cancer. 1995;62:552–8.
Haberkorn U, Eder M, Kopka K, Babich JW, Eisenhut M. New strategies in prostate cancer: prostate-specific membrane antigen (PSMA) ligands for diagnosis and therapy. Clin Cancer Res. 2016;22:9–15.
Sgouros G, Roeske JC, McDevitt MR, Palm S, Allen BJ, Fisher DR, et al. MIRD pamphlet no. 22 (abridged): radiobiology and dosimetry of a-particle emitters for targeted radionuclide therapy. J Nucl Med. 2010;51:311–28.
Wulbrand C, Seidl C, Gaertner FC, Bruchertseifer F, Morgenstern A, Essler M, et al. Alpha particle emitting 213Bi-anti-EGFR immunoconjugates eradicate tumor cells independent of oxygenation. PLoS ONE. 2013;8:e64730.
Friesen C, Glatting G, Koop B, Schwarz K, Morgenstern A, Apostolidis C, et al. Cancer Res. 2007;67:1950–8.
Kratochwil C, Giesel FL, Bruchertseifer F, Mier W, Apostolidis C, Boll R, et al. 213Bi-DOTATOC receptor-targeted alpha-radionuclide therapy induces remission in neuroendocrine tumours refractory to beta radiation: a first-in-human experience. Eur J Nucl Med Mol Imaging. 2014;41:2106–19.
Seidl C. Radioimmunotherapy with alpha-particle-emitting radionuclides. Immunotherapy. 2014;6:431–58.
Juzeniene A, Stenberg VY, Bruland ØS, Larsen RH. Preclinical and clinical status of PSMA-targeted alpha therapy for metastatic castration-resistant prostate cancer. Cancers (Basel). 2021;13:779.
Morgenstern A, Apostolidis C, Kratochwil C, Sathekge M, Krolicki L, Bruchertseifer F. An overview of targeted alpha therapy with 225Actinium and 213Bismuth. Curr Radiopharm. 2018;11:200–8.
Ballangrud AM, Yang WH, Charlton DE, McDevitt MR, Hamacher KA, Panageas KS, et al. Response of LNCaP spheroids after treatment with an alpha-particle emitter (213Bi)-labeled anti-prostate specific membrane antigen antibody (J591). Cancer Res. 2001;61:2008–14.
Müller C, Domnanich KA, Umbricht CA, van der Meulen NP. Scandium and terbium radionuclides for radiotheranostics: current state of development towards clinical application. Br J Radiol. 2018;91:20180074.
Beyer GJ, Miederer M, Vranjes-Durić S, Comor JJ, Künzi G, Hartley O, et al. Targeted alpha therapy in vivo: direct evidence for single cancer cell kill using 149Tb-rituximab. Eur J Nucl Med Mol Imaging. 2004;31:547–54.
Gholami YH, Willowson KP, Forwood NJ, Harvie R, Hardcastle N, Bromley R, et al. Comparison of radiobiological parameters for (90)Y radionuclide therapy (RNT) and external beam radiotherapy (EBRT) in vitro. EJNMMI Phys. 2018;5:1–19.
de Kruijff RM, Wolterbeek HT, Denkova AG. A critical review of alpha radionuclide therapy-how to deal with recoiling daughters? Pharmaceuticals. 2015;8:321–36.
Lindegren S, Albertsson P, Bäck T, Jensen H, Palm S, Aneheim E. Realizing clinical trials with astatine-211: the chemistry infrastructure. Cancer Biother Radiopharm. 2020;35:425–36.
Kiess AP, Minn I, Vaidyanathan G, Hobbs RF, Josefsson A, Shen C, et al. (2S)-2-(3-(1-Carboxy-5-(4–211At astatobenzamido)pentyl)ureido)-pentanedioic acid for PSMA-targeted alpha-particle radiopharmaceutical therapy. J Nucl Med. 2016;57:1569–75.
Gott M, Yang P, Kortz U, Stephan H, Pietzsch HJ, Mamat CA. (224)Ra-labeled polyoxopalladate as a putative radiopharmaceutical. Chem Commun. 2019;55:7631–4.
Czerwińska M, Fracasso G, Pruszyński M, Bilewicz A, Kruszewski M, Majkowska-Pilip A, et al. Design and evaluation of (223)Ra-labeled and anti-PSMA targeted NaA nanozeolites for prostate cancer therapy-Part I. Materials. 2020;13:3875.
Larsen RH, Borrebaek J, Dahle J, Melhus KB, Krogh C, Valan MH, et al. Preparation of Th227-labeled radioimmunoconjugates, assessment of serum stability and antigen binding ability. Cancer Biother Radiopharm. 2007;22:431–7.
Roscher M, Bakos G, Benešová M. Atomic nanogenerators in targeted alpha therapies: Curie’s legacy in modern cancer management. Pharmaceuticals. 2020;13:76.
Kratochwil C, Bruchertseifer F, Giesel FL, Weis M, Verburg FA, Mottaghy F, et al. 225Ac-PSMA-617 for PSMA-targeted α-radiation therapy of metastatic castration-resistant prostate cancer. J Nucl Med. 2016;57:1941–4.
McDevitt MR, Ma D, Lai LT, Simon J, Borchardt P, Frank RK, et al. Tumor therapy with targeted atomic nanogenerators. Science. 2001;294:1537–40.
Sgouros G, Roeske JC, McDevitt MR, Palm S, Allen BJ, Fisher DR, et al. MIRD pamphlet no. 22 (abridged): radiobiology and dosimetry of a-particle emitters for targeted radionuclide therapy. J Nucl Med. 2010;51:311–28.
McDevitt MR, Barendswaard E, Ma D, Lai L, Curcio MJ, Sgouros G, et al. An alpha-particle emitting antibody ([213Bi]J591) for radioimmunotherapy of prostate cancer. Cancer Res. 2000;60:6095–100.
Filippi L, Chiaravalloti A, Schillaci O, Bagni O. The potential of PSMA-targeted alpha therapy in the management of prostate cancer. Expert Rev Anticancer Ther. 2020;20:823–9.
Sathekge M, Knoesen O, Meckel M, Modiselle M, Vorster M, Marx S. 213Bi-PSMA-617 targeted alpha-radionuclide therapy in metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2017;44:1099–100.
Kratochwil C, Schmidt K, Afshar-Oromieh A, Bruchertseifer F, Rathke H, Morgenstern A, et al. Targeted alpha therapy of mCRPC: dosimetry estimate of 213Bismuth-PSMA-617. Eur J Nucl Med Mol Imaging. 2018;45:31–7.
Pommé S, Marouli M, Suliman G, Dikmen H, Van Ammel R, Jobbágy V, et al. Measurement of the 225Ac half-life. Appl Radiat Isot. 2012;70:2608–14.
Suliman G, Pommé S, Marouli M, Van Ammel R, Stroh H, Jobbágy V, et al. Half-lives of (221)Fr, (217)At, (213)Bi, (213)Po and (209)Pb from the (225)Ac decay series. Appl Radiat Isot. 2013;77:32–7.
Gosewisch A, Schleske M, Gildehaus FJ, Berg I, Kaiser L, Brosch J, et al. Image-based dosimetry for 225Ac-PSMA-I&T therapy using quantitative SPECT. Eur J Nucl Med Mol Imaging. 2021;48:1260–1.
Vatsa R, Sood A, Vadi SK, Das CK, Kaur K, Parmar M, et al. 225Ac-PSMA-617 radioligand posttherapy imaging in metastatic castrate-resistant prostate cancer patient using 3 photopeaks. Clin Nucl Med. 2020;45:437–8.
Usmani S, Rasheed R, Marafi F, Naqvi SAR. Ac prostate-specific membrane antigen posttherapy α imaging: comparing 2 and 3 photopeaks. Clin Nucl Med. 2019;44:401–3.
Fendler WP, Kratochwil C, Ahmadzadehfar H, Rahbar K, Baum RP, Schmidt M, et al. 177Lu-PSMA-617 therapy, dosimetry and follow-up in patients with metastatic castration-resistant prostate cancer. Nuklearmedizin. 2016;55:123–8.
Fendler WP, Rahbar K, Herrmann K, Kratochwil C, Eiber M. 177Lu-PSMA radioligand therapy for prostate cancer. J Nucl Med. 2017;58:1196–200.
Rahbar K, Afshar-Oromieh A, Jadvar H, Ahmadzadehfar H. PSMA Theranostics: current status and future directions. Mol Imaging. 2018;17:1536012118776068.
Ahmadzadehfar H, Aryana K, Pirayesh E, Farzanehfar S, Assadi M, Fallahi B, et al. The Iranian society of nuclear medicine practice guideline on radioligand therapy in metastatic castration-resistant prostate cancer using 177Lu-PSMA. Iran J Nucl Med. 2018;26:2–8.
Vorster M, Warwick J, Lawal IO, Du Toit P, Vangu M, Nyakale NE, et al. South African guidelines for receptor radioligand therapy (RLT) with Lu-177-PSMA in prostate cancer. S Afr J Surg. 2019;57:45–51.
Kratochwil C, Fendler WP, Eiber M, Baum R, Bozkurt MF, Czernin J, et al. EANM procedure guidelines for radionuclide therapy with 177Lu-labelled PSMA-ligands (177Lu-PSMA-RLT). Eur J Nucl Med Mol Imaging. 2019;46:2536–44.
Current K, Meyer C, Magyar CE, Mona CE, Almajano J, Slavik R, et al. Investigating PSMA-targeted radioligand therapy efficacy as a function of cellular PSMA levels and intratumoral PSMA heterogeneity. Clin Cancer Res. 2020;26:2946–55.
Giesel FL, Will L, Lawal I, Lengana T, Kratochwil C, Vorster M, et al. Intraindividual comparison of 18F-PSMA-1007 and 18F-DCFPyL PET/CT in the prospective evaluation of patients with newly diagnosed prostate carcinoma: a pilot study. J Nucl Med. 2018;59:1076–80.
Lawal I, Vorster M, Boshomane T, Ololade K, Ebenhan T, Sathekge M. Metastatic prostate carcinoma presenting as a superscan on 68Ga-PSMA PET/CT. Clin Nucl Med. 2015;40:755–6.
Haberkorn U, Giesel F, Morgenstern A, Kratochwil C. The future of radioligand therapy: α, β, or both? J Nucl Med. 2017;58:1017–8.
Kratochwil C, Bruchertseifer F, Rathke H, Bronzel M, Apostolidis C, Weichert W, et al. Targeted α-therapy of metastatic castration-resistant prostate cancer with 225Ac-PSMA-617: dosimetry estimate and empiric dose finding. J Nucl Med. 2017;58:1624–31.
Lawal IO, Ankrah AO, Mokgoro NP, Vorster M, Maes A, Sathekge MM. Diagnostic sensitivity of Tc-99m HYNIC PSMA SPECT/CT in prostate carcinoma: a comparative analysis with Ga-68 PSMA PET/CT. Prostate. 2017;77:1205–12.
Kratochwil C, Haberkorn U, Giesel FL. 225Ac-PSMA-617 for therapy of prostate cancer. Semin Nucl Med. 2020;50:133–40.
Hindié E, Zanotti-Fregonara P, Quinto MA, Morgat C, Champion C. Dose deposits from 90Y, 177Lu, 111In, and 161Tb in micrometastases of various sizes: implications for radiopharmaceutical therapy. J Nucl Med. 2016;57:759–64.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J Clin Oncol. 2016;34:1402–18.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–59.
Heinzel A, Boghos D, Mottaghy FM, Gaertner F, Essler M, von Mallek D, et al. 68Ga-PSMA PET/CT for monitoring response to 177Lu-PSMA-617 radioligand therapy in patients with metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2019;46:1054–62.
Grubmüller B, Senn D, Kramer G, Baltzer P, D’Andrea D, Grubmüller KH, et al. Response assessment using 68Ga-PSMA ligand PET in patients undergoing 177Lu-PSMA radioligand therapy for metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2019;46:1063–72.
Grubmüller B, Rasul S, Baltzer P, Fajkovic H, D’Andrea D, Berndl F, et al. Response assessment using [68 Ga]Ga-PSMA ligand PET in patients undergoing systemic therapy for metastatic castration-resistant prostate cancer. Prostate. 2020;80:74–82.
Fanti S, Goffin K, Hadaschik BA, Herrmann K, Maurer T, MacLennan S, et al. Consensus statements on PSMA PET/CT response assessment criteria in prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48:469–76.
Hofman MS, Lawrentschuk N, Francis RJ, Tang C, Vela I, Thomas P, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet. 2020;395:1208–16.
Lengana T, Lawal IO, Boshomane TG, Popoola GO, Mokoala KMG, Moshokoa E, et al. 68Ga-PSMA PET/CT replacing bone scan in the initial staging of skeletal metastasis in prostate cancer: a fait accompli? Clin Genitourin Cancer. 2018;16:392–401.
Emmett L, Crumbaker M, Ho B, Willowson K, Eu P, Ratnayake L, et al. Results of a prospective phase 2 pilot trial of 177Lu-PSMA-617 therapy for metastatic castration-resistant prostate cancer including imaging predictors of treatment response and patterns of progression. Clin Genitourin Cancer. 2019;17:15–22.
Lawal IO, Mokoala KMG, Mahapane J, Kleyhans J, Meckel M, Vorster M, et al. A prospective intra-individual comparison of [68Ga]Ga-PSMA-11 PET/CT, [68Ga]Ga-NODAGAZOL PET/CT, and [99mTc]Tc-MDP bone scintigraphy for radionuclide imaging of prostate cancer skeletal metastases. Eur J Nucl Med Mol Imaging. 2021;48:134–42.
Kratochwil C, Bruchertseifer F, Rathke H, Bronzel M, Apostolidis C, Weichert W, et al. Targeted α-therapy of metastatic castration-resistant prostate cancer with 225Ac-PSMA-617: dosimetry estimate and empiric dose finding. J Nucl Med. 2017;58:1624–31.
Kratochwil C, Bruchertseifer F, Rathke H, Hohenfellner M, Giesel FL, Haberkorn U, et al. Targeted α-therapy of metastatic castration-resistant prostate cancer with 225Ac-PSMA-617: swimmer-plot analysis suggests efficacy regarding duration of tumor control. J Nucl Med. 2018;59:795–802.
Sathekge M, Bruchertseifer F, Vorster M, Lawal IO, Knoesen O, Mahapane J, et al. Predictors of overall and disease-free survival in metastatic castration-resistant prostate cancer patients receiving 225Ac-PSMA-617 radioligand therapy. J Nucl Med. 2020;61:62–9.
Yadav MP, Ballal S, Sahoo RK, Tripathi M, Seth A, Bal C. Efficacy and safety of 225Ac-PSMA-617 targeted alpha therapy in metastatic castration-resistant prostate cancer patients. Theranostics. 2020;10:9364–77.
Satapathy S, Mittal BR, Sood A, Das CK, Singh SK, Mavuduru RS, et al. Health-related quality-of-life outcomes with Actinium-225-prostate-specific membrane antigen-617 therapy in patients with heavily pretreated metastatic castration-resistant prostate cancer. Indian J Nucl Med. 2020;35:299–304.
van der Doelen MJ, Mehra N, van Oort IM, Looijen-Salamon MG, Janssen MJR, et al. Clinical outcomes and molecular profiling of advanced metastatic castration-resistant prostate cancer patients treated with 225Ac-PSMA-617 targeted alpha-radiation therapy. Urol Oncol. 2020;S1078–1439(20)30631–1. https://doi.org/10.1016/j.urolonc.2020.12.002.
Sathekge MM, Bruchertseifer F, Lawal IO, Vorster M, Knoesen O, Lengana T, et al. Treatment of brain metastases of castration-resistant prostate cancer with 225Ac-PSMA-617. Eur J Nucl Med Mol Imaging. 2019;46:1756–7.
Maserumule LC, Mokoala KMG, Hlongwa KN, Ndlovu H, Reed JD, Ismail A, et al. Exceptional initial response of prostate cancer lung metastases to 225Ac-PSMA: a case report. Curr Problems Cancer Case Rep. 2021;3:100038.
Rathke H, Bruchertseifer F, Kratochwil C, Keller H, Giesel FL, Apostolidis C, et al. First patient exceeding 5-year complete remission after Ac-PSMA-TAT. Eur J Nucl Med Mol Imaging. 2021;48:311–2.
de Medeiros RB, Grigolon MV, Araújo TP, Srougi M. Metastatic castration-resistant prostate cancer (mCRPC) treated with 225Ac-PSMA-617. Case report Braj J Oncol. 2019;15:1–9.
Pelletier K, Côté G, Fallah-Rad N, John R, Kitchlu A. CKD after 225Ac-PSMA617 therapy in patients with metastatic prostate cancer. Kidney Int Rep. 2021;6:853–6.
Weineisen M, Schottelius M, Simecek J, Baum RP, Yildiz A, Beykan S, et al. 68Ga- and 177Lu-labeled PSMA I&T: optimization of a PSMA-targeted theranostic concept and first proof-of-concept human studies. J Nucl Med. 2015;56:1169–76.
Ilhan H, Gosewisch A, Böning G, Völter F, Zacherl M, Unterrainer M, et al. Response to 225Ac-PSMA-I&T after failure of long-term 177Lu-PSMA RLT in mCRPC. Eur J Nucl Med Mol Imaging. 2021;48:1262–3.
Zacherl MJ, Gildehaus FJ, Mittlmeier L, Böning G, Gosewisch A, Wenter V, et al. First clinical results for PSMA-targeted α-therapy using 225Ac-PSMA-I&T in advanced-mCRPC patients. J Nucl Med. 2021;62:669–74.
Feuerecker B, Tauber R, Knorr K, Heck M, Beheshti A, Seidl C, et al. Activity and adverse events of Actinium-225-PSMA-617 in advanced metastatic castration-resistant prostate cancer after failure of Lutetium-177-PSMA. Eur Urol. 2021;79:343–50.
Khreish F, Ebert N, Ries M, Maus S, Rosar F, Bohnenberger H, et al. 225Ac-PSMA-617/177Lu-PSMA-617 tandem therapy of metastatic castration-resistant prostate cancer: pilot experience. Eur J Nucl Med Mol Imaging. 2020;47:721–8.
Rosar F, Hau F, Bartholomä M, Maus S, Stemler T, Linxweiler J, et al. Molecular imaging and biochemical response assessment after a single cycle of [225Ac]Ac-PSMA-617/[177Lu]Lu-PSMA-617 tandem therapy in mCRPC patients who have progressed on [177Lu]Lu-PSMA-617 monotherapy. Theranostics. 2021;11:4050–60.
Barber TW, Singh A, Kulkarni HR, Niepsch K, Billah B, Baum RP. Clinical outcomes of (177)Lu-PSMA radioligand therapy in earlier and later phases of metastatic castration-resistant prostate cancer grouped by previous taxane chemotherapy. J Nucl Med. 2019;60:955–62.
Sathekge M, Bruchertseifer F, Knoesen O, Reyneke F, Lawal I, Lengana T, et al. 225Ac-PSMA-617 in chemotherapy-naive patients with advanced prostate cancer: a pilot study. Eur J Nucl Med Mol Imaging. 2019;46:129–38.
Kilnoshita Y, Kuratsukuri K, Landas S, et al. Expression of prostate-specific membrane antigen in normal and malignant human tissues. World J Surg. 2006;30:628–36.
Lawal IO, Bruchertseifer F, Vorster M, Morgenstern A, Sathekge MM. Prostate-specific membrane antigen-targeted endoradiotherapy in metastatic prostate cancer. Curr Opin Urol. 2020;30:98–105.
Satapathy S, Sood A, Das CK, Mittal BR. Evolving role of 225Ac-PSMA radioligand therapy in metastatic castration-resistant prostate cancer-a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2021. https://doi.org/10.1038/s41391-021-00349-w.
Rupp NJ, Umbricht CA, Pizzuto DA, Lenggenhager D, Töpfer A, Müller J, Muehlematter UJ, et al. First clinicopathologic evidence of a non-PSMA-related uptake mechanism for 68Ga-PSMA-11 in salivary glands. J Nucl Med. 2019;60:1270–6.
Yilmaz B, Nisli S, Ergul N, Gursu RU, Acikgoz O, Çermik TF. Effect of external cooling on 177Lu-PSMA uptake by the parotid glands. J Nucl Med. 2019;60:1388–93.
van Kalmthout LWM, Lam MGEH, de Keizer B, Krijger GC, Ververs TFT, de Roos R, et al. Impact of external cooling with icepacks on 68Ga-PSMA uptake in salivary glands. EJNMMI Res. 2018;8:56.
Kalidindi TM, Lee SG, Jou K, Chakraborty G, Skafida M, Tagawa ST, et al. A simple strategy to reduce the salivary gland and kidney uptake of PSMA-targeting small molecule radiopharmaceuticals. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-020-05150-w.
Rousseau E, Lau J, Kuo HT, Zhang Z, Merkens H, Hundal-Jabal N, et al. Monosodium glutamate reduces 68Ga-PSMA-11 uptake in salivary glands and kidneys in a preclinical prostate cancer model. J Nucl Med. 2018;59:1865–8.
Armstrong WR, Gafita A, Zhu S, Thin P, Nguyen K, Alano RM, et al. The impact of monosodium glutamate on 68Ga-PSMA-11 biodistribution in men with prostate cancer: a prospective randomized, controlled, imaging study. J Nucl Med. 2021 Jan 28:jnumed.120.257931. https://doi.org/10.2967/jnumed.120.257931.
Harsini S, Saprunoff H, Alden T, Mohammadi B, Wilson D, Bénard F. The effects of monosodium glutamate on PSMA radiotracer uptake in men with recurrent prostate cancer: a prospective, randomized, double-blind, placebo-controlled intraindividual imaging study. J Nucl Med. 2021;62:81–7.
Paganelli G, Sarnelli A, Severi S, Sansovini M, Belli ML, Monti M, et al. Dosimetry and safety of 177Lu PSMA-617 along with polyglutamate parotid gland protector: preliminary results in metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2020;47:3008–17.
Felber VB, Valentin MA, Wester HJ. Design of PSMA ligands with modifications at the inhibitor part: an approach to reduce the salivary gland uptake of radiolabeled PSMA inhibitors? EJNMMI Radiopharm Chem. 2021;6:10.
Baum RP, Langbein T, Singh A, Shahinfar M, Schuchardt C, Volk GF, et al. Injection of botulinum toxin for preventing salivary gland toxicity after PSMA radioligand therapy: an empirical proof of a promising concept. Nucl Med Mol Imaging. 2018;52:80–1.
Mohan V, Bruin NM, Tesselaar MET, de Boer JP, Vegt E, Hendrikx JJMA, et al. Muscarinic inhibition of salivary glands with glycopyrronium bromide does not reduce the uptake of PSMA-ligands or radioiodine. EJNMMI Res. 2021;11:25.
Rathke H, Kratochwil C, Hohenberger R, Giesel FL, Bruchertseifer F, Flechsig P, et al. Initial clinical experience performing sialendoscopy for salivary gland protection in patients undergoing 225Ac-PSMA-617 RLT. Eur J Nucl Med Mol Imaging. 2019;46:139–47.
Gaertner FC, Halabi K, Ahmadzadehfar H, Kürpig S, Eppard E, Kotsikopoulos C, et al. Uptake of PSMA-ligands in normal tissues is dependent on tumor load in patients with prostate cancer. Oncotarget. 2017;8:55094–103.
Tranel J, Feng FY, James SS, Hope TA. Effect of microdistribution of alpha and beta-emitters in targeted radionuclide therapies on delivered absorbed dose in a GATE model of bone marrow. Phys Med Biol. 2021;66:035016.
Stuparu AD, Capri JR, Meyer C, Le TM, Evans-Axelsson SL, Current K, et al. Mechanisms of Resistance to Prostate-Specific Membrane Antigen-Targeted Radioligand Therapy in a Mouse Model of Prostate Cancer. J Nucl Med. 2020;120.256263. https://doi.org/10.2967/jnumed.120.256263.
Kratochwil C, Giesel FL, Heussel CP, Kazdal D, Endris V, Nientiedt C, et al. Patients resistant against PSMA-targeting α-radiation therapy often harbor mutations in DNA damage-repair-associated genes. J Nucl Med. 2020;61:683–8.
de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for metastatic castration-resistant prostate cancer. N Engl J Med. 2020;382:2091–102.
Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science. 2015;348:69–74.
Kgatle MM, Boshomane TMG, Lawal IO, Mokoala KMG, Mokgoro NP, Lourens N, et al. Immune checkpoints, inhibitor and radionuclides in prostate cancer: promising combinatorial therapy approach. Int J Mol Sci. 2021;22:4109.
Czernin J, Current K, Mona CE, Nyiranshuti L, Hikmat F, Radu CG, et al. Immune-checkpoint blockade enhances 225Ac-PSMA617 efficacy in a mouse model of prostate cancer. J Nucl Med. 2021;62:228–31.
Morgenstern A, Apostolidis C, Bruchertseifer F. Supply and clinical application of Actinium-225 and Bismuth-213. Semin Nucl Med. 2020;50:119–23.
Acknowledgements
We thank our patients we have entrusted with the care of their disease. It is by their sacrifice that we have learnt about the safety and efficacy of targeted alpha therapy in metastatic castration-resistant prostate cancer.
Author information
Authors and Affiliations
Contributions
All authors contributed to content selection and writing of the manuscripts. All authors read and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - Genitourinary
The original online version of this article was revised: The authors request that they need to incorporate the below correction in their article in order to fully credit the original authors of the cited reference. To replace the sentence: “Figure 1 shows the nuclear recoil effect during α-decay within radioligand for TAT.” With the sentence: “Figure 1 from the paper by Roscher and colleagues shows the nuclear recoil effect during α-decay within radioligand for TAT [37].” The original article has been corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sathekge, M.M., Bruchertseifer, F., Vorster, M. et al. Global experience with PSMA-based alpha therapy in prostate cancer. Eur J Nucl Med Mol Imaging 49, 30–46 (2021). https://doi.org/10.1007/s00259-021-05434-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05434-9