Abstract
Background
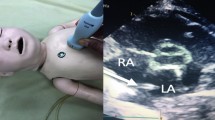
Chest radiography after peripherally inserted central catheter insertion in infants is the reference standard method for verifying catheter tip position. The utilisation of ultrasound (US) for catheter placement confirmation in the neonatal and paediatric population has been the focus of many recent studies.
Objective
In this systematic review we investigated the diagnostic accuracy of US for peripherally inserted central catheter tip confirmation in infants in the neonatal intensive care unit (NICU)
Materials and methods
We conducted a systematic literature search of multiple databases. The study selection yielded eight articles, all of which had acceptable quality and homogeneity for inclusion in the meta-analysis. Sensitivity and specificity values were reported together with their respective 95% confidence intervals (CI).
Results
After synthesising the eligible studies, we found that US had a sensitivity of 95.2% (95% CI 91.9–97.4%) and specificity of 71.4% (95% CI 59.4–81.6%) for confirming catheter tip position.
Conclusion
Analyses indicated that US is an excellent imaging test for localising catheter tip position in the NICU when compared to radiography. Ultrasonography is a sensitive, specific and timely imaging modality for confirming PICC tip position. In cases where US is unable to locate malpositioned PICC tips, a chest or combined chest–abdominal radiograph should be performed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripherally inserted central catheters (PICC) are ubiquitous in the neonatal intensive care unit (NICU) and are used to facilitate administration of total parenteral nutrition in low-birth-weight infants, and long-term administration of intravenous antibiotics [1]. The establishment of long-term venous access is also advantageous because it averts the need for repetitive catheterisation, thereby reducing pain and risk of infection for the infant whilst limiting excessive stimuli and extended time away from dedicated nursing care [2].
The use of PICCs in clinical practice is associated with various complications. Most of these complications are associated with malpositioning or migration of the catheter tip [3,4,5]. If the catheter tip is incorrectly placed, or migrates following insertion, pericardial effusion, thrombosis, infection, perforation, arrhythmia, cardiac tamponade, heart valve damage and patient discomfort can occur [6, 7].
Accurate PICC tip positioning is essential to minimise the risk of complications. The international standard for upper body inserted PICC tip position is at the caval–atrial junction at the lower third of the superior vena cava [8]. For PICCs inserted via the lower limb, the tip should be within the upper inferior vena cava between the 9th and 11th thoracic vertebrae [9, 10]. PICC tip localisation and confirmation can be achieved through myriad diagnostic imaging modalities. Verification of the catheter tip in infants is typically undertaken using the reference standard for PICC confirmation, an anteroposterior chest radiograph for upper-body-deployed PICCs and a combined chest–abdominal radiograph for PICCs deployed via the lower limb [11, 12].
There is evidence to suggest that chest radiography alone is not entirely accurate at identifying intra-atrial tip position [13, 14]. Additionally, it is often difficult to position the neonate for an optimum radiographic image without geometric or movement artefact. Chest radiography also provides only a static image of PICC position. Arm movements have been shown to influence the position of the PICC, so a radiograph captures the tip position in respect to the limb position of the neonate at the time of exposure and might not be entirely representative of the long-term position [15, 16].
Repositioning of misplaced PICC lines requires supplementary radiographs to re-assess tip position. This exposes the infant to additional ionising radiation repeatedly, until the catheter tip is in the appropriate position. Neonatal and paediatric populations are considerably more susceptible to ionising radiation because the rate at which their cells undergo mitosis is more rapid than that observed in adult populations [17]. Increased radiosensitivity, greater mitotic activity and a protracted period for consequences to manifest mean that the risk of radiation-induced cancer per unit of dose is 2–3 times higher for preterm infants than the average population [18]. Reduction in the risk of radiation-associated comorbidities can be achieved by limiting unnecessary radiographs by employing alternative methods to achieve similar diagnostic information or conclusions [19,20,21].
Bedside radiographic imaging in the NICU can be challenging for radiographers because the environment can make it impractical to comply with standard examination protocols. Neonates are unable to control their movements, making positioning accuracy difficult to accomplish. It is often the case that various lines, tubes and devices overlie the area of interest, interfering with image quality and diagnosis [22].
Neonatal intensive care unit staff are often required to be within 2 m of the X-ray source to hold the neonate, with their hands sometimes inadvertently being caught within the primary X-ray beam. A study by Russell et al. [23] showed that 15–40% of mobile radiographic examinations conducted in the NICU had at least one adult finger visible on the resultant image. In addition to direct radiation exposure, staff and patients in the NICU may also be exposed to secondary scatter radiation. Employing alternative imaging modalities that avoid the use of ionising radiation, such as US, is becoming increasingly popular, particularly for routine checks of catheter or tube positioning [24,25,26].
Technological advancements have expanded the role that US can play in the critical care setting through improved image quality and accessibility. Advantages of US include real-time assessment and limited handling of critically ill infants. Evidence shows that minimal training is required to reliably perform quantitative US [27]. Additionally, clinical reporting can be performed by the sonographer at the time of scanning, which can reduce report turnaround time. However, US does carry a higher infection control risk and therefore good basic hygiene standards are essential [28].
Previous systematic reviews [29, 30] have shown the success of US in localising central venous catheters in comparison to the reference standard (radiography), but these studies have not investigated the accuracy of US in a neonatal population. The aim of this systematic review was to identify, critically appraise and assess the sensitivity and specificity of US in confirming PICC tip position in infants on the NICU.
Materials and methods
Using the Cochrane protocol, we conducted and report a systematic review (CRD42020223684) in adherence with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) criteria/guidelines [31].
Search strategy
We searched Embase, PubMed, CINAHL and MEDLINE (Ovid) in February 2021 and included eligible publications between January 2001 and February 2021. We also performed a grey literature search using OpenGrey and Google Scholar. We examined the bibliographies and reference lists of the identified studies for relevance and to identify additional studies. Two authors (S.C.D., N.M.B.), who were final year master’s-level student radiographers, independently searched the databases by applying a set of pre-determined search terms as described in Table 1.
Study selection
Two authors (S.C.D., N.M.B.) independently screened titles and abstracts of the returned search results to determine applicability for inclusion. Articles were included if they were published in English during the last 10 years and assessed the diagnostic accuracy of US for PICC tip confirmation in infants in the NICU. References of the chosen studies were exported to a bibliographic database through EndNote [32] and duplicates were automatically removed. All studies eligible for inclusion or classified as “unclear” based on the title or abstract were subjected to a full-text review by either author. Full texts were independently assessed for eligibility using the pre-set inclusion and exclusion criteria. Discrepancies between the two authors were resolved by consensus discussion.
Risk of bias assessment
We assessed the internal validity of the included studies using the Quality Assessment of Diagnostic Accuracy Studies-2 tool (QUADAS-2) [33]. The quality assessment of homogeneity was completed by both authors, independently. The tool assesses bias across four separate domains: patient selection, index test, reference test, and flow and timing. Concerns regarding the applicability of the study were judged dependent on whether risk of bias was low, high or unclear across these four domains.
Data abstraction
Two authors (S.C.D., N.M.B.) independently extracted data from articles meeting criteria for final inclusion. Any disagreement between the authors was mediated through consensus discussion. The designed data extraction tool collected elements relating to various aspects of the studies such as patient demographics, index test characteristics, methods and outcomes, study characteristics and diagnostic accuracy measurements. Extraction also included an assessment of the role and type of US within each study, for example where US was used to provide real-time intra-procedural guidance by the operator or whether US was used to evaluate a previously implanted PICC. Where available, we also recorded US technique, e.g., transthoracic, transoesophageal. We used Microsoft Excel (Microsoft Inc., Redmond, WA) for data management.
Data analysis
The meta-analysis was conducted using RevMan 5 [34]. The diagnostic accuracy measures used in the analyses were sensitivity, specificity and positive and negative predictive values. A 2 × 2 contingency table was derived to represent the pooled diagnostic accuracy measurements across all included studies. Sensitivity and specificity figures of individual studies were summarised and compared using a forest plot. Sensitivity and specificity values are presented together with their corresponding 95% confidence intervals (CI). The diagnostic accuracy of US in assessing PICC tip location is summarised using the receiver operating characteristic curve (ROC). We constructed an ROC for each study as well as an ROC to represent the pooled diagnostic accuracy data.
Results
The PRISMA flowchart (Fig. 1) summarises the results of the search and review process. The search strategy yielded 120 studies following the removal of duplicates. We screened the abstracts and titles of these 120 papers and completed a full-text review of 15 studies. Eight papers were deemed eligible for inclusion. Potential studies for inclusion in this systematic review were appraised using the modified QUADAS-2 tool [33] (Table 2; [5, 35,36,37,38,39,40,41]). All eight studies were included because they had an overall low risk of bias.
Details of the study characteristics for all eight papers are detailed in Table 3 [5, 35,36,37,38,39,40,41]. Across the eight studies, 421 infants received a PICC line and 341 US scans were conducted. All eight studies reported the gestation for those neonates included, with a mean gestation for the eight studies of 38.6 (range 25.4 to 35.0) weeks. The mean birth weight recorded for included neonates was 1,581.1 (range 525.0 to 3,302.0) grams. All infants included in the study were in-patients in the NICU.
Five studies detailed the PICC insertion site, with 215 (59.9%) in the upper limb and 103 (28.7%) in the lower limb; 38 (10.6%) were superficial temporally located and three (0.8%) were auricle. Three studies (n = 64) did not report the exact insertion site of the PICC lines, but each of the three studies reported inclusion of both upper- and lower-extremity PICC line insertions [3, 21, 35].
All included studies reported diagnostic accuracy of US in relation to the reference standard. All included studies used radiography as the reference standard. The reference standard in six studies was solely chest radiography. In two studies the reference standard was both supine chest and abdominal radiography [36, 37].
Six studies provided details regarding the qualification and level of experience of the US operator involved (Table 3). The frequencies, brand and type of the US probes and machines used in the eight studies are reported in Table 4 [5, 35,36,37,38,39,40,41].
All included studies acquired the reference standard image using a mobile radiography machine, although they did not specify the machine manufacture or detector type. All studies had a radiologist report the radiographs, except one, in which a neonatologist reported the radiographic images [37].
Four studies documented that the reference test was reported incorrectly. These erroneous radiographic reports were ultimately corrected following the US examination, which demonstrated a more accurate tip position [36, 38,39,40]. Radiographic misinterpretations in these four studies were a mixture of false reports of malposition and false reports of optimum position. Diagnostic accuracy measurements from included studies are summarised in Table 5 [5, 35,36,37,38,39,40,41].
The estimated sensitivity and specificity for US were 95.2% (95% CI: 91.9–97.4%) and 71.4% (CI: 59.4–81.6%), respectively. The pooled positive likelihood ratio was 3.3 (95% CI: 2.3–4.8) and the negative likelihood ratio was 0.07 (95% CI: 0.04–0.12). The positive predictive value and the negative predictive value were 92.8% (95% CI: 89.9–94.9) and 6.7% (0.04–12.0), respectively. Figure 2 shows the forest plot of the overall odds ratios. The ROC curve for the pooled diagnostic accuracy of US across all eight studies indicated an acceptable overall accuracy (area under the curve [AUC] = 0.83) (Fig. 3).
Receiver operating curve for pooled diagnostic accuracy indices. Area under the curve (AUC) = 0.83 (95% confidence interval: 0.79–0.87). The solid black line indicates a theoretical diagnostic test with a random performance level. The dotted black line indicates the performance of ultrasound in the confirmation of peripherally inserted central catheter placement
Discussion
Mobile radiographic imaging is the modality employed in the NICU for confirming PICC tip location. An imaging pathway free from ionising radiation, such as US, is a contemporary and novel approach to confirming the position of the PICC line tip in a neonatal population. By acknowledging the limitations of conventional radiography, it is reasonable to suggest that questions might soon be raised regarding the preferred primary imaging approach. This systematic review considers whether US is a viable alternative to mobile radiography in the localisation of the PICC line tip in a neonatal population.
Eight studies were eligible for inclusion in this review and meta-analysis. We calculated a pooled sensitivity of 95.2% (95% CI: 91.9–97.4%). The specificity values across all eight studies were variable because of misinterpretations made by the reference standard, lowering the pooled specificity value to 71.4% (95% CI: 59.4–81.6%). These results suggest US to be an excellent test for the localisation of the correctly positioned PICC line tip; however, it is less than perfect for identifying a misplaced or migrated PICC tip.
The low specificity can be explained by referencing the studies by Jain et al. [39] and Shabeer et al. [40]. Jain et al. [39] reported sensitivity and specificity values of 60% (95% CI 41.6–81.1) and 58% (95% 34.1–73.5%), respectively. Radiography inaccurately interpreted 4/11 misplaced PICC tips as appropriately placed, evidently impacting the false-negative rate, which had a negative impact on the sensitivity value. Furthermore, radiography incorrectly indicated that five of the correctly positioned PICC line tips were malpositioned, subsequently elevating the false-positive rate and negatively affecting the specificity. The study by Shabeer et al. [40] had a notably lower sensitivity value of 47.8% (95% CI 35.8–60.1%) in comparison to the other studies included in the analysis. The specificity value reported by Shabeer et al. was similar to that reported in the other studies (82.4% [95% CI 61.7–93.1%]). The limited specificity of US in detecting the PICC line tips in the study by Shabeer et al. [40] was also attributed to an imperfect reference standard. Chan et al. [42] acknowledged the variability amongst radiologists regarding the cavo-atrial junction, which would explain the misjudgements made on the reports in the studies by Jain et al. [39] and Shabeer et al. [40]. Taking the limitations of the reference standard into consideration, had both these studies been omitted from the meta-analysis, the pooled sensitivity and specificity values for the remaining seven studies would have been 97.5% and 91.4%, respectively.
The pervasiveness of PICC tip malposition within our systematic review aligns with that reported in the published literature in respect to the general population (10–53%) [43, 44]. Repositioning of these malpositioned or migrated catheter tips can be achieved under US guidance, avoiding the need for repeated radiographic imaging to reassess catheter tip location. This advantage of US has the potential to negate additional radiation exposure to the neonate [2].
Whilst our systematic review investigates the pooled diagnostic accuracy measurements of US as a confirmatory method for PICC line tip position in the neonatal population, our results align with recent publications exploring the accuracy of US for various other catheter and tube types. In 2017, a meta-analysis by Ablordeppey et al. [30] reported a pooled sensitivity of 82% (77–86%) and specificity of 98% (97–99%) of US as a confirmatory tool for central venous catheters. Similarly, a systematic review and meta-analysis published by Smit et al. [29] showed US to be an excellent alternative for the localisation of misplaced or migrated central venous catheter tips, reporting a pooled sensitivity and specificity of 68.2% (54.4–79.4%) and 98.9% (97.8–99.5%), respectively. The low sensitivity value was explained by an incorrect reference standard, further encouraging investigation into the accuracy of the reference standard chest radiography.
Our review extracted data in relation to the time taken to confirm PICC location using US. Four of the eight studies did not provide any data for the time taken to achieve PICC confirmation using US; however, all four of these studies reported that the US was faster than the reference standard. The remaining four studies reported time values. Three reported a scan time of less than 15 min [35, 39, 41]. The fourth study recorded a mean scan time of 60 min, which was considerably less than the time taken for conventional radiography (136 min) [40]. This element of the data extraction confirmed that US is a faster imaging modality than radiography for confirming catheter tip position in the neonatal population. In addition to this, US provides a real-time assessment, negating the time traditionally required for radiology reporting of the radiographic images.
Ultrasound quality is highly operator-dependent, making it necessary that US providers are appropriately trained. The lack of implementation of US as a contemporary imaging modality within the NICU setting is often a result of the lack of availability of appropriately qualified US staff [45]. The level of training of US operators varied across all eight studies included in our review. Six of the eight studies reported the qualification and training of the US operators. Despite varying levels of operator experience across all eight studies, diagnostic accuracy measurements did not vary significantly.
Limitations
The quality of US examinations is highly operator-dependent and sonographic scans can be subject to interpretation bias. Errors in US examinations can occur during the study, in the form of bias and at the level of the individual operator through misinterpretation of clinical evidence, resulting in an erroneous diagnosis and affecting the clinical management of the individual patient. Six studies included in the review reported the qualifications and training received by the US practitioner. However, two studies did not report this information, which might have impacted on diagnostic accuracy.
Within recent years, US technology has been making considerable advances in the areas of image quality, image acquisition and physics [46]. Application of a language restriction to include only studies published in the English language might have limited our review. Considering the advancements in US science it is possible that additional research was published following the completion of our literature search. However, we are not aware of any new research published since execution of our data search and it is unlikely that a single additional publication would significantly impact our findings.
It is likely that the US visualisation of catheter tips and relevant anatomy varies depending on the deployment site. Anecdotally, it is likely to be easier to obtain a longitudinal view of the inferior vena cava and the inferior cavo-atrial junction with clear determination of the catheter tip when compared to obtaining longitudinal views of the superior vena cava for thoracic cage and pulmonary artefacts. It is therefore possible that if this review contained more lower-body PICCs, the sensitivity and specificity rates might be artificially higher. Sufficient data are not available to prove or disprove this within the current review; further work is needed to assess diagnostic performance by deployment site.
Implications for practice
Ultrasound is clinically practical for confirming PICC line tip position in the NICU. In cases where US is unable to locate malpositioned PICC tips, chest radiography should be performed. Employing US as the reference standard for PICC tip confirmation in the NICU setting would have many advantages. The ability to provide real-time assessment and guidance for repositioning whilst avoiding the use of ionising radiation indicates it is a safe and efficient alternative to conventional radiography. Albeit there are advantages to sonography, particularly in relation to a neonatal population, it is important to acknowledge the potential limitations of US. US is highly operator-dependent [47]. Adoption of bedside US in neonatal practice is gaining popularity; however, widespread implementation is hindered by the lack of unified guidelines and training for US use in neonatal critical care [45].
Conclusion
Our systematic review and meta-analysis provide evidence that US is sensitive and specific for confirming PICC line placement in the NICU. Our analysis estimated a pooled sensitivity of 95.2% (95% CI: 91.9–97.4%) and a pooled specificity of 71.4% (95% CI: 59.4–81.6%). In cases where US fails to locate misplaced PICC tips, radiography should be performed.
References
Yu X, Yue S, Wang M et al (2018) Risk factors related to peripherally inserted central venous catheter nonselective removal in neonates. Biomed Res Int 2018:3769376
Katheria AC, Fleming SE, Kim JH (2013) A randomized controlled trial of ultrasound-guided peripherally inserted central catheters compared with standard radiograph in neonates. J Perinatol 33:791–794
Jain A, Deshpande P, Shah P (2013) Peripherally inserted central catheter tip position and risk of associated complications in neonates. J Perinatol 33:307–312
Imakiire Y, Yanaru T, Kumano H et al (2018) Malposition of peripherally inserted central catheter into the right inferior thyroid vein: a case report. Am J Case Rep 19:491–493
Ren XL, Li HL, Liu J et al (2021) Ultrasound to localize the peripherally inserted central catheter tip position in newborn infants. Am J Perinatol 38:122–125
Sharma D, Farahbakhsh N, Tabatabaii SA (2019) Role of ultrasound for central catheter tip localization in neonates: a review of the current evidence. J Matern Fetal Neonatal Med 32:2429–2437
Kearns PJ, Coleman S, Wehner JH (1996) Complications of long arm-catheters: a randomized trial of central vs peripheral tip location. J Parenter Enteral Nutr 20:20–24
Gao Y, Liu Y, Zhang H et al (2018) The safety and accuracy of ECG-guided PICC tip position verification applied in patients with atrial fibrillation. Ther Clin Risk Manag 14:1075–1081
Racadio JM, Doellman DA, Johnson ND et al (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107:E28
Mason Wyckoff M, Sharp E (2015) Peripherally inserted central catheters: PICC guidelines for practice. National Association of Neonatal Nurses, Chicago
Sneath N (2010) Are supine chest and abdominal radiographs the best way to confirm PICC placement in neonates? Neonatal Netw 29:23–35
Hostetter R, Nakasawa N, Tompkins K, Hill B (2010) Precision in central venous catheter tip placement: a review of the literature. J Assoc Vasc Acc 15:112–125
Ohki Y, Tabata M, Kuwashima M et al (2000) Ultrasonographic detection of very thin percutaneous central venous catheter in neonates. Acta Paediatr 89:1381–1384
Blans MJ, Endeman H, Bosch FH (2016) The use of ultrasound during and after central venous catheter insertion versus conventional chest X-ray after insertion of a central venous catheter. Neth J Med 74:353–357
Nadroo AM, Glass RB, Lin J et al (2002) Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics 110:131–136
Connolly B, Amaral J, Walsh S et al (2006) Influence of arm movement on central tip location of peripherally inserted central catheters (PICCS). Pediatr Radiol 36:845–850
Bahreyni Toosi M, Malekzadeh M (2012) Radiation dose to newborns in neonatal intensive care units. Iran J Radiol 9:145–149
Linet MS, Kim KP, Rajaraman P (2009) Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol 39:S4-26
Livingstone RS, Keshava SN (2011) Technical note: reduction of radiation dose using ultrasound guidance during transjugular intrahepatic portosystemic shunt procedure. Indian J Radiol Imaging 21:13–14
Sheyn DD, Racadio JM, Ying J et al (2008) Efficacy of a radiation safety education initiative in reducing radiation exposure in the pediatric IR suite. Pediatr Radiol 38:669–674
Motz P, Do J, Lam T et al (2020) Decreasing radiographs in neonates through targeted quality improvement interventions. J Perinatol 40:330–336
Edison P, Chang PS, Toh GH et al (2017) Reducing radiation hazard opportunities in neonatal unit: quality improvement in radiation safety practices. BMJ Open Qual 6:e000128
Russell J, Burbridge BE, Duncan MD, Tynan J (2013) Adult fingers visualized on neonatal intensive care unit chest radiographs: what you don’t see. Can Assoc Radiol J 64:236–239
Chowdhry R, Dangman B, Pinheiro JM (2015) The concordance of ultrasound technique versus X-ray to confirm endotracheal tube position in neonates. J Perinatol 35:481–484
Wallbridge P, Steinfort D, Tay TR et al (2018) Diagnostic chest ultrasound for acute respiratory failure. Respir Med 141:26–36
Miller LE, Stoller JZ, Fraga MV (2020) Point-of-care ultrasound in the neonatal ICU. Curr Opin Pediatr 32:216–227
Zaidman CM, Wu JS, Wilder S et al (2014) Minimal training is required to reliably perform quantitative ultrasound of muscle. Muscle Nerve 50:124–128
Nyhsen CM, Humphreys H, Koerner RJ et al (2017) Infection prevention and control in ultrasound — best practice recommendations from the European Society of Radiology Ultrasound Working Group. Insights Imaging 8:523–535
Smit JM, Raadsen R, Blans MJ et al (2018) Bedside ultrasound to detect central venous catheter misplacement and associated iatrogenic complications: a systematic review and meta-analysis. Crit Care 22:65
Ablordeppey EA, Drewry AM, Beyer AB et al (2017) Diagnostic accuracy of central venous catheter confirmation by bedside ultrasound versus chest radiography in critically ill patients: a systematic review and meta-analysis. Crit Care Med 45:715–724
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 18:e1003583
Hupe M (2019) EndNote X9. J Electron Resour Med Libr 16:117–119
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Deeks J, Higgins J (2010) Statistical algorithms in Review Manager 5. Statistical Methods Group of the Cochrane Collaboration. https://training.cochrane.org/handbook/archive/v6.2/statistical-methods-revman5. Accessed 21 Mar 2022
Saul D, Ajayi S, Schutzman DL, Horrow MM (2016) Sonography for complete evaluation of neonatal intensive care unit central support devices. J Ultrasound Med 35:1465–1473
Kadivar M, Mosayebi Z, Ghaemi O et al (2020) Ultrasound and radiography evaluation of the tips of peripherally inserted central catheters in neonates admitted to the NICU. Iran J Pediatr 30:e108416
Telang N, Sharma D, Pratap OT et al (2017) Use of real-time ultrasound for locating tip position in neonates undergoing peripherally inserted central catheter insertion: a pilot study. Indian J Med Res 145:373–376
Motz P, Von Saint Andre Von Arnim A, Iyer RS et al (2019) Point-of-care ultrasound for peripherally inserted central catheter monitoring: a pilot study. J Perinat Med 47:991–996
Jain A, McNamara PJ, Ng E, El-Khuffash A (2012) The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol 29:101–106
Shabeer MP, Abiramalatha T, Gibikote S et al (2021) Bedside sonography performed by neonatology residents to confirm central vascular catheter position in neonates — a prospective diagnostic evaluation study. J Neonatal Perinatal Med 14:101–107
Motz P, von Saint Andre von Arnim A, Likes M et al (2019) Limited ultrasound protocol for upper extremity peripherally inserted central catheter monitoring: a pilot study in the neonatal intensive care unit. J Ultrasound Med 38:1341–1347
Chan TY, England A, Meredith SM, McWilliams RG (2016) Radiologist variability in assessing the position of the cavoatrial junction on chest radiographs. Br J Radiol 89:20150965
Trerotola SO, Thompson S, Chittams J, Vierregger KS (2007) Analysis of tip malposition and correction in peripherally inserted central catheters placed at bedside by a dedicated nursing team. J Vasc Interv Radiol 18:513–518
Glauser F, Breault S, Rigamonti F et al (2017) Tip malposition of peripherally inserted central catheters: a prospective randomized controlled trial to compare bedside insertion to fluoroscopically guided placement. Eur Radiol 27:2843–2849
Singh S, Venkatesh HA, Swamy R, Nagesh NK (2020) Ultrasound guided confirmation of tip of peripherally inserted central catheter in neonates. Indian Pediatr 57:858–859
Sassaroli E, Crake C, Scorza A et al (2019) Image quality evaluation of ultrasound imaging systems: advanced b-modes. J Appl Clin Med Phys 20:115–124
Farina R, Sparano A (2012) Errors in sonography. In: Romano L, Pinto A (eds) Errors in radiology. Springer, New York, pp 79–85
Funding
Open Access funding was provided by the IReL Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doyle, S.C., Bergin, N.M., Young, R. et al. Diagnostic accuracy of ultrasound for localising peripherally inserted central catheter tips in infants in the neonatal intensive care unit: a systematic review and meta-analysis. Pediatr Radiol 52, 2421–2430 (2022). https://doi.org/10.1007/s00247-022-05379-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05379-7