Abstract
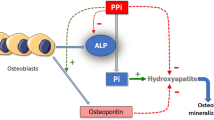
Nephrolithiasis is a result of formation and retention of crystals within the kidneys. The driving force behind crystal formation is urinary supersaturation with respect to the stone-forming salts, which means that crystals form when the concentrations of participating ions are higher than the thermodynamic solubility for that salt. Levels of supersaturation are kept low and under control by proper functioning of a variety of cells including those that line the renal tubules. It is our hypothesis that crystal deposition, i.e., formation and retention in the kidneys, is a result of impaired cellular function, which may be intrinsic and inherent or triggered by external stimuli and challenges. Cellular impairment or dysfunction affects the supersaturation, by influencing the excretion of participating ions such as calcium, oxalate and citrate and causing hypercalciuria, hyperoxaluria or hypocitraturia. The production and excretion of macromolecular promoters and inhibitors of crystallization is also dependent upon proper functioning of the renal epithelial cells. Insufficient or ineffective crystallization modulators such as osteopontin, Tamm-Horsfall protein, bikunin, etc. are most likely produced by the impaired cells.

Similar content being viewed by others
References
Stamatelou KK, Francis MF, Jones CA, Curhan GC (2003) Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int 63:1817–1823. doi:10.1046/j.1523-1755.2003.00917.x
Randall A (1940) The etiology of primary renal calculus. Int Abstr Surg 71:209–240
Finlayson B, Reid S (1978) The expectation of free or fixed particles in urinary stone disease. Invest Urol 15:442–448
Kok DJ, Khan SR (1994) Calcium oxalate nephrolithiasis, a free or fixed particle disease. Kidney Int 46:847–854. doi:10.1038/ki.1994.341
Kavanagh JP (1995) Calcium oxalate crystallization in vitro. In: Khan SR (ed) Calcium oxalate in biological systems. CRC Press, Boca Raton, p 1
Robertson WG, Peacock M, Nordin BEC (1968) Activity products in stone forming and non-stone forming urine. Clin Sci 34:579–594
Khan SR, Kok DJ (2004) Modulators of urinary stone formation. Front Biosci 9:1450–1480. doi:10.2741/1347
Vezzoli G, Soldati L, Gambaro G (2008) Update on primary hypercalciuria from a genetic perspective. J Urol 179:1676–1682. doi:10.1016/j.juro.2008.01.011
Geng W, Wang Z, Zhang J, Reed BY, Pak CY, Moe OW (2005) Cloning and characterization of the human soluble adenylyl cyclase. Am J Physiol Cell Physiol 288:C1305–C1311. doi:10.1152/ajpcell.00584.2004
Pastor-Soler N, Beaulieu V, Litvin TN, Da Silva N, Chen Y, Brown D, Buck J, Levin LR, Breton S (2003) Bicarbonate-regulated adenylyl cyclase (sAC) is a sensor that regulates pH-dependent V-ATPase recycling. J Biol Chem 278:49523–49529. doi:10.1074/jbc.M309543200
Reed BY, Heller HJ, Gitomer WL, Pak CY (1999) Mapping a gene defect in absorptive hypercalciuria to chromosome 1q23.3-q24. J Clin Endocrinol Metab 84:3907–3911. doi:10.1210/jc.84.11.3907
Reed BY, Gitomer WL, Heller HJ, Hsu MC, Lemke M, Padalino P et al (2002) Identification and characterization of a gene with base substitutions associated with the absorptive hypercalciuria phenotype and low spine bone density. J Clin Endocrinol Metab 87:1476–1481. doi:10.1210/jc.87.4.1476
Bushinsky DA (1999) Genetic hypercalciuric stone-forming rats. Curr Opin Nephrol Hypertens 8:479–489. doi:10.1097/00041552-199907000-00013
Khullar M, Relan V, Singh SK (2006) VDR gene and urinary calcium excretion in nephrolithiasis. Kidney Int 69:943–951. doi:10.1038/sj.ki.5000176
Recker F, Rubben H, Bex A, Constantinides C (1989) Morphological changes following ESWL in the rat kidney. Urol Res 17:229–233
Relan V, Khullar M, Singh SK, Sharma SK (2004) Association of vitamin D receptor genotypes with calcium excretion in nephrolithiatic subjects in northern India. Urol Res 32:236–241. doi:10.1007/s00240-004-0414-x
Rendina D, Mossetti G, Viceconti R, Sorrentino M, Castaldo R, Manno G et al (2004) Association between vitamin D receptor gene polymorphisms and fasting idiopathic hypercalciuria in recurrent stone-forming patients. Urology 64:838–842. doi:10.1016/j.urology.2004.05.013
Soylemezoglu O, Ozkaya O, Gonen S, Misirlioglu M, Kalman S, Buyan N (2004) Vitamin D receptor gene polymorphism in hypercalciuric children. Pediatr Nephrol 19:724–730. doi:10.1007/s00467-004-1490-4
Bushinsky DA, Asplin JR, Grynpass MD et al (2002) Calcium oxalate stone formation in genetic hypercalciuric stone-forming rats. Kidney Int 61:975–987. doi:10.1046/j.1523-1755.2002.00190.x
Zerwekh JE, Hughes MR, Reed BY, Breslau NA, Heller HJ, Lemke M et al (1995) Evidence for normal vitamin D receptor messenger ribonucleic acid and genotype in absorptive hypercalciuria. J Clin Endocrinol Metab 80:2960–2965. doi:10.1210/jc.80.10.2960
Scott P, Ouimet D, Valiquette L, Guay G, Proulx Y, Trouve ML et al (1999) Suggestive evidence for a susceptibility gene near the vitamin D receptor locus in idiopathic calcium stone formation. J Am Soc Nephrol 10:1007–1013
Muller D, Hoenderop JG, Vennekens R, Eggert P, Harangi F, Mehes K et al (2002) Epithelial Ca(2−) channel (ECAC1) in autosomal dominant idiopathic hypercalciuria. Nephrol Dial Transplant 17:1614–1621. doi:10.1093/ndt/17.9.1614
Bid HK, Kumar A, Kapoor R, Mittal RD (2005) Association of vitamin D receptor- gene (FokI) polymorphism with calcium oxalate nephrolithiasis. J Endourol 19:111–115. doi:10.1089/end.2005.19.111
Chen W-C, Chen H-Y, Lu H-F, Hsu C-D, Tsai F-J (2001) Association of the vitamin D receptor gene start codon Fok I polymorphism with calcium oxalate stone disease. BJU Int 87:168–174. doi:10.1046/j.1464-410x.2001.02074.x
Nishijima S, Sugaya K, Naito A, Morozumi M, Hatano T, Ogawa Y (2002) Association of vitamin D receptor gene polymorphism with urolithiasis. J Urol 167:2188–2195. doi:10.1016/S0022-5347(05)65126-9
Ozkaya O, Soylemezoglu O, Misirlioglu M, Gonen S, Buyan N, Hasanoglu E (2003) Polymorphisms in the vitamin D receptor gene and the risk of calcium nephrolithiasis in children. Eur Urol 44:150–154. doi:10.1016/S0302-2838(03)00206-9
Devuyst O, Pirson Y (2007) Genetics of hypercalciuric stone forming diseases. Kidney Int 72:1065–1072. doi:10.1038/sj.ki.5002441
Tfelt-Hansen J, Brown EM (2004) The calcium-sensing receptor in normal physiology and pathophysiology: a review. Crit Rev Clin Lab Sci 42:35–48. doi:10.1080/10408360590886606
Vezzoli G, Tanini A, Ferrucci L, Soldati L, Bianchin C, Franceschelli F et al (2002) Influence of calcium-sensing receptor gene on urinary calcium excretion in stone-forming patients. J Am Soc Nephrol 13:2125–2517. doi:10.1097/01.ASN.0000030077.72157.D2
Vezzoli G, Terranegra A, Arcidiacono T, Biasion R, Coviello D, Syren ML et al (2007) R990G polymorphism of calcium-sensing receptor does produce a gain-of-function and predispose to primary hypercalciuria. Kidney Int 71:1155–1163. doi:10.1038/sj.ki.5002156
Hough TA, Bogani D, Cheeseman MT, Favor J, Nesbit MA, Thakker RV, Lyon MF (2004) Activating calcium-sensing receptor mutation in the mouse is associated with cataracts and ectopic calcification. Proc Natl Acad Sci USA 101:13566–13571. doi:10.1073/pnas.0405516101
Prie D, Huart V, Bakouh N, Planelles G, Dellis O, Gerard B et al (2002) Nephrolithiasis and osteoporosis caused by mutations in the type 2a sodium-phosphate cotransporter. N Engl J Med 347:983–988. doi:10.1056/NEJMoa020028
Lapointe Y, Tessier J, Paquette Y, Wallendorff B, Coady MJ, Pichette V et al (2006) NPT2 gene variation in calcium nephrolithiasis with renal phosphate leak. Kidney Int 69:226–233. doi:10.1038/sj.ki.5000437
Bergwitz C, Roslin NM, Tieder M, Loredo-Osti JC, Bastepe M, Abu-Zahra H, Frappier D, Burkett K, Carpenter TO, Anderson D, Garabedian M, Sermet I, Fujiwara TM, Morgan K, Tenenhouse HS, Juppner H (2006) SLC34A3 mutations in patients with hereditary hypophosphatemic rickets with hypercalciuria predict a key role for the sodium-phosphate cotransporter NaPi-Iic in maintaining phosphate homeostasis. Am J Hum Genet 78:179–192. doi:10.1086/499409
Tennenhouse HS (2005) Regulation of phosphorus homeostasis by the type iia Na/phosphate cotransporter. Annu Rev Nutr 25:197–214. doi:10.1146/annurev.nutr.25.050304.092642
Khan SR, Glenton PA (2008) Calcium oxalate crystal deposition in kidneys of hypercalciuric mice with disrupted type IIa sodium-phosphate cotransporter. Am J Physiol Renal Physiol 294:F1109–F1115. doi:10.1152/ajprenal.00620.2007
Wrong OM, Norden AG, Feest TG (1994) Dent’s disease; a familial proximal renal tubular syndrome with low-molecular weight proteinuria, hypercalciuria, nephrocalcinosis, metabolic bone disease, progressive renal failure and a marked male predominance. QJM 87:473–493
Christensen EI, Devuyst O, Dom G, Nielsen R, Van der Smissen P, Verroust P et al (2003) Loss of chloride channel ClC-5 impairs endocytosis by defective trafficking of megalin and cubilin in kidney proximal tubules. Proc Natl Acad Sci USA 100:8472–8479. doi:10.1073/pnas.1432873100
Devuyst O, Jouret F, Auzanneau C, Courtoy PJ (2005) Chloride channels and endocytosis: new insights from Dent’s disease and CIC-5 knockout mice. Nephron Physiol 99:69–73. doi:10.1159/000083210
Piwon N, Gunther W, Schwake M, Bosl MR, Jentsch TJ (2000) ClC-5 Cl- -channel disruption impairs endocytosis in a mouse model for Dent’s disease. Nature 408:369–373. doi:10.1038/35042597
Gunther W, Piwon N, Jentsch TJ (2003) The ClC-5 chloride channel knock-out mouse-an animal model for Dent’s disease. Pflugers Arch 445:456–462
Loffing J, Loffing-Cueni D, Valderrabano V, Klausli L, Hebert SC et al (2001) Distribution of transcellular calcium and sodium transport pathways along mouse distal nephron. Am J Physiol Renal Physiol 281:F1021–F1027
Suzuki Y, Landowski CP, Hedinger MA (2008) Mechanisms and regulation of epithelial Ca absorption in health and disease. Annu Rev Physiol 70:257–271. doi:10.1146/annurev.physiol.69.031905.161003
Hoenderop JG, van Leeuwen JP, van der Eerden BC et al (2003) Renal Ca2+ wasting, hyperabsorption, and reduced bone thickness in mice lacking TRPV5. J Clin Invest 112:1906–1914
Jiang Y, Ferguson WB, Peng JB (2006) WNK4 enhances TRPV5-mediated calcium transport: potential role in hypercalciuria of familial hyperkalemic hypertension caused by gene mutation of WNK4. Am J Physiol Renal Physiol 292:F545–F554
Colegio OR, Van Itallie CM, McCrea HJ, Rahner C, Anderson JM (2002) Claudins create charge-selective channels in the paracellular pathway between epithelial cells. Am J Physiol Cell Physiol 283:C142–C147
Konrad M, Schlingmann KP, Gudermann T (2004) Insights into the molecular nature of magnesium homeostasis. Am J Physiol Renal Physiol 286:F599–F605. doi:10.1152/ajprenal.00312.2003
Weber S, Schneider L, Peters M, Misselwitz J, Ronnefarth G, Boswald M, Bonzel KE, Seeman T, Sulakova T, Kuwertz-Broking E, Gregoric A, Palcoux JB, Tasic V, Manz F, Scharer K, Seyberth HW, Konrad M (2001) Novel paracellin-1 mutations in 25 families with familial hypomagnesemia with hypercalciuria and nephrocalcinosis. J Am Soc Nephrol 12:1872–1881
Muller D, Kausalya PJ, Claverie-Martin F, Meij IC, Eggert P, Garcia-Nieto V, Hunziker W (2003) A novel claudin 16 mutation associated with childhood hypercalciuria abolishes binding to ZO-1 and results in lysosomal mistargeting. Am J Hum Genet 73:1293–1301. doi:10.1086/380418
Arking DE (2002) Association of human aging with a functional variant of klotho. Proc Natl Acad Sci USA 99:856–861. doi:10.1073/pnas.022484299
Kuro-o M, Matsumora Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kanaem T, Kume E, Iwasaki H, Iida A, Shiraki-iida T, Nishikawa S, Nagai R, Nabeshima Y (1997) Mutation of the mouse klotho gene leads to a syndrome resembling aging. Nature 390:45–51. doi:10.1038/36285
Ogata N, Matsumura Y, Shiraki M, Kawano K, Koshizuka Y, Hosoi T, Nakamura K, Kuro-o M, Kawaguchi H (2002) Association of klotho gene polymorphism with bone density and spondylosis of the lumbar spine in postmenopausal women. Bone 31:37–41. doi:10.1016/S8756-3282(02)00786-X
Tsuruoka S, Nishi K, Ioka T, Ando H, Saito Y, Kurabayashi M, Nagai R, Fujimora A (2006) Defect in parathyroid hormone induced luminal calcium absorption in connecting tubules of klotho mice. Nephrol Dial Transplant 21:2762–2767
Chang Q, Hoefs S, ven der Kemp AW, Topala AW, Bindels RJ, Hoenderop JG (2005) The beta glucoronidase klotho hydrolyzes and activates TRPV5 channel. Science 310:490–493. doi:10.1126/science.1114245
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S, Hu MC, Moe OW, Kuro-o M (2006) Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem 281:6120–6123. doi:10.1074/jbc.C500457200
Marengo SR, Romani AMP (2008) Oxalate in renal stone disease: the terminal metabolite that just won’t go away. Nat Clin Pract Nephrol 4:368–377
Danpure CJ, Rumsby G (1995) Enzymology and molecular genetics of primary hyperoxaluria type 1, consequences for clinical management. In: Khan SR (ed) Calcium oxalate in biological systems. CRC Press Inc, Boca Raton, pp 189–205
Cramer SD, Ferree PM, Lin K, Milliner DS, Holmes RP (1999) The gene encoding hydroxypyruvate reductase (GRHPR) is mutated in patients with primary hyperoxaluria type II. Hum Mol Genet 8:2063–2069. doi:10.1093/hmg/8.11.2063
Salido EC, Li XM, Lu Y, Wang X, Santana A, Roy-Chowdhury N, Torres A, Shapiro LJ, Roy-Chowdhury J (2006) Alanine-glyoxylate aminotransferase-deficient mice, a model for primary hyperoxaluria that responds to adenoviral gene transfer. Proc Natl Acad Sci USA 103:18249–18254. doi:10.1073/pnas.0607218103
Alper SL (2003) Diseases of mutations in the SLC4A1/AE1 (band 3) Cl–/HCO3–exchanger. In: Broer S, Wagner CA (eds) Membrane transporter diseases. Kluwer, New York, pp 39–63
Stehberger PA, Shmukler BE, Stuart-Tilley AK, Peters LL, Alper SL, Wagner CA (2007) Distal renal tubular acidosis in mice lacking the AE1 (band3) Cl−/HCO3-exchanger (slc4a1). J Am Soc Nephrol 18:1408–1418. doi:10.1681/ASN.2006101072
Knight J, Holmes RP, Assimos DG (2007) Intestinal and renal handling of oxalate loads in normal individuals and stone formers. Urol Res 35:111–117. doi:10.1007/s00240-007-0090-8
Krishnamurthy M, Hruska KA, Chandhoke PS (2003) The urinary response to an oral oxalate load in recurrent calcium stone formers. J Urol 169:2030–2035. doi:10.1097/01.ju.0000062527.37579.49
Hatch M, Freel RW (2005) Intestinal transport of an obdurate anion: oxalate. Urol Res 33:1–16. doi:10.1007/s00240-004-0445-3
Mount DB, Romero MF (2004) The SLC26 gene family of multifunctional anion exchangers. Pflugers Arch 447:710–721. doi:10.1007/s00424-003-1090-3
Soleimani M (2006) Expression, regulation and the role of SLC26 Cl−/HCO3–exchangers in kidney and gastrointestinal tract. Novartis Found Symp 273:91–102. doi:10.1002/0470029579.ch7
Soleimani M, Xu J (2006) SLC26 chloride/nase exchangers in the kidney in health and disease. Semin Nephrol 26:375–385. doi:10.1016/j.semnephrol.2006.07.005
Xie Q, Welch R, Mercado A, Romero MF, Mount DB (2002) Molecular characterization of the murine Slc26a6 anion exchanger: functional comparison with Slc26a1. Am J Physiol Renal Physiol 283:F826–F838
Wang Z, Wang T, Petrovic S, Tuo B, Riederer B, Barone S, Lorenz JN, Seidler U, Aronson PS, Soleimani M (2005) Renal and intestinal transport defects in Slc26a6-null mice. Am J Physiol Cell Physiol 288:C957–C965. doi:10.1152/ajpcell.00505.2004
Freel RW, Hatch M, Green M, Soleimani M (2006) Ileal oxalate absorption and urinary oxalate excretion are enhanced in Slc26a6 null mice. Am J Physiol 290:G719–G728
Jiang Z, Asplin JR, Evan AP, Rajendran VM, Velazquez H, Nottoli TP, Binder HJ, Aronson PS (2006) Calcium oxalate urolithiasis in mice lacking anion transporter Slc26a6. Nat Genet 38:474–478. doi:10.1038/ng1762
Parks JH, Ruml LA, Pak CYC (1996) Hypocitraturia. In: Coe FL, Favus MJ, Pak CYC, Parks JH, Preminger GM (eds) Kidney stones: medical and surgical management. Lippincott, Philadelphia, pp 905–920
Meyer JL, Smith LH (1975) Growth of calcium oxalate crystals II: inhibition by natural urinary crystal growth inhibitors. Invest Urol 13:36–39
Pak CY, Nicar M, Northcutt C (1982) The definition of the mechanism of hypercalciuria is necessary for the treatment of recurrent stone formers. Contrib Nephrol 33:136–151
Shah O, Assimos DG, Holmes RP (2005) Genetic and dietary factors in urinary citrate excretion. J Endourol 19:177–182. doi:10.1089/end.2005.19.177
Pak CY (1987) Citrate and renal calculi. Miner Electrolyte Metab 13:257–266
Hamm LL, Alpern RJ (1996) Regulation of acid–base balance, citrate, and urine pH. In: Coe FL, Favus MJ, Pak CYC, Parks JH, Preminger GM (eds) Kidney stones: medical and surgical management. Lippincott, Philadelphia, pp 289–302
Hamm LL, Hering-Smith KS (2002) Pathophysiology of hypocitraturic nephrolithiasis. Endocrinol Metab Clin North Am 31:885–893. doi:10.1016/S0889-8529(02)00031-2
Pajor AM (2001) Conformationally sensitive residues in transmembrane domain 9 of the Na+/dicarboxylate co-transporter. J Biol Chem 276:29961–29968. doi:10.1074/jbc.M011387200
Okamoto N, Aruga S, Matsuzaki S, Takahashi S, Matsushita K, Kitamura T (2007) Associations between renal sodium-citrate co-transporter (hNaDC-1) gene polymorphism and urinary citrate excretion in recurrent renal calcium stone formers and normal controls. Int J Urol 14:344–349. doi:10.1111/j.1442-2042.2007.01554.x
He Y, Chen X, Yu Z, Wu D, Lv Y, Shi S, Zhu H (2004) Sodium dicarboxylate cotransporter-1 expression in renal tissues and its role in rat experimental nephrolithiasis. J Nephrol 17:34–42
Kok DJ, Papapoulos SE, Blomen LMJ, Bijvoet OLM (1988) Modulation of calcium-oxalate monohydrate crystallization kinetics in vitro. Kidney Int 34:346–350. doi:10.1038/ki.1988.187
Ryall RL, Harnett RM, Marshall VR (1988) The effect of urine, pyrophosphate, citrate, magnesium and glycosaminoglycans on the growth and aggregation of calcium oxalate crystals in vitro. Clin Chim Acta 112:349–356. doi:10.1016/0009-8981(81)90458-7
Schwille PO, Rumenapf G, Wolfel G, Kohler R (1988) Urinary pyrophosphate in patients with recurrent urolithiasis and in healthy controls: a reevaluation. J Urol 140:239–245
Sidhu H, Gupta R, Thind SK, Nath R (1986) Inhibition of calcium oxalate monohydrate crystal growth by pyrophosphate, citrate and rat urine. Urol Res 14:299–303. doi:10.1007/BF00262379
Achilles W, Coors D, Reifenberger B, Sallis JD, Schalk CH (1989) Natural and artificial substances as inhibitors of crystal growth of calcium oxalates in gel matrices. In: Vahlensieck W, Gasser G, Hesse A, Schoeneich G (eds) Urolithiasis, proceedings 1st European symposium on urolithiasis, Bonn. Excerpta Medica, Amsterdam. ISBN 90 219 9865 3, pp 65–67
Grases F, Ramis M, Costa-Bauza A (2000) Effects of phytate and pyrophosphate on brushite and hydroxyapatite crystallization—comparison with the action of other polyphosphates. Urol Res 28:136–140. doi:10.1007/s002400050152
Robertson WG (1973) Factors affecting the precipitation of calcium phosphate in vitro. Calcif Tissue Res 11:311–322. doi:10.1007/BF02547230
Laminski NA, Meyers AM, Sonnekus MI, Smyth AE (1990) Prevalence of hypocitraturia and hypopyrophosphaturia in recurrent calcium stone formers: as isolated defects or associated with other metabolic abnormalities. Nephron 56:379–384. doi:10.1159/000186179
Tsui HW, Inman RD, Paterson AD, Reveille JD, Tsui FW (2005) ANKH variant is associated with ankylosing spondylitis: gender differences. Arthritis Res Ther 7:R513–R525. doi:10.1186/ar1701
Canales BK, Leonard SM, Singh JS, Orzano IM, Zimmerman B, Weiland D, Monga M, Krug HS (2006) Spondyloarthropathy: an independent risk factor for kidney stones. J Endourol 20:542–546. doi:10.1089/end.2006.20.542
Korkmaz C, Ozcan A, Akcar N (2005) Increased frequency of ultrasonographic findings suggestive of renal stone patients with ankylosing spondylitis. Clin Exp Rheumatol 23:389–392
Min W, Sgiraga H, Chalko C, Goldfarb S, Krishna GG, Hoyer JR (1998) Quantitative studies of human urinary excretion of uropontin. Kidney Int 53:189–193. doi:10.1046/j.1523-1755.1998.00745.x
Nishio S, Hatanaka M, Takeda H, Iseda T, Iwata H, Yokoyama M (1999) Analysis of urinary concentrations of calcium phosphate crystal-associated proteins: alpha-2-HS-glycoprotein, prothrombin F1, and osteopontin. J Am Soc Nephrol 10:S394–S396
Wesson JA, Johnson RJ, Mazzali M, Beshensky AM, Steitz S, Giachelli C, Liaw L, Alpers CE, Couser WG, Kleinman JG, Hughes J (2003) Osteopontin is acritical inhibitor of calcium oxalate crystal formation and retention in renal tubules. J Am Soc Nephrol 14:139–147. doi:10.1097/01.ASN.0000040593.93815.9D
Gao B, Yasui T, Itoh Y, Li Z, Okada A, Tozawa K, Hayashi Y, Kohri K (2007) Association of osteopontin gene haplotypes with nephrolithiasis. Kidney Int 72:592–598. doi:10.1038/sj.ki.5002345
Fisher LW, Hawkins GR, Tuross N, Termine JD (1987) Purification and partial characterization of small proteoglycans I and II, bone sialoproteins I and II, and osteonectin from the mineral compartment of developing human bone. J Biol Chem 262:9702–9708
Singh K, DeVouge MW, Mukherjee BB (1990) Physiological properties and differential glycosylation of phosphorylated and nonphosphorylated forms of osteopontin secreted by normal rat kidney cells. J Biol Chem 265:18696–18701
Hunter GK, Kyle CL, Goldberg HA (1994) Modulation of crystal formation by bone phosphoproteins; structural specificity of the osteopontin-mediated inhibition of hydroxyapatite formation. Biochem J 300:723–728
Hoyer JR, Asplin JR, Otvos LJ (2001) Phosphorylated osteopontin peptides suppress crystallization by inhibiting growth of calcium oxalate crystals. Kidney Int 60:77–82. doi:10.1046/j.1523-1755.2001.00772.x
Atmani F, Glenton PA, Khan SR (1998) Identification of proteins extracted from calcium oxalate and calcium phosphate crystals induced in the urine of healthy and stone forming subjects. Urol Res 26:201–207. doi:10.1007/s002400050047
Glauser A, Horhreiter W, Jaeger P, Hess B (2000) Determinants of urinary excretion of Tamm-Horsfall protein in non-selected kidney stone formers and healthy subjects. Nephrol Dial Transplant 15:158–1587. doi:10.1093/ndt/15.10.1580
Romero MC, Nocera S, Nesse AB (1997) Decreased Tamm-Horsfall protein in lithiasis patients. Clin Biochem 30:63–67. doi:10.1016/S0009-9120(96)00136-1
Schnierle P (1995) A simple diagnostic method for the differentiation of Tamm-Horsfall glycoprotein from healthy probands and those from recurrent calcium oxalate renal stone formers. Experimentia 51:1068–1072. doi:10.1007/BF01946918
Mo L, Huang H-Y, Zhu X-H, Shapiro E, Hasty DL, X-Ru Wu (2004) Tamm-Horsfall protein is a critical renal defense factor protecting against calcium oxalate crystal formation. Kidney Int 66:1159–1166. doi:10.1111/j.1523-1755.2004.00867.x
Mo L, Liaw L, Evan AP, Sommer AJ, Lieske JC, Wu X-R (2007) Renal calcinosis and stone formation in mice lacking osteopontin, Tamm-Horsfall protein, or both. Am J Physiol Renal Physiol 293:F1935–F1943. doi:10.1152/ajprenal.00383.2007
Bernascone I, Vavassori S, Di Pentima AD, Santambrogio S, Lamorte G, Amoroso A, Scolari F, Ghiggeri GM, Casari G, Polishchuk R, Rampoldi L (2006) Defective intracellular trafficking of uromodulin mutant isoforms. Traffic 7:1567–1579. doi:10.1111/j.1600-0854.2006.00481.x
Serafini-Cessi F, Maligolini N, Cavallone D (2003) Tamm-Horsfall protein glycoprotein: biology and clinical relevance. Am J Kidney Dis 42:658–676. doi:10.1016/S0272-6386(03)00829-1
Biri H, Ozturk HS, Buyukkocak S, Kacmaz M, Cimen MYB, Unal D, Birey M, Bozkirli I, Durak I (1998) Antioxidant defense potential of rabbit renal tissues after ESWL: protective effects of antioxidant vitamins. Nephron 79:181–185. doi:10.1159/000045022
Atmani F, Lacour B, Jungers P, Drüeke T, Daudon M (1994) Reduced inhibitory activity of uronic-acid-rich protein in urine of stone formers. Urol Res 22:257–260. doi:10.1007/BF00541903
Suzuki S, Kobayashi H, Kageyama S, Shibata K, Fujie M, Terao T (2001) Excretion of bikunin and its fragments in the urine of patients with renal stones. J Urol 166:268–274. doi:10.1016/S0022-5347(05)66143-5
Medetognon-Benissan J, Tardivel S, Hennequin C, Daudon T, Drueke T, Lacour B (1999) Inhibitory effect of bikunin on calcium oxalate crystallization in vitro and urinary bikunin decrease in renal stone formers. Urol Res 27:69–75. doi:10.1007/s002400050091
Atmani F, Khan SR (1999) Role of urinary bikunin in the inhibition of calcium oxalate crystallization. J Am Soc Nephrol 10:S385–S390
Atmani F, Mizon J, Khan SR (1996) Identification of uronic-acid-rich protein as urinary bikunin, the light chain of inter-α-inhibitor. Eur J Biochem 236:984–990. doi:10.1111/j.1432-1033.1996.00984.x
Ebisuno S, Nishihata M, Inagaki T, Umehara M, Kohjimoto Y (1999) Bikunin prevents adhesion of CaOx crystal to renal tubular cells in human urine. J Am Soc Nephrol 10:S436
Tardivel S, Medetognon J, Randoux C, Kebede M, Drueke T, Daudon M, Hennequin C, Lacour B (1999) Alpha-1-microglobulin: inhibitory effect on calcium oxalate crystallization in vitro and decreased urinary concentration in calcium oxalate stone formers. Urol Res 27:243–249. doi:10.1007/s002400050117
Khan SR (2005) Hyperoxaluria-induced oxidative stress and antioxidants for renal protection. Urol Res 33:349–357. doi:10.1007/s00240-005-0492-4
Acknowledgments
Research supported by NIH grants # RO1DK065658 and RO1DK59765, and The University of Florida Center for the Study of Lithiasis and Pathological Calcification.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, S.R., Canales, B.K. Genetic basis of renal cellular dysfunction and the formation of kidney stones. Urol Res 37, 169–180 (2009). https://doi.org/10.1007/s00240-009-0201-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-009-0201-9