Abstract
Increased serum levels of alkaline phosphatase (ALP) are widely recognized as a biochemical marker of many disorders affecting the liver or bone. However, the approach for patients with low ALP phosphatase is not well-established. Low serum ALP is an epiphenomenon of many severe acute injuries and diseases. Persistently low serum ALP may be secondary to drug therapy (including antiresorptives) or a variety of acquired disorders, such as malnutrition, vitamin and mineral deficiencies, endocrine disorders, etc. Hypophosphatasia, due to pathogenic variants of the ALPL gene, which encodes tissue non-specific ALP, is the most common genetic cause of low serum ALP. Marked bone hypomineralization is frequent in severe pediatric-onset cases. However, adult forms of hypophosphatasia usually present with milder manifestations, such as skeletal pain, chondrocalcinosis, calcific periarthritis, dental problems, and stress fractures. The diagnostic approach to these patients is discussed. Measuring several ALP substrates, such as pyrophosphate, pyridoxal phosphate, or phosphoethanolamine, may help to establish enzyme deficiency. Gene analysis showing a pathogenic variant in ALPL may confirm the diagnosis. However, a substantial proportion of patients show normal results after sequencing ALPL exons. It is still unknown if those patients carry unidentified mutations in regulatory regions of ALPL, epigenetic changes, or abnormalities in other genes.



Similar content being viewed by others
References
Whyte MP (2017) Hypophosphatasia: an overview for 2017. Bone 102:15–25. https://doi.org/10.1016/j.bone.2017.02.011
Whyte MP (2016) Hypophosphatasia—aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol 12:233–246. https://doi.org/10.1038/NRENDO.2016.14
Sekaran S, Selvaraj V, Thangavelu L (2021) The physiological and pathological role of tissue nonspecific alkaline phosphatase beyond mineralization. Biomolecules. https://doi.org/10.3390/BIOM11111564
Komaru K, Ishida-Okumura Y, Numa-Kinjoh N et al (2019) Molecular and cellular basis of hypophosphatasia. J oral Biosci 61:141–148. https://doi.org/10.1016/J.JOB.2019.07.003
Schmidt T, Schmidt C, Amling M et al (2021) Prevalence of low alkaline phosphatase activity in laboratory assessment: is hypophosphatasia an underdiagnosed disease? Orphanet J Rare Dis. https://doi.org/10.1186/S13023-021-02084-W
Maman E, Borderie D, Roux C, Briot K (2016) Absence of recognition of low alkaline phosphatase level in a tertiary care hospital. Osteoporos Int 27:1251–1254. https://doi.org/10.1007/S00198-015-3346-0
Guañabens N, Mumm S, Möller I et al (2014) Calcific periarthritis as the only clinical manifestation of hypophosphatasia in middle-aged sisters. J Bone Miner Res 29:929–934. https://doi.org/10.1002/JBMR.2110
Wang Z, Guo H, Wang Y et al (2014) Interfering effect of bilirubin on the determination of alkaline phosphatase. Int J Clin Exp Med 7:4244
McKiernan FE, Shrestha LK, Berg RL, Fuehrer J (2014) Acute hypophosphatasemia. Osteoporos Int 25:519–523
Napal J, Amado JAA, Riancho JAA et al (1993) Stress decreases the serum level of osteocalcin. Bone Miner 21:113–118. https://doi.org/10.1016/S0169-6009(08)80013-X
van Dommelen CKV, Klaassen CHL (1964) Cyanocobalamin-dependent depression of the serum alkaline phosphatase level in patients with pernicious anemia. N Engl J Med 271:541–544. https://doi.org/10.1056/NEJM196409102711104
Kim GS, Kim CH, Park JY et al (1996) Effects of vitamin B12 on cell proliferation and cellular alkaline phosphatase activity in human bone marrow stromal osteoprogenitor cells and UMR106 osteoblastic cells. Metabolism 45:1443–1446. https://doi.org/10.1016/S0026-0495(96)90171-7
Shaver WA, Bhatt H, Combes B (1986) Low serum alkaline phosphatase activity in Wilson’s disease. Hepatology 6:859–863. https://doi.org/10.1002/HEP.1840060509
Güngör Ş, Selimoğlu MA, Bağ HGG, Varol F (2020) Is it possible to diagnose fulminant Wilson’s disease with simple laboratory tests? Liver Int 40:155–162. https://doi.org/10.1111/LIV.14263
Gibbon VE, Harington JS, Penny CB, Fredlund V (2010) Mseleni joint disease: a potential model of epigenetic chondrodysplasia. Jt bone spine 77:399–404. https://doi.org/10.1016/J.JBSPIN.2010.01.013
Mornet E (2018) Hypophosphatasia. Metabolism 82:142–155. https://doi.org/10.1016/J.METABOL.2017.08.013
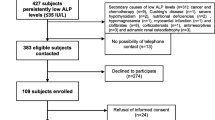
Riancho-Zarrabeitia L, García-Unzueta M, Tenorio JA et al (2016) Clinical, biochemical and genetic spectrum of low alkaline phosphatase levels in adults. Eur J Intern Med 29:40–45. https://doi.org/10.1016/j.ejim.2015.12.019
López-Delgado L, Riancho-Zarrabeitia L, García-Unzueta MT et al (2018) Abnormal bone turnover in individuals with low serum alkaline phosphatase. Osteoporos Int 29:2147–2150. https://doi.org/10.1007/s00198-018-4571-0
Berkseth KE, Tebben PJ, Drake MT et al (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54:21–27
Schmidt T, Mussawy H, Rolvien T et al (2017) Clinical, radiographic and biochemical characteristics of adult hypophosphatasia. Osteoporos Int 28:2653–2662. https://doi.org/10.1007/S00198-017-4087-Z
Alonso N, Larraz-Prieto B, Berg K et al (2020) Loss-of-function mutations in the ALPL gene presenting with adult onset osteoporosis and low serum concentrations of total alkaline phosphatase. J Bone Miner Res 35:657–661. https://doi.org/10.1002/JBMR.3928
Shane E, Burr D, Ebeling PR et al (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the american society for bone and mineral research. J Bone Miner Res 25:2267–2294. https://doi.org/10.1002/jbmr.253
Sutton RAL, Mumm S, Coburn SP et al (2012) “Atypical femoral fractures” during bisphosphonate exposure in adult hypophosphatasia. J Bone Miner Res 27:987–994. https://doi.org/10.1002/jbmr.1565
Rassie K, Dray M, Michigami T, Cundy T (2019) Bisphosphonate use and fractures in adults with hypophosphatasia. JBMR plus. https://doi.org/10.1002/JBM4.10223
Chodirker BN, Coburn SP, Seargeant LE et al (1990) Increased plasma pyridoxal-5′-phosphate levels before and after pyridoxine loading in carriers of perinatal/infantile hypophosphatasia. J Inherit Metab Dis 13:891–896. https://doi.org/10.1007/BF01800216
Whyte MP, May JD, McAlister WH et al (2021) Vitamin B6 deficiency with normal plasma levels of pyridoxal 5′-phosphate in perinatal hypophosphatasia. Bone. https://doi.org/10.1016/j.bone.2021.116007
Whyte MP, Zhang F, Wenkert D et al (2022) Hypophosphatasia: vitamin B6 status of affected children and adults. Bone. https://doi.org/10.1016/j.bone.2021.116204
del Angel G, Reynders J, Negron C et al (2020) Large-scale in vitro functional testing and novel variant scoring via protein modeling provide insights into alkaline phosphatase activity in hypophosphatasia. Hum Mutat 41:1250–1262. https://doi.org/10.1002/HUMU.24010
Bianchi ML, Bishop NJ, Guañabens N et al (2020) Hypophosphatasia in adolescents and adults: overview of diagnosis and treatment. Osteoporos Int 31:1445–1460. https://doi.org/10.1007/S00198-020-05345-9
Guarnieri V, Sileri F, Indirli R et al (2022) Clinical, biochemical and genetic findings in adult patients with chronic hypophosphatasemia. J Endocrinol Invest 45:125–137. https://doi.org/10.1007/S40618-021-01625-1
Santurtun M, Mediavilla-Martinez E, Vega AI et al (2022) Pain and health-related quality of life in patients with hypophosphatasemia with and without ALPL gene mutations. Front Endocrinol (Lausanne) 13:965476. https://doi.org/10.3389/fendo.2022.965476
Masi L, Marini F, Franceschelli F et al (2021) Polymorphic variants of alkaline phosphatase gene correlate with clinical signs of adult hypophosphatasia? Osteoporos Int 32:2461–2472. https://doi.org/10.1007/S00198-021-05893-8
Delgado-Calle J, Sanudo C, Sanchez-Verde L et al (2011) Epigenetic regulation of alkaline phosphatase in human cells of the osteoblastic lineage. Bone 49:830–838
Tornero C, Navarro-Compán V, Buño A et al (2022) Biochemical algorithm to identify individuals with ALPL variants among subjects with persistent hypophosphatasaemia. Orphanet J Rare Dis. https://doi.org/10.1186/s13023-022-02253-5
Tornero C, Navarro-Compán V, Tenorio JA et al (2020) Can we identify individuals with an ALPL variant in adults with persistent hypophosphatasaemia? Orphanet J Rare Dis. https://doi.org/10.1186/S13023-020-1315-Y
Liu W, Zhang L, Xuan K et al (2018) Alpl prevents bone ageing sensitivity by specifically regulating senescence and differentiation in mesenchymal stem cells. Bone Res 6:27. https://doi.org/10.1038/S41413-018-0029-4
Huggins E, Ong R, Rockman-Greenberg C et al (2020) Multigenerational case examples of hypophosphatasia: challenges in genetic counseling and disease management. Mol Genet Metab reports. https://doi.org/10.1016/J.YMGMR.2020.100661
Hofmann C, Girschick H, Mornet E et al (2014) Unexpected high intrafamilial phenotypic variability observed in hypophosphatasia. Eur J Hum Genet 22:1160–1164. https://doi.org/10.1038/EJHG.2014.10
Black DM, Geiger EJ, Eastell R et al (2020) Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med 383:743–753. https://doi.org/10.1056/nejmoa1916525
Whyte MP, Greenberg CR, Salman NJ et al (2012) Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med 366:904–913. https://doi.org/10.1056/NEJMOA1106173
Whyte MP, Simmons JH, Moseley S et al (2019) Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial. Lancet Diabetes Endocrinol 7:93–105. https://doi.org/10.1016/S2213-8587(18)30307-3
Kishnani PS, Rockman-Greenberg C, Rauch F et al (2019) Five-year efficacy and safety of asfotase alfa therapy for adults and adolescents with hypophosphatasia. Bone 121:149–162. https://doi.org/10.1016/J.BONE.2018.12.011
Khan AA, Josse R, Kannu P et al (2019) Hypophosphatasia: Canadian update on diagnosis and management. Osteoporos Int 30:1713–1722. https://doi.org/10.1007/S00198-019-04921-Y
Funding
No specific funding was received for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jose A. Riancho have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Riancho, J.A. Diagnostic Approach to Patients with Low Serum Alkaline Phosphatase. Calcif Tissue Int 112, 289–296 (2023). https://doi.org/10.1007/s00223-022-01039-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-022-01039-y