Abstract
Introduction and hypothesis
The use of mesh in pelvic organ prolapse (POP) surgery has become a widespread treatment option, but carries a risk of specific complications. The objective was to report the rate and type of reoperation for mesh-related complications after pelvic organ prolapse surgery in an urogynecological referral center over a period of 8 years.
Methods
A retrospective study was carried out including all patients operated for a mesh complication after prolapse surgery between September 2006 and September 2014 in the urogynecology unit in Nîmes hospital.
Results
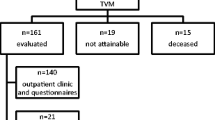
Sixty-nine mesh complications were recorded among the 67 patients included. Surgical treatment of mesh-related complications accounted for 7% of all pelvic surgeries performed in our center. Thirty-two patients (47.8%) were referred from other centers and 35 patients (52.2%) were initially operated in our unit. The global rate of reintervention for mesh-related complications after prolapse repair performed in our unit was 2.8%. Of 69 mesh complications, 48 patients (71.6%) had transvaginal mesh (TVM) and 19 patients (28.4%) sacrocolpopexy (SCP). The indication for surgery was a symptomatic or large vaginal erosion (47.8%), symptomatic mesh contraction (20.3%), and infection (11.6%). The most frequent primary symptom was pelvic/perineal pain or dyspareunia (33.3% of cases). The mean time between initial mesh surgery and the reoperation for a complication was 33.4 months (95% CI, 24.5 to 42.2). Eleven patients (15.9%) required several interventions. In total, 77.9% of patients experienced complete recovery of symptoms after surgical management.
Conclusion
In a referral center the global rate of reinterventions for mesh-related complications after POP repair is 2.8%. The surgical treatment of mesh complications appears to be a safe and effective procedure with cure of the symptoms in most cases.



Similar content being viewed by others
References
Helström L, Nilsson B. Impact of vaginal surgery on sexuality and quality of life in women with urinary incontinence or genital descensus. Acta Obstet Gynecol Scand. 2005;84(1):79–84.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277–85.
Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806.
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104(4):805–23.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376.
Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol. 2009;113(2 Pt 1):367–73.
De Tayrac R, Sentilhes L. Complications of pelvic organ prolapse surgery and methods of prevention. Int Urogynecol J. 2013;24(11):1859–72.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079.
Food Drug Administration FDA. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm.
South MMT, Foster RT, Webster GD, Weidner AC, Amundsen CL. Surgical excision of eroded mesh after prior abdominal sacrocolpopexy. Am J Obstet Gynecol. 2007;197(6):615.e1–5.
Margulies RU, Lewicky-Gaupp C, Fenner DE, McGuire EJ, Clemens JQ, Delancey JOL. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008;199(6):678.e1–4.
Ridgeway B, Walters MD, Paraiso MFR, Barber MD, McAchran SE, Goldman HB, et al. Early experience with mesh excision for adverse outcomes after transvaginal mesh placement using prolapse kits. Am J Obstet Gynecol. 2008;199(6):703.e1–7.
Hurtado EA, Appell RA. Management of complications arising from transvaginal mesh kit procedures: a tertiary referral center’s experience. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):11–7.
Marcus-Braun N, von Theobald P. Mesh removal following transvaginal mesh placement: a case series of 104 operations. Int Urogynecol J. 2010;21(4):423–30.
Feiner B, Maher C. Vaginal mesh contraction: definition, clinical presentation, and management. Obstet Gynecol. 2010;115(2 Pt 1):325–30.
Tijdink MM, Vierhout ME, Heesakkers JP, Withagen MIJ. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. 2011;22(11):1395–404.
Skala C, Renezeder K, Albrich S, Puhl A, Laterza RM, Naumann G, et al. The IUGA/ICS classification of complications of prosthesis and graft insertion: a comparative experience in incontinence and prolapse surgery. Int Urogynecol J. 2011;22(11):1429–35.
Firoozi F, Ingber MS, Moore CK, Vasavada SP, Rackley RR, Goldman HB. Purely transvaginal/perineal management of complications from commercial prolapse kits using a new prostheses/grafts complication classification system. J Urol. 2012;187(5):1674–9.
Lee D, Dillon B, Lemack G, Gomelsky A, Zimmern P. Transvaginal mesh kits—how “serious” are the complications and are they reversible? Urology. 2013;81(1):43–8.
Abbott S, Unger CA, Evans JM, Jallad K, Mishra K, Karram MM, et al. Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. Am J Obstet Gynecol. 2014;210(2):163.e1–8.
Arsene E, Giraudet G, Lucot J-P, Rubod C, Cosson M. Sacral colpopexy: long-term mesh complications requiring reoperation(s). Int Urogynecol J. 2015;26(3):353–8.
Crosby EC, Abernethy M, Berger MB, DeLancey JO, Fenner DE, Morgan DM. Symptom resolution after operative management of complications from transvaginal mesh. Obstet Gynecol. 2014;123(1):134–9.
Withagen MI, Vierhout ME, Hendriks JC, Kluivers KB, Milani AL. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet Gynecol. 2011;118(3):629–36.
De Landsheere L, Ismail S, Lucot J-P, Deken V, Foidart J-M, Cosson M. Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol. 2012;206(1):83.e1–7.
Quemener J, Joutel N, Lucot J-P, Giraudet G, Collinet P, Rubod C, et al. Rate of re-interventions after transvaginal pelvic organ prolapse repair using partially absorbable mesh: 20 months median follow-up outcomes. Eur J Obstet Gynecol Reprod Biol. 2014;175:194–8.
Belot F, Collinet P, Debodinance P, Ha Duc E, Lucot J-P, Cosson M. Risk factors for prosthesis exposure in treatment of genital prolapse via the vaginal approach. Gynécologie Obstétrique Fertil. 2005;33(12):970–4.
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot J-P, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):315–20.
Deffieux X, de Tayrac R, Huel C, Bottero J, Gervaise A, Bonnet K, et al. Vaginal mesh erosion after transvaginal repair of cystocele using Gynemesh or Gynemesh-Soft in 138 women: a comparative study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(1):73–9.
Chanelles O, Poncelet C. Late vaginal mesh exposure after prolapse repair. J Gynécologie Obstétrique Biol Reprod. 2010;39(8):672–4.
Miklos JR, Chinthakanan O, Moore RD, Mitchell GK, Favors S, Karp DR, et al. The IUGA/ICS classification of synthetic mesh complications in female pelvic floor reconstructive surgery: a multicenter study. Int Urogynecol J. 2016;27(6):933–8.
Haylen BT, Freeman RM,Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J. 2011;22(1):3–15.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Abdel-Fattah M, Ramsay I, West of Scotland Study Group. Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG Int J Obstet Gynaecol. 2008;115(1):22–30.
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B. Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(7):743–52.
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R. Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(9):1059–64.
Kasyan G, Abramyan K, Popov AA, Gvozdev M, Pushkar D. Mesh-related and intraoperative complications of pelvic organ prolapse repair. Cent Eur J Urol. 2014;67(3):296–301.
Deffieux X, Sentilhes L, Savary D, Letouzey V, Marcelli M, Mares P, et al. Indications of mesh in surgical treatment of pelvic organ prolapse by vaginal route: expert consensus from the French College of Gynecologists and Obstetricians (CNGOF). J Gynécologie Obstétrique Biol Reprod. 2013;42(7):628–38.
Deffieux X, Letouzey V, Savary D, Sentilhes L, Agostini A, Mares P, et al. Prevention of complications related to the use of prosthetic meshes in prolapse surgery: guidelines for clinical practice. Eur J Obstet Gynecol Reprod Biol. 2012;165(2):170–80.
Deffieux X, Huel C, de Tayrac R, Bottero J, Porcher R, Gervaise A, et al. Vaginal mesh extrusion after transvaginal repair of cystocele using a prosthetic mesh: Treatment and functional outcomes. J Gynécologie Obstétrique Biol Reprod. 2006;35(7):678–84.
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004;190(1):20–6.
Blandon RE, Gebhart JB, Trabuco EC, Klingele CJ. Complications from vaginally placed mesh in pelvic reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(5):523–31.
Gyang AN, Feranec JB, Patel RC, Lamvu GM. Managing chronic pelvic pain following reconstructive pelvic surgery with transvaginal mesh. Int Urogynecol J. 2014;25(3):313–8.
Batalden RP, Weinstein MM, Foust-Wright C, Alperin M, Wakamatsu MM, Pulliam SJ. Clinical application of IUGA/ICS classification system for mesh erosion. Neurourol Urodyn. 2015;35(5):589–94.
Bontje HF, van de Pol G, van der Zaag-Loonen HJ, Spaans WA. Follow-up of mesh complications using the IUGA/ICS category-time-site coding classification. Int Urogynecol J. 2014;25(6):817–22.
Bako A, Dhar R. Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):103–11.
Jacquetin B, Cosson M. Complications of vaginal mesh: our experience. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(8):893–6.
Swift S. To mesh or not to mesh? That is the question. Int Urogynecol J. 2011;22(5):505–6.
De Ridder D. Should we use meshes in the management of vaginal prolapse? Curr Opin Urol. 2008;18(4):377–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
S. Warembourg and M. Labaki declare that they have no conflicts of interest. B. Fatton declares acceptance of paid travel expenses from Boston Scientific and declares being a consultant for Allergan and Astellas. R. de Tayrac declares acceptance of paid travel expenses, payment for research, and being a consultant for Boston Scientific. P. Costa declares acceptance of paid travel expenses and being a consultant for Allergan and Boston Scientific.
Rights and permissions
About this article
Cite this article
Warembourg, S., Labaki, M., de Tayrac, R. et al. Reoperations for mesh-related complications after pelvic organ prolapse repair: 8-year experience at a tertiary referral center. Int Urogynecol J 28, 1139–1151 (2017). https://doi.org/10.1007/s00192-016-3256-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3256-5