Abstract
Introduction and hypothesis
This is a presentation of case series after the use of alloplasic material in urogynaecology.
Methods
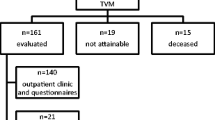
From 2004 to 2010, a total 179 patients with complications have been referred directly after the use of alloplastic material in incontinence and prolapse surgery. Of this total, 125 patients had a previous vaginal sling plasty because of urinary stress incontinence, while 54 patients underwent a prolapse surgery with mesh use. Symptoms and findings are expressed by the recently introduced International Urogynecological Association/International Continence Society (IUGA/ICS) terminology.
Results
The most frequent findings after vaginal sling plasty were bladder outlet obstruction, pain and tape exposure. The most frequent findings after prolapse surgery were pain and mesh erosion. The IUGA/ICS classification does not give the possibility to express functional disorders. Most revisions were done more than 2 months after surgery. After incontinence surgery, mostly the vaginal area of suture line was affected; after prolapse surgery, the vagina and the trocar passage were affected.
Conclusions
Mesh complication and affected site after prolapse surgery do differ from those after incontinence surgery. The IUGA/ICS classification of mesh complication facilitates the comparison of mesh complication.
Similar content being viewed by others
Abbreviations
- IUGA:
-
International Urogynecological Association
- ICS:
-
International Continence Society
- CTS:
-
code C category T time, S site
- SUI:
-
Stress urinary incontinence
- TVT:
-
Tension-free vaginal tape
- BOO:
-
Bladder outlet obstruction
References
Karram MM, Segal JL, Vasallo BJ, Kleemann SD (2003) Complications and untoward effects of the tension free vaginal tape procedure. Obstet Gynecol 101:929–932
Miedel A, Tegerstedt G, Mörlin B, Hammarström M (2008) A 5 year prospective follow-up study of vaginal surgery for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 19(12):1593–1601
Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111:891–898
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R (2007) Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18:1059–1064
Nieminen K, Hiltunen R, Heiskanen E, Tarala T, Niemi K, Merikari M, Heinonen PK (2008) Symptom resolution and sexual function after anterior vaginal wall repair with or without polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct 19:1611–1616
Altmann D, Falconer C, for the Nordic Transvaginal Mesh Group (2007) Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol 109:303–308
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18(7):743–752
Abdel-Fattah M, Ramsay I, On behalf of the West of Scotland Study Group (2008) Retrospective multicenter study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG 115:22–30
Karlovsky ME, Thakre AA, Rastinehad A, Kushner L, Badlani GH (2005) Biomaterials for pelvic floor reconstruction. Urology 66:469–475
Comiter CV, Colgrove PM (2004) High rate of vaginal extrusion of silicone-coated polyester sling. Urology 63:1066–1070
Huebner M, Hsu Y, Fenner DE (2006) The use of graft materials in vaginal pelvic floor surgery. Int J Gynaecol Obstet 92:279–288
Baessler K, Hewson AD, Tunn R, Schuessler B, Maher CF (2005) Severe mesh complications following intravaginal slingplasty. Obstet Gynecol 106:713–716
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, Dwyer PL, Fatton B, Kocjancic E, Lee J, Maher C, Petri E, Rizk DE, Sand PK, Schaer GN, Webb RJ (2011) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Int Urogynecol J 22:3–15
Petri E, Niemeyer R, Martan A, Tunn R, Naumann G, Koelbl H (2005) Reasons for and treatment of surgical complications with alloplastic slings. Int Urogynecol J Pelvic Floor Dysfunct 17:3–13
Kuuva N, Nilsson CG (2002) A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand 81(1):72–77
Tamussino KF, Hanzal E, Kölle D, Ralph G, Riss PA, Austrian Urogynecology Working Group (2001) Tension-free vaginal tape operation: results of the Austrian registry. Obstet Gynecol 98(5 Pt 1):732–736
Martínez-Fornés MT, Fernández Pérez C, Fouz López C, Fernández Lucas C, Borrego Hernando J (2009) A three year follow-up of a prospective open randomized trial to compare tension-free vaginal tape with Burch colposuspension for treatment of female stress urinary incontinence. Actas Urol Esp 33(10):1088–1096
De Tayrac R, Deffieux X, Gervaise A, Chauveaud Lambling A, Fernandesz H (2005) Long-term anatomical and functional assessment of trasnvaginal cystocele repair using a tension free polyproöylene mesh. Int Urogynecol J Pelvic Floor Dysfunct 17:1–6
Benhaim Y, de Tayrac R, Deffieux X, Gervaise A, Chauveaud Lambling A, Frydman R, Fernandesz H (2006) Treatment of genital prolapse with a polypropylene mesh inserted via the vaginal route: anatomic and functional outcome in women aged less than 50 years. J Gynecol Obstet Biol Reprod 35(3):219–226
De Tayrac R, Devoldere G, Renaudie J, Villard P, Guilbaud O, Eglin G, The French Ugytex Study Group (2007) Prolapse repair by vaginal route using a new protected low-weight polypropylene mesh: 1-year functional and anatomical outcome in a prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct 18(3):251–256
Iglesia DB, Sokol AI, Sokol ER, Kudish BI, Guman RE, Peterson JL, Shott S (2010) Vaginal mesh for prolapse. A randomized controlled trial. Obstet Gynecol 116:293–303
Hiltunen R, Nieminen K, Takala T, Heiskanen E, Merikari M, Niemi K (2007) Low weight polypropylene mesh for anterior vaginal wall prolapse: an randomized controlled trial. Obstet Gynecol 110:455–462
Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE (2009) Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol 113:367–373
Margulies RU, Lewicky-Gaupp C, Fenner DE, McGuire EJ, Clemens JQ, Delancey JO (2008) Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol 199(6):678.e1–e4
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skala, C., Renezeder, K., Albrich, S. et al. The IUGA/ICS classification of complications of prosthesis and graft insertion. Int Urogynecol J 22, 1429–1435 (2011). https://doi.org/10.1007/s00192-011-1508-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1508-y