Abstract
Introduction and hypothesis
To compare apical correction in stage ≥3 cystocele between two mesh kits.
Methods
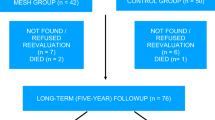
This was a retrospective, nonrandomized study that compared two groups matched on anterior/apical POP-Q stage: 84 received Elevate Ant™ single-incision mesh (Elevate Ant group) and 42 Perigee™ transvaginal mesh (Perigee group). Follow-up at 1 and 2 years comprised objective (POP-Q) and subjective (PFDI-20, PFIQ-7, PISQ-12) assessments. The primary endpoint was objective success: 2-year apical POP-Q stage ≤1. Secondary endpoints were anterior POP-Q stage, subjective results and complications.
Results
Groups were comparable in terms of age (66.6 and 64.7 years, respectively; p = 0.19), BMI (both 25.4 kg/m2; p = 0.93), and history of hysterectomy (7.2 % and 14.3 %; p = 0.21) or prolapse surgery (12 % and 14.3 %; p = 0.72). Operative time was shorter in the Elevate Ant group (54.1 vs. 62.5 min; p = 0.048), and the 2-year objective apical success rate was higher (92.9 % vs. 66.7 %; p < 0.0001), with better point C correction (−5 vs. −3.8; p = 0.006). Function improved in both groups, with significantly better PFIQ-7 (p = 0.03) and PFDI-20 (p = 0.02) scores in the Elevate Ant group at 2 years. Vaginal exposure was not seen in the Elevate Ant group but occurred in two patients in the Perigee group (p = 0.33). Factors associated with success were age >65 years (OR 7.16, 95 % CI 1.83 – 27.97) and treatment with Elevate Ant mesh (OR 10.16, 95 % CI 2.78 – 37.14). Postoperative stress urinary incontinence rate was greater with the Elevate Ant group (29.8 % and 16.7 %; p = 0.11).
Conclusions
The use of the Elevate Ant mesh was associated with significantly better apical correction at 2 years. Function improved in both groups, but with a significantly better PFDI-20 score in the Elevate Ant group at 1 and 2 years. The postoperative stress urinary incontinence rate, however, tended to be greater in the Elevate Ant group. The results need confirming with longer follow-up of these cohorts and in randomized studies.


Similar content being viewed by others
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
De Boer TA, Slieker-Ten Hove MCP, Burger CW, Kluivers KB, Vierhout ME (2011) The prevalence and factors associated with previous surgery for pelvic organ prolapse and/or urinary incontinence in a cross-sectional study in The Netherlands. Eur J Obstet Gynecol Reprod Biol 158:343–349
Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C, Nordic Transvaginal Mesh Group (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med 364:1826–1836
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Lamblin G, Van-Nieuwenhuyse A, Chabert P, Lebail-Carval K, Moret S, Mellier G (2014) A randomized controlled trial comparing anatomical and functional outcome between vaginal colposuspension and transvaginal mesh. Int Urogynecol J 25:961–970
Jacquetin B, Hinoul P, Gauld J, Fatton B, Rosenthal C, Clavé H et al (2013) Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 5-year prospective follow-up study. Int Urogynecol J 24(10):1679–1686
US Food and Drug Administration (2013) Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA Safety Communication. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm
Feiner B, O’Rourke P, Maher C (2012) A prospective comparison of two commercial mesh kits in the management of anterior vaginal prolapse. Int Urogynecol J 23:279–283
Stanford EJ, Moore RD, Roovers JP, VanDrie DM, Giudice TP, Lukban JC et al (2015) Elevate Ant and uterine preservation: 2-year results. Female Pelvic Med Reconstr Surg 21:205–210
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J et al (2012) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn 30:2–12
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23:85–91
Lamblin G, Delorme E, Cosson M, Rubod C (2015) Cystocele and functional anatomy of the pelvic floor: review and update of the various theories. Int Urogynecol J. doi:10.1007/s00192-015-2832-4
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717–1724
DeLancey JO (2012) Surgery for cystocele III: do all cystoceles involve apical descent? Observations on cause and effect. Int Urogynecol J 23:665–667
Petros PE, Woodman PJ (2008) The Integral Theory of continence. Int Urogynecol J Pelvic Floor Dysfunct 19:35–40
Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L (2006) Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol 195:1837–1840
Summers A, Winkel LA, Hussain HK, DeLancey JO (2006) The relationship between anterior and apical compartment support. Am J Obstet Gynecol 194:1438–1443
Yousuf A, Chen L, Larson K, Ashton-Miller JA, DeLancey JO (2014) The length of anterior vaginal wall exposed to external pressure on maximal straining MRI: relationship to urogenital hiatus diameter, and apical and bladder location. Int Urogynecol J 25:1349–1356
Hsu Y, Chen L, Summers A, Ashton-Miller JA, DeLancey JO (2008) Anterior vaginal wall length and degree of anterior compartment prolapse seen on dynamic MRI. Int Urogynecol J Pelvic Floor Dysfunct 19:137–142
Rapp DE, King AB, Rowe B, Wolters JP (2014) Comprehensive evaluation of anterior Elevate Ant system for the treatment of anterior and apical pelvic floor descent: 2-year followup. J Urol 191:389–394
Rogowski A, Bienkowski P, Tarwacki D, Szafarowska M, Samochowiec J, Sienkiewicz-Jarosz H, Jerzak M, Baranowski W (2015) Retrospective comparison between the Prolift and Elevate Anterior vaginal mesh procedures: 18-month clinical outcome. Int Urogynecol J 26:1815–1820
Moore RD, Beyer RD, Jacoby K, Freedman SJ, McCammon KA, Gambla MT (2010) Prospective multicenter trial assessing type I, polypropylene mesh placed via transobturator route for the treatment of anterior vaginal prolapse with 2-year follow-up. Int Urogynecol J 21(5):545–552
Rane A, Iyer J, Kannan K, Corstiaans A (2012) Prospective study of the Perigee™ system for treatment of cystocele – our five-year experience. Aust N Z J Obstet Gynaecol 52:28–33
Lo TS, Bt Karim N, Cortes EF, Wu PY, Lin YH, Tan YL (2015) Comparison between Elevate Anterior/apical system and Perigee system in pelvic organ prolapse surgery: clinical and sonographic outcomes. Int Urogynecol J 26:391–400
Letouzey V, Ulrich D, Balenbois E, Cornille A, de Tayrac R, Fatton B (2015) Utero-vaginal suspension using bilateral vaginal anterior sacrospinous fixation with mesh: intermediate results of a cohort study. Int Urogynecol J 26:1803–1807
McLennan GP, Sirls LT, Killinger KA, Nikolavsky D, Boura JA, Fischer MC et al (2013) Perioperative experience of pelvic organ prolapse repair with the Prolift and Elevate Ant vaginal mesh procedures. Int Urogynecol J 24:287–294
Deffieux X, Letouzey V, Savary D, Sentilhes L, Agostini A, Mares P et al (2012) Prevention of complications related to the use of prosthetic meshes in prolapse surgery: guidelines for clinical practice. Eur J Obstet Gynecol Reprod Biol 165:170–180
De Landsheere L, Ismail S, Lucot JP, Deken V, Foidart JM, Cosson M (2012) Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol 206:83.e1–83.e7
Halaska M, Maxova K, Sottner O, Svabik K, Mlcoch M, Kolarik D et al (2012) A multicenter, randomized, prospective, controlled study comparing sacrospinous fixation and transvaginal mesh in the treatment of posthysterectomy vaginal vault prolapse. Am J Obstet Gynecol 207:301.e1–301.e7
Acknowledgments
Sincere thanks to Dr. Muriel Rabilloud (biostatistician at Lyon University, France) for statistical analysis, and to Dr. Emile Simon (surgeon and Lyon Medical School anatomist at Lyon University) for Fig. 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
Laure Panel receives honoraria from AMS. Christophe Courtieu receives honoraria and payment for research from AMS. The other authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Lamblin, G., Gouttenoire, C., Panel, L. et al. A retrospective comparison of two vaginal mesh kits in the management of anterior and apical vaginal prolapse: long-term results for apical fixation and quality of life. Int Urogynecol J 27, 1847–1855 (2016). https://doi.org/10.1007/s00192-016-3045-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3045-1