Abstract
Purpose
The aim of this systematic review was to investigate the clinical and functional knee outcomes after Verasense sensor-assisted total knee arthroplasty (VA TKA), and to compare these outcomes, where possible, with those from manually balanced total knee arthroplasty (MB TKA).
Methods
A systematic literature search following PRISMA guidelines was conducted on PubMed, Embase, Medline and Scopus from the beginning of January 2012 until the end of June 2022, to identify potentially relevant articles for this review. Selection was based on the following inclusion criteria: full text English- or German-language clinical studies, published in peer-reviewed journals, which assessed clinical and functional outcomes following VA TKA. Not original research, preprints, abstract-only papers, protocols, reviews, expert opinion papers, book chapters, surgical technique papers, and studies pertaining only to unicondylar knee arthroplasty (UKA) or patellofemoral arthroplasty (PFA) were excluded. Several scores (Knee Society Score [KSS], Oxford Knee Score [OKS], Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC], Knee injury and Osteoarthritis Outcome Score—4 subscales [KOOS4] and Physical Function—Computerised Adaptive Testing [PF˗CAT]), alongside postoperative measurements of range of motion [ROM], reoperation rates and the rate of manipulation under anaesthesia [MUA]) were used to evaluate clinical and functional outcomes. The quality of included papers, except randomised control trials (RCTs), was evaluated using the Methodological Index for Non-Randomised Studies (MINORS). For the assessment of included RCTs, the Jadad Scale was used.
Results
The literature search identified 243 articles. After removing duplicates, 184 papers were included in the initial screening process. Fourteen of them met all the inclusion criteria following the selection process. Mean MINORS for non-comparative studies value was 11.5 (11–12), and for comparative studies 18.2 (13–21). Mean Jadad Scale score was 3.6 (2–5). Outcomes from a total number of 3633 patients were evaluated (mean age at surgery 68.5 years [32–88 years]). In terms of clinical outcomes, the overwhelming majority of studies observed an improvement after VA TKA, but no statistically significant difference in ROM and reoperation rate when compared to MB TKA. On the other hand, lower rates of MUA have been described in the VA TKA group. An increase in postoperative clinical and functional scores values, when compared to the preoperative ones, has been reported in both groups, although no statistically significant difference between them has been observed.
Conclusion
The use of Verasense pressure sensors in TKA leads to no significant improvement in ROM, reoperation rate or functional outcomes, when compared to the standard manually balancing technique. However, lower rates of MUA have been described in the VA TKA group. These findings highlight the importance of tools being able to measure ligament stresses or joint pressure for achieving an optimally balanced knee.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Achieving optimal clinical and functional outcomes after total knee arthroplasty (TKA) depends on a number of factors such as leg alignment, orientation of the components, as well as adequate soft tissue balancing [2, 9, 21, 24]. Assessing soft tissue balance is challenging for the surgeon, as the perceived “feeling for balance” is influenced by several elements such as surgical experience, patients’ body mass index (BMI), gender, soft tissue laxity, the degree of joint contracture, as well as the fitness level of the surgeon [14]. Consequently, this might lead to an unbalanced knee as well as further revisions, which both reduce the patients’ quality of life [11]. Hence, the development of new methods to assess intraoperative ligament laxity and balancing is important [28]. One of the current debated methods is the use of intraoperative sensor technology, which allows surgeons to dynamically quantify in vivo joint laxity and perform a more objective soft tissue balancing [26]. These sensors enable the surgeon to receive objective intraoperative digital feedback [17]. Intraoperative pressure sensors may play an important role in reducing dissatisfaction related to knee stiffness or instability [11]. Despite their ability to improve soft tissue balance, it is not clear whether the use of intraoperative sensors improve clinical and functional outcomes in TKA. Several studies have shown improved early outcomes with the use of sensors [8, 11, 12], whereas others have failed to demonstrate any clinical benefit [18, 25]. Although an optimal balance of the medial and lateral joint gaps in flexion and extension has been considered an important determinant of clinical and functional outcomes, improved outcomes when compared with TKAs that are not balanced, have not yet been proven [9, 17]. One of the commercially available intraoperative sensors is the Verasense sensor [17]. Due to its widespread use, and to the fact that the majority of the studies, which report on clinical and functional outcomes following sensor-assisted TKA, are using Verasense, the present study focuses on its use. The aim of this systematic review was to investigate the clinical and functional knee outcomes after Verasense sensor-assisted TKA (VA TKA) and to compare these outcomes where possible with those from manually balanced TKA (MB TKA). The hypothesis was VA TKA does yield satisfactory postoperative clinical and functional outcomes, but not superior to those after MB TKA.
Materials and methods
A systematic literature search was conducted on PubMed, Embase, Medline and Scopus to identify potentially relevant articles published between June 2012 and June 2022. Terms including “intraoperative sensor”, “sensor technology”, “sensor assisted”, “Verasense”, “pressure sensor”, “force sensor”, “sensor balancing”, “total knee arthroplasty”, “knee revision”, “knee replacement”, “revision arthroplasty”, “TKA” and “TKR” were searched for in both title and abstract. Detailed information regarding the used search strategy can be found in “Additional file 1”.
Inclusion criteria were full text English- or German-language clinical studies, published in peer-reviewed journals that assessed the clinical and functional outcomes following VA TKA. Only original research articles were considered. Preprints, abstract-only studies, protocols, reviews, expert opinion studies, book chapters, surgical technique studies, and studies pertaining only to unicondylar knee arthroplasty (UKA) or patellofemoral arthroplasty (PFA), were excluded. Only articles reporting clinical and functional knee outcomes after VA TKA were included.
After collecting all articles and removing duplicates, two authors screened the studies by title and abstract analysis for inclusion. In a second step, selected articles were checked for their eligibility by full text analysis. In case of uncertainty regarding inclusion a third author was consulted. A further manual screening of the reference lists of included articles was done for additional studies. For this review, only studies reporting clinical and functional outcomes were included. Endpoints included various postoperative patient-reported outcome measures (PROMs) such as Knee Society Score (KSS), Oxford Knee Score (OKS), Knee Injury and Osteoarthritis Outcome Score—4 Subscales (KOOS4), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Physical Function—Computerised Adaptive Testing (PF˗CAT), as well as range of motion (ROM), rate of arthrofibrosis and reoperation rate.
Quality assessment
The methodological quality of the included comparative and non-comparative non-randomised clinical studies was assessed by two raters independently, using the Methodological Index for Non-Randomised Studies (MINORS). The global ideal score is 16 for non-comparative studies, and 24 for comparative studies. For the assessment of included randomised control trials (RCTs), the Jadad Scale was used, with the maximum score being 5. The level of evidence of the included studies was also reported.
Data extraction
From the selected publications, title, author, year of publication, study design, level of evidence, number of knees, follow-up time, patient demographics, clinical outcome scores and functional outcomes were extracted.
Statistical analysis
Continuous variables were described with mean and standard deviation or median and range. Categorical variables were reported with absolute and relative frequencies. A p < 0.05 was considered statistically significant.
Results
Search results and characteristics of included studies
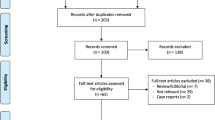
The literature search identified 243 scientific articles in the initial screening. A total of 11 met all the inclusion criteria following the selection process shown in Fig. 1 (Additional file 2). Median MINORS for non-comparative studies value was 11.5 (11–12), and for comparative studies 18.2 (13–21). Median Jadad Scale score was 3.6 (2–5). Results from a total number of 3633 patients were evaluated (median age at surgery 68.5 years, range 32–88 years). The reported median body mass index (BMI) was 30.8 (17–45). Several scores (KSS, OKS, WOMAC, KOOS4, PF˗CAT), alongside postoperative ROM, reoperation rates and the rate of manipulation under anaesthesia (MUA), were used to evaluate clinical and functional outcomes. The detailed characteristics of the included studies are presented in Table 1 (Additional file 3).
Clinical outcomes
ROM was evaluated in five studies (Table 1). They reported no statistically significant differences between the VA and MB groups [5, 7, 19, 25, 29]. Mean follow-up time ranged from 3 to 24 months.
Nine studies examined the rate of MUA as an assessment of postoperative arthrofibrosis (Table 2). Geller et al. reported that the rate of MUA in the MB TKA group was higher than in the VA TKA group, and that the period between TKA and MUA was on average 13.5 weeks and 7.5 weeks, respectively [15]. Some of the other studies also showed higher rates of MUA in the MB TKA group, but with no significant differences. The mean follow-up time ranged from 6 to 24 months [1, 3, 5, 7, 16, 18, 19, 25, 29].
Livermore et al. and MacDessi et al. reported the reoperation rate at a mean follow-up of 12 months and 24 months, respectively, with no significant differences [16, 18].
Patient-reported outcome measures
Four studies have evaluated pre- and postoperative KSS (Table 3). These studies showed improved postoperative KSS, for both groups (VA TKA and MB TKA), but with no significant differences between the analysed groups at 6 and 12 months [3, 5, 25].
Three studies evaluated pre- and postoperative OKS (Table 4). Although the 6-month OKS scores were higher in the VA TKA group (p = 0.01), no significant differences were found between the two groups at 1- and 2-year follow-ups [3, 5, 29].
Three studies have reported preoperative and 1- and 2-year postoperative KOOS and WOMAC after VA and MB TKA [16, 19, 25]. They described improved postoperative scores in both groups, but with no significant differences between them. Detailed information can be found in Table 5.
Discussions
The main findings of this study are that both VA TKA and MB TKA showed improved clinical and functional scores, but that there is no statistically significant difference in between VA TKA and MB TKA [5, 7, 19, 25, 29]. Similar findings were shown for PROMs (OKS, KSS, WOMAC, KOOS4 and PF-CAT) [5, 16, 18, 19, 25, 29]. There is only one exception, which has been also reported by Chow et al. who described a statistically significant difference (p < 0.025) in OKS at 6-month follow-up between VA TKA and MB TKA groups [3]. The VA TKA group scored higher (Δ17 vs Δ13). A similar difference for the KSS (Δ63 vs. Δ52) has also been shown by Chow et al. [3]. However, the findings although significant do not represent clinically relevant differences. In addition, in this study, only the mean change between preoperative OKS/KSS and 6-month postoperative OKS/KSS and not the absolute values were presented.
The most interesting finding of the present review is the fact that when no pressure sensors were used for TKA, the knee was more likely to undergo a manual manipulation [1, 3, 7, 16, 17, 19, 29]. However, although there was clear difference for a higher need for MUA in the conventional groups, the findings were not always statistically significant. This might be due to the laxity differences in the included knees. Many studies have just recently highlighted the importance of the envelope of laxity [9, 10]. In line with the ongoing knee phenotype discussion, with regards to alignment parameters, the identification of different knee phenotypes for the individual envelope of laxity has just begun [20, 27]. When having identified different knee laxity types, the question arises how to measure these pre-, intra- and postoperatively. Pre- and postoperatively stress radiographs might play a major role. Intraoperative sensor technology, navigational or robotic devices might also be helpful. However, all technologies available are still in the early childhood and needs to mature to make a real clinical impact in TKA. The biggest obstacle besides availability is questionable inter- and intra-observer reliability of all such tools, when measuring stress or pressure in the different joint compartments.
The findings of this review are in line with the findings of Sun et al. in their metanalysis [26]. The number of included studies was lower than in ours. Since then, many more studies have been published. Another difference lies in the availability and the language of the studies included. In the present review, no articles published in other languages aside English and German were included. In addition, the articles had to possess identification numbers (i.e. PID, DOI), or these had to be accessible (e.g. in online medical libraries [i.e. PubMed, Scopus, Embase, Medline, Google Scholar] and/or peer-reviewed journals).
This study presents a number of limitations. The low number of RCTs analysed in our review (i.e. three) combined with the inferior quality of some non-randomised clinical studies limits the level of evidence. The low number of enrolled patients in the majority of analysed studies could also play a major role as the ability to identify a statistically significant difference between study groups is heavily linked to the sample size. Although all present completed studies pertaining to this subject have been included, more RCTs and prospective studies are currently in different stages of completion [4, 23]. Their results are yet to be reported; thus, there is a possibility their future findings might not concur with ours. The variability between included studies regarding surgical techniques, type of prosthesis (i.e. cruciate retaining [CR] or posterior stabilised [PS]), endpoints, outcomes, follow-up periods and size of cohorts adds to the heterogeneity of the study samples. In addition, the follow-up period for these studies is relatively short, with no study analysing long-term outcomes (clinical or functional). In the end, this systematic review only assessed studies which included a certain type of intraoperative sensors (Verasense). Several other sensors are available on the market (e.g. eLibra, Omnibot), to which our findings may not apply [6, 15]. The number of available studies reporting on outcomes following these sensors is low though, and there is none comparing those outcomes to the ones following MB TKA. Therefore, inclusion of these studies in the review, and a subsequent comprehensive analysis of their findings, has not been performed.
Conclusion
The use of Verasense pressure sensors in TKA leads to no significant improvement in ROM, reoperation rate or functional outcomes, when compared to the standard manually balancing technique. However, lower rates of MUA have been described in the VA TKA group.
Data availability
Data is available on request in personal repository.
Abbreviations
- TKA:
-
Total knee arthroplasty
- BMI:
-
Body mass index
- VA:
-
Verasense assisted
- MB:
-
Manually balanced
- UKA:
-
Unicondylar knee arthroplasty
- PFA:
-
Patellofemoral arthroplasty
- PROMs:
-
Patient-reported outcome measures
- KSS:
-
Knee Society Score
- OKS:
-
Oxford Knee Score
- KOOS4:
-
Knee Injury and Osteoarthritis Outcome Score—4 subscales
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
- PF-CAT:
-
Physical Function—Computerised Adaptive Test
- ROM:
-
Range of motion
- MINORS:
-
Methodological Index for Non-Randomised Studies
- RCT:
-
Randomised control trial
- MUA:
-
Manipulation under anaesthesia
- CR:
-
Cruciate retaining
- PS:
-
Posterior stabilised
References
Amundsen S, Lee YY, González Della Valle A (2017) Algorithmic pie-crusting of the medial collateral ligament guided by sensing technology affects the use of constrained inserts during total knee arthroplasty. Int Orthop 41(6):1139–1145
Cho KJ, Seon JK, Jang WY, Park CG, Song EK (2018) Objective quantification of ligament balancing using VERASENSE in measured resection and modified gap balance total knee arthroplasty. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-018-2190-8
Chow JC, Breslauer L (2017) The use of intraoperative sensors significantly increases the patient-reported rate of improvement in primary total knee arthroplasty. Orthopedics 40(4):e648–e651. https://doi.org/10.3928/01477447-20170503-01
Clement ND, Bardgett M, Galloway S, Baron JY, Smith K, Weir DJ, Deehan DJ (2022) Robotic—and orthosensor-assisted versus manual (ROAM) total knee replacement: a study protocol for a randomised controlled trial. Trials. https://doi.org/10.1186/s13063-021-05936-9
Cochetti A, Ghirardelli S, Iannotti F, Giardini P, Risitano S, Indelli PF (2020) Sensor-guided technology helps to reproduce medial pivot kinematics in total knee arthroplasty. J Orthop Surg. https://doi.org/10.1177/2309499020966133
D’Angelo F, Binda T, Cherubino P (2013) Use of an electronic system for soft tissue balancing in primary total knee arthroplasty. Orthopedics 36(11):856–859
Geller JA, Lakra A, Murtaugh T (2017) The use of electronic sensor device to augment ligament balancing leads to a lower rate of arthrofibrosis after total knee arthroplasty. J Arthroplasty 32(5):1502–1504
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD et al (2019) Are patients more satisfied with a balanced total knee arthroplasty? J Arthroplasty 34(7):195–200
Graichen H, Luderer V, Strauch M, Hirschmann MT, Scior W (2022) Navigated, gap-balanced, adjusted mechanical alignment achieves alignment and balancing goals in a very high percentage but with partially non-anatomical resections. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07014-2
Graichen H, Lekkreusuwan K, Eller K, Grau T, Hirschmann MT, Scior W (2022) A single type of varus knee does not exist: morphotyping and gap analysis in varus OA. Knee Surg Sports Traumatol Arthrosc 30(8):2600–2608
Gustke KA, Golladay GJ, Roche MW, Jerry GJ, Elson LC, Anderson CR (2014) Increased satisfaction after total knee replacement using sensor-guided technology. Bone Joint J. 96-B(10):1333–1338
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty 29(5):955–960
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Adv Orthop. 2014:628695. https://doi.org/10.1155/2014/628695
Heesterbeek PJC, Haffner N, Wymenga AB, Stifter J, Ritschl P (2017) Patient-related factors influence stiffness of the soft tissue complex during intraoperative gap balancing in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(9):2760–2768
Kaneko T, Kono N, Mochizuki Y, Hada M, Toyoda S, Ikegami H, Musha Y (2020) The influence of tibiofemoral joint forces on patient-reported outcome measurements after bicruciate stabilized total knee arthroplasty. J Orthop Surg 28(2):2309499020915106. https://doi.org/10.1177/2309499020915106
Livermore AT, Erickson JA, Blackburn B, Peters CL (2020) Does the sequential addition of accelerometer-based navigation and sensor-guided ligament balancing improve outcomes in TKA? Bone Joint J. 102(6):24–30
MacDessi SJ, Wood JA, Diwan AD, Harris IA, Sensor Balance Study Group (2021) Surgeon-defined assessment is a poor predictor of knee balance in total knee arthroplasty: a prospective, multicenter study. Knee Surg Sports Traumatol Arthrosc 29(2):498–506
MacDessi SJ, Cohen DA, Wood JA, Diwan AD, Harris IA (2021) Does the use of intraoperative pressure sensors for knee balancing in total knee arthroplasty improve clinical outcomes? A comparative study with a minimum two-year follow-up. J Arthroplasty 36(2):514–519
MacDessi SJ, Wood JA, Diwan A, Harris IA, Sensor Balance Study Group (2022) Intraoperative pressure sensors improve soft-tissue balance but not clinical outcomes in total knee arthroplasty: a multicentre randomized controlled trial. Bone Joint J. 104-B(5):604–612
Moser LB, Hess S, de Villeneuve Bargemon JB, Faizan A, LiArno S, Amsler F, Hirschmann MT, Ollivier M (2022) Ethnical differences in knee phenotypes indicate the need for a more individualized approach in knee arthroplasty: a comparison of 80 Asian knees with 308 Caucasian knees. J Pers Med 12(1):121. https://doi.org/10.3390/jpm12010121
Ogawa H, Sengoku M, Shimokawa T, Nakamura Y, Ohnishi K, Matsumoto K, Akiyama H (2022) Extra-articular factors of the femur and tibia affecting knee balance in mechanically aligned total knee arthroplasty. Orthop Traumatol Surg 108(8):103297. https://doi.org/10.1016/j.otsr.2022.103297
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Sarpong NO, Held MB, Grosso MJ, Herndon CL, Santos W, Lakra A, Shah RP, Cooper HJ, Geller JA (2022) No benefit to sensor-guided balancing compared with freehand balancing in TKA: a randomized controlled trial. Clin Orthop Relat Res 480(8):1535–1544
Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT (2018) Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 26(6):1602–1609
Song SJ, Kang SG, Lee YJ, Kim KI, Park CH (2019) An intraoperative load sensor did not improve the early postoperative results of posterior-stabilized TKA for osteoarthritis with varus deformities. Knee Surg Sports Traumatol Arthrosc 27(5):1671–1679
Sun C, Zhao Z, Lee WG, Ma Q, Zhang X, Zhu J, Cai X (2022) Sensor-guided gap balance versus manual gap balance in primary total knee arthroplasty: a meta-analysis. J Orthop Surg Res 17:243. https://doi.org/10.1186/s13018-022-03129-x
von Eisenhart-Rothe R, Lustig S, Graichen H, Koch PP, Becker R, Mullaji A, Hirschmann MT et al (2022) A safe transition to a more personalized alignment in total knee arthroplasty: the importance of a “safe zone” concept. Knee Surg Sports Traumatol Arthrosc 30(2):365–367
Williams DP, O’Brien S, Doran E, Price AJ, Beard DJ, Murray DW, Beverland DE (2013) Early postoperative predictors of satisfaction following total knee arthroplasty. Knee 20(6):442–446
Wood TJ, Winemaker MJ, Williams DS, Petruccelli DT, Tushinski DM, de Beer JV (2021) Randomized controlled trial of sensor-guided knee balancing compared to standard balancing technique in total knee arthroplasty. J Arthroplasty 36(3):953–957
Acknowledgements
The authors would like to extend their thanks to Silvia Reichl, Iris Spörri and Felix Amsler, for offering their invaluable research knowledge as guidance, when conducting this systematic review.
Funding
Open access funding provided by University of Basel. This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: M-PS, HH, AL and MTH; methodology: M-PS and HH; data curation: M-PS, HH, AL and MTH; writing—original draft preparation: M-PS, HH and AL; writing—review and editing: MTH, M-PS, and HH; supervision: MTH and RWH; project administration: M-PS and HH. All the authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MTH is a consultant for Medacta™, Symbios™ and Depuy Synthes™. The rest of the authors declare no conflicts of interest.
Ethical approval
Ethical review and approval were waived for this study because unlike primary research, no new personal, sensitive or confidential information has been collected from participants. Only publicly available documents were used for the systematic review.
Informed consent
Due to the nature of the study, no “Informed Consent” was necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
167_2023_7352_MOESM2_ESM.docx
Supplementary file2 Flow-chart of the study selection process according to the PRISMA 2020 statement: an updated guideline for reporting systematic reviews [29]—available as Additional file 2 (DOCX 17 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sava, MP., Hara, H., Alexandra, L. et al. Verasense sensor-assisted total knee arthroplasty showed no difference in range of motion, reoperation rate or functional outcomes when compared to manually balanced total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 31, 1851–1858 (2023). https://doi.org/10.1007/s00167-023-07352-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07352-9