Abstract
Purpose
How much force is needed to pre-tension the ligaments during total knee arthroplasty? The goal of this study was to determine this force for extension and flexion, and for both compartments, and to identify predicting patient-related factors.
Methods
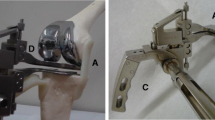
Eighty patients [55 females, mean age 71 (SD 9.7)] were recruited and had a navigated cruciate-retaining total knee arthroplasty. Distraction of the medial and lateral compartments of the extension and flexion gap (90°) with an instrumented bi-compartmental double-spring tensioner took place after finishing the bone cuts. Applied forces and resulting gap distances were recorded by the navigation system, resulting in a force–elongation curve. Lines were fitted with the intersection defined as the stiffness transition point. The slopes (N/mm) represented the stiffness of the ligamentous complex. Linear multiple regression analysis was performed to identify predicting factors.
Results
The amount of force at the stiffness transition point was on average 52.3 (CI95 50.7–53.9), 54.5 (CI95 52.7–56.3), 48.3 (CI95 46.2–50.2), and 59.3 (CI95 57.0–61.6) N for the medial and lateral extension and flexion gap, respectively, and varied considerably between patients. The force at the stiffness transition point was significantly different between extension and flexion and both compartments (P < 0.05). Stiffness of the ligaments statistically significantly helped to predict the amount of force at the stiffness transition point, as well as body mass index, gender, and varus–valgus alignment.
Conclusion
The amount of force at the stiffness transition point varies between 48 and 59 N, depending on flexion/extension and compartment. Patient-related factors influence the stiffness transition point and can help predict the stiffness transition point. When forces higher than 60 N are used for gap distraction, the ligamentous sleeve of the knee might be over-tensioned.
Level of evidence
Prognostic study, Level I—high-quality prospective cohort study with >80 % follow-up, and all patients enrolled at same time point in disease.




Similar content being viewed by others
References
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S, Tashiro Y, Iwamoto Y (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Wasielewski RC, Galat DD, Komistek RD (2005) Correlation of compartment pressure data from an intraoperative sensing device with postoperative fluoroscopic kinematic results in TKA patients. J Biomech 38:333–339
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Insall J, Scott WN, Ranawat CS (1979) The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am 61:173–180
Asano H, Hoshino A, Wilton TJ (2004) Soft-tissue tension total knee arthroplasty. J Arthroplasty 19:558–561
Asano H, Muneta T, Hoshino A (2008) Stiffness of soft tissue complex in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16:51–55
Gamada K, Jayasekera N, Kashif F, Fennema P, Schmotzer H, Banks SA (2008) Does ligament balancing technique affect kinematics in rotating platform, PCL retaining knee arthroplasties? A prospective randomized study. Knee Surg Sports Traumatol Arthrosc 16:160–166
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2006) Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng 128:867–871
Nowakowski AM, Majewski M, Muller-Gerbl M, Valderrabano V (2011) Development of a force-determining tensor to measure “physiologic knee ligament gaps” without bone resection using a total knee arthroplasty approach. J Orthop Sci 16:56–63
Swank M, Romanowski JR, Korbee LL, Bignozzi S (2007) Ligament balancing in computer-assisted total knee arthroplasty: improved clinical results with a spring-loaded tensioning device. Proc Inst Mech Eng H 221:755–761
Wyss T, Schuster AJ, Christen B, Wehrli U (2008) Tension controlled ligament balanced total knee arthroplasty: 5-year results of a soft tissue orientated surgical technique. Arch Orthop Trauma Surg 128:129–135
Nowakowski AM, Majewski M, Muller-Gerbl M, Valderrabano V (2012) Measurement of knee joint gaps without bone resection: “physiologic” extension and flexion gaps in total knee arthroplasty are asymmetric and unequal and anterior and posterior cruciate ligament resections produce different gap changes. J Orthop Res 30:522–527
Viskontas DG, Skrinskas TV, Johnson JA, King GJ, Winemaker MJ, Chess DG (2007) Computer-assisted gap equalization in total knee arthroplasty. J Arthroplasty 22:334–342
Zalzal P, Papini M, Petruccelli D, de Beer J, Winemaker MJ (2004) An in vivo biomechanical analysis of the soft-tissue envelope of osteoarthritic knees. J Arthroplasty 19:217–223
Woo SL, Debski RE, Withrow JD, Janaushek MA (1999) Biomechanics of knee ligaments. Am J Sports Med 27:533–543
Ritschl P, Fuiko R, Machacek F (2005) Evolution in ligament balancing surgical technique for TKR. From historical gap measurement via today’s force controlled gap balancing to tomorrows patient’s individual joint stability. Conference Proceeding. In: Computer Assisted Orthopaedic Surgery, pp 383–385
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y (2013) Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res 471:1334–1342
Heesterbeek PJC, Keijsers NL, Wymenga AB (2010) Ligament releases do not lead to increased postoperative varus-valgus laxity in flexion and extension: a prospective clinical study in 49 TKR patients. Knee Surg Sports Traumatol Arthrosc 18:187–193
Heesterbeek PJC, Verdonschot N, Wymenga AB (2008) In vivo knee laxity in flexion and extension: a radiographic study in 30 older healthy subjects. Knee 15:45–49
Ten Ham AM, Heesterbeek PJC, van der Schaaf DB, Jacobs WC, Wymenga AB (2013) Flexion and extension laxity after medial, mobile-bearing unicompartmental knee arthroplasty: a comparison between a spacer- and a tension-guided technique. Knee Surg Sports Traumatol Arthrosc 21:2447–2452
Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, Laprade RF (2010) Structural properties of the primary medial knee ligaments. Am J Sports Med 38:1638–1646
Bellemans J, D’Hooghe P, Vandenneucker H, Van Damme G, Victor J (2006) Soft tissue balance in total knee arthroplasty: does stress relaxation occur perioperatively? Clin Orthop Relat Res 452:49–52
Christen B, Neukamp M, Aghayev E (2012) No difference in anterior tibial translation with and without posterior cruciate ligament in less invasive total knee replacement. Knee Surg Sports Traumatol Arthrosc 20:503–509
Matsumoto T, Kubo S, Muratsu H, Matsushita T, Ishida K, Kawakami Y, Oka S, Matsuzaki T, Kuroda Y, Nishida K, Akisue T, Kuroda R, Kurosaka M (2013) Different pattern in gap balancing between the cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2338–2345
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38:1067–1074
Yoshino N, Watanabe N, Watanabe Y, Fukuda Y, Takai S (2009) Measurement of joint gap load in patella everted and reset position during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17:484–490
Komatsu T, Ishibashi Y, Otsuka H, Nagao A, Toh S (2003) The effect of surgical approaches and tourniquet application on patellofemoral tracking in total knee arthroplasty. J Arthroplasty 18:308–312
Herald J, Cooper L, Machart F (2002) Tourniquet-induced restriction of the quadriceps muscle mechanism. Fact or fiction? J Bone Joint Surg Br 84:856–857
Acknowledgments
Some financial support was provided by Smith and Nephew. Smith and Nephew had no involvement in the study design, data collection, analysis and interpretation, writing of the report, and in the decision to submit the article for publication. The authors wish to thank Noël Keijsers for his support in writing the data analysis software.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heesterbeek, P.J.C., Haffner, N., Wymenga, A.B. et al. Patient-related factors influence stiffness of the soft tissue complex during intraoperative gap balancing in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 2760–2768 (2017). https://doi.org/10.1007/s00167-015-3694-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3694-5