Abstract
Purpose
The purpose of this study was to evaluate the return to knee-strenuous sport rate, muscle function and subjective knee function among adolescent patients (15–20 years of age) and adult patients (21–30 years of age) 8 and 12 months, respectively, after anterior cruciate ligament (ACL) reconstruction. It was hypothesised that no differences in outcome would be found between age groups at 8 or 12 months after ACL reconstruction.
Methods
Cross-sectional data from five tests of muscle function, from the Knee injury and Osteoarthritis Outcome Score (KOOS) and the Tegner Activity Scale (Tegner), performed at 8 and 12 months after a primary ACL reconstruction, were extracted from a rehabilitation outcome register. A total of 270 (51% women) athletes, aged 15–30 years, who were all involved in knee-strenuous sport prior the injury, were included at 8 months after ACL reconstruction. At 12 months 203 (51% women) were included. The return to knee-strenuous-sport rates and the rate of achieving a limb symmetry index of ≥ 90% in all five tests of muscle function, defined as recovery of muscle function, and subjective knee function scores, as measured with the KOOS, were compared between age groups.
Results
The adolescent patients had a higher (50%) return to knee-strenuous sport rate compared with the adult patients (38%) 8 months after ACL reconstruction (p = 0.04). At the 12-month follow-up, no difference was found between the age groups; 74 and 63%, respectively. At the 8-month follow-up, 29% of the patients, in both age groups, who had returned to sport had recovered their muscle function in all five tests of muscle function. At the 12-month follow-up, the corresponding results were 20% for the adolescents and 28% for the adult patients. No difference in mean KOOS scores was found between the age groups at 8 or at 12 months after ACL reconstruction.
Conclusion
The majority of young athletes make an early return to knee-strenuous sport after a primary ACL reconstruction, without recovering their muscle function. To set realistic expectations, clinicians are recommended to ensure that young athletes receive information about not to return before muscle function is recovered and that this may take longer time than 12 months.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most devastating consequences when returning to sport (RTS) after anterior cruciate ligament (ACL) reconstruction is a subsequent ACL injury. Adolescent patients (15–20 years) run a remarkably increased risk of a second ACL injury; up to 30% will require a new ACL reconstruction within the first two years after RTS [1, 2, 13, 23, 27, 34, 36]. Two identified risk factors for an additional ACL reconstruction are primary ACL reconstruction at younger age, i.e., age < 20 years [9, 19, 20, 28], and higher activity level [2, 9, 19, 28, 36].
Recent studies have highlighted and discussed the importance of delaying RTS to at least 9 months to lower the risk of a subsequent ACL injury [14, 23]. Further, restoring muscle function before RTS is regarded as another important factor [14, 21] in lowering the re-injury risk. The limb symmetry index (LSI) is the most frequently reported criterion for assessing whether strength and hop performance is classified as normal or abnormal. An LSI of > 90% is commonly regarded as sufficient for both leg muscle strength and hop performance after ACL injury and reconstruction [4, 22, 31]. However, several studies report that many patients do not achieve this level in a combined battery of strength and hop tests 6–12 months after ACL reconstruction [11, 14, 17, 32, 35]. Younger age appears to favour returning to the pre-injury level of sport [3]. However, it has not previously been reported whether younger athletes (15–20 years old) recover their muscle function before they return to knee-strenuous sport.
Patients have been reported to have high expectations on the overall condition of the knee joint 12 months after an ACL reconstruction, especially younger patients, patients without previous knee surgery, and highly active patients [10]. Furthermore, patients who return to sport have been found to have less impairment during sport and recreation and enhanced knee-related quality of life after ACL reconstruction as compared to patients who do not return to sport [8, 16]. However, it is not known whether there is any discrepancy in subjective knee function between patients of different ages who return to sporting activities.
Taken together, patients under the age of 20 who are involved in knee-strenuous sport at the index ACL injury constitute a high-risk group in terms of sustaining a subsequent ACL injury. The timing of RTS and recovery of muscle function have been reported to be important aspects to consider in the RTS decision. To our knowledge, no previous study has evaluated these aspects specifically in adolescent patients. The purpose of this study was, therefore, to evaluate the return to knee-strenuous-sport rates, muscle function and subjective knee function among adolescent patients (15–20 years) and adult patients (21–30 years) 8 and 12 months, respectively, after ACL reconstruction. It was hypothesised that no differences in outcome would be found between the age groups at 8 or 12 months after ACL reconstruction.
Materials and methods
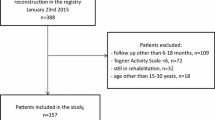
The study was performed as a prospective, observational register study based on data from a rehabilitation outcome register. The register is located in the western part of Sweden and was established in September 2014. At the end of March 2017, the register comprised more than 1,200 patients, of which 560 patients had undergone a unilateral ACL reconstruction and were between 15 and 30 years of age at the time of surgery (Fig. 1). The register consists of two parts: a battery of validated patient-reported outcome measurements (PROMs) and a battery of muscle function tests for leg-muscle strength and hop performance. Patients were regularly assessed according to a predefined schedule of follow-ups at 10 weeks, 4, 8, 12, 18 and 24 months and then every 5 years after their index ACL injury or reconstructive surgery. All patients were given written information about the study. Informed consent was obtained and the rights of subjects were protected.
Participants
Cross-sectional data from the 8- and 12-month follow-ups were extracted from the rehabilitation outcome register. Patients with a unilateral ACL injury who had undergone ACL reconstruction between September 2013 and July 2016 were eligible for inclusion. A further inclusion criterion was a pre-injury self-reported physical activity level on the Tegner Activity Scale (Tegner) [30] of ≥ 6, i.e., involvement in a knee-strenuous sport. A flow chart of the inclusion and exclusion criteria is presented in Fig. 1.
Procedure
Muscle function
Assessments of muscle strength were performed at the House of Sport Science, University of Gothenburg, by educated test administrators, all registered physiotherapists. Two methods of muscle strength assessment were used in this study. Initially, isometric tests were performed using a David F200 DMS-EVE (David Health Solutions Ltd, 2013, Finland) and these values contribute to about 30% of the total muscle strength data. The isometric test evaluated peak torque in knee extension at 60° of knee flexion and knee flexion at 30° of flexion. In December 2015, these tests were replaced by an isokinetic concentric strength test of knee extension and knee flexion using a Biodex System 4 (Biodex Medical Systems, Shirley, New York) [33]. Both versions of the strength test were performed according to a structured protocol, consisting of a 10-min warm-up on an exercise bike, followed by a warm-up procedure and familiarisation with sub-maximum practice trials. The isometric tests were performed unilaterally and the patients were instructed to extend/flex their knee with maximum effort for 2–4 s. The isokinetic tests were performed at an angular velocity of 90°/s after a warm-up protocol similar to that for the isometric tests. After warming up, 3–5 maximum isometric/isokinetic trials were performed with 40 s’ rest in between. For both tests, the best trial for extension and flexion torque for each leg was documented and used for further analysis.
After strength testing, three hop tests were performed in the following order: unilateral vertical hop; unilateral hop for distance; and unilateral side hop. High test–retest reliability for the three different tests in the battery of hop tests has been reported [15]. For the vertical hop and the hop for distance, the patients in the present study performed three to five practice trials, followed by three maximum trials. However, if the subject or the test administrator felt that an even better result could be achieved, one to two additional hops were allowed. The side hop was tested once and started with ten practice hops, followed by as many hops as possible for 30 s over two lines, 40 cm apart. Three minutes of rest were given between legs for the side-hop test [15]. The best trial for each leg in each test was used for further analysis.
Patient-reported outcome measurements
To assess the pre-injury and the present level of physical activity, the Tegner was used. The Tegner is graded from 1 to 10, with 1 representing the least strenuous knee activity and 10 representing the most strenuous knee activity, such as rugby and international soccer. The Tegner has been reported to have acceptable test–retest reliability (ICC = 0.8) [6]. In the present study, return to sport was defined as returning to a Tegner of 6 or higher, i.e., a knee-strenuous sport [16].
The Knee injury and Osteoarthritis Outcome Score (KOOS) [25] was used to assess patients’ opinions about their knee and associated problems. In the present study, the subscales of pain, other symptoms, function in sport and recreation and knee-related quality of life were used. The KOOS has been reported to have acceptable test–retest reliability with an ICC ranging from 0.85 to 0.93 for the subscales used in the present study [25].
Ethics Approval has been obtained from the Regional Ethical Review Board in Gothenburg, Sweden (registration numbers: 265-13, T023-17).
Statistics analysis
Statistical analysis was performed using the statistical package for the social sciences, SPSS (version 22, 2013; SPSS Inc., Chicago, IL, USA). The results of muscle function tests were presented as the LSI. The LSI was used to analyse results from the muscle function tests. The LSI was defined as the ratio of the injured side and the non-injured side expressed as a percentage. In this study, recovery of muscle function was defined as achieving an LSI of ≥ 90% in all tests of muscle function.
Descriptive statistics for patient demographics and outcomes were reported as the mean and standard deviation (SD) for parametric data and as the median, interquartile range and minimum and maximum for non-parametric data. For between-group comparisons, the Mann–Whitney U test and an independent t test were used for non-parametric and parametric data respectively. The Chi-square test was used to analyse associations between categorical variables.
A power analysis based on a previous study [32] suggested that 36 persons/group were needed for a power of 80% to detect a significant difference in knee extension strength, presented as LSI, between groups with a variance of 10% point and a significance level of 5%.
Results
A total of 270 (51% women) patients met the inclusion criteria at 8 months. At 12 months, 203 (51% women) patients were included. In all, 42% (114/270) and 67% (136/203) of the cohort reported that they had returned to knee-strenuous sport 8 and 12 months, respectively, after ACL reconstruction (Tables 1, 2).
At 8 months after ACL reconstruction, there was a significant difference in the return to knee-strenuous sport rate between the adolescent patients and the adult patients, 50 and 38%, respectively (p = 0.044). No significant difference in the return to knee-strenuous- sport rate was found between females and males among the adolescent patients (44 and 64%, respectively). However, among the adult patients, males had a significantly higher rate of return to knee-strenuous sport compared with females (45 and 27%, respectively; p = 0.019) (Table 2).
No significant difference was found in the rate of return to knee-strenuous sport between the adolescent patients and the adult patients at 12 months after ACL reconstruction, 74 and 63%, respectively. Furthermore, no difference in the return to knee-strenuous sport rate was found between males and females among either the adolescent or the adult patients.
In all, 29% of both the adolescent (13/45) and the adult patients (14/49), who had returned to knee-strenuous sport, achieved an LSI of ≥ 90% in all five tests of muscle function at 8 months after ACL reconstruction. At the 12-month follow-up, 20% of the adolescent patients (8/40) and 28% of the adult patients (17/60) (n.s.) achieved an LSI of ≥ 90% in all five tests of muscle function. No difference in the proportion of patients who achieved an LSI of ≥ 90% in all five tests of muscle function or in the mean LSI was found between the adolescent and the adult patients or between females and males in any age group in any of the separate tests in the test battery at either 8 or 12 months after ACL reconstruction (Tables 3, 4).
No differences in any of the KOOS subscales were seen between the adolescent and the adult patients who reported that they had returned to knee-strenuous sport, at 8 or at 12 months after ACL reconstruction (Tables 5, 6). Furthermore, no differences in any of the KOOS subscales were found between females and males in either the adolescent or the adult patients.
Discussion
The main finding in this prospective observational register study was that adolescent patients returned at a higher rate to knee-strenuous sport 8 months after ACL reconstruction compared with adult patients. Furthermore, fewer than 30% of all patients who had returned to knee-strenuous sport, at both follow-ups, achieved an LSI of ≥ 90% in all measurements in a battery of tests.
In the present study, there was a significant difference in the rate of return to knee-strenuous sport between adolescent and adult patients 8 months, but not 12 months, after ACL reconstruction. It has previously been reported that younger athletes are more likely to return to their pre-injury sport compared with their older counterparts 12 months after ACL reconstruction [3]. The difference in the result of the present study and the study by Ardern et al. [3] can be attributed to the fact that the present study only included young patients, aged 15–30 years, whereas Ardern et al. [3] based their systematic review on studies including patients up to 60 years of age. However, the present study indicates that the adolescent patients returned to knee-strenuous sport to a higher extent compared with the adult patients 8 months after the ACL reconstruction. It can be argued that the majority of the adolescent patients in the present study returned to knee-strenuous sport too early after ACL reconstruction. However, 8 months after ACL reconstruction, some patients are in a phase of rehabilitation where the transitioning to sport through sport-specific exercises, such as cutting and jumping, and gradual sports participation are commonly introduced or progress further in terms of intensity [4, 12, 29]. Some patients might even have begun to participate, at least in a modified manner, in knee-strenuous activities. There is a lack of evidence in the current literature with regard to adolescent patients in terms of the optimal progression of rehabilitation and the criteria patients need to meet before returning to unrestricted sports participation.
In the present study, only a minority, less than one-third, of both the adolescent and the adult patients achieved an LSI of ≥ 90% in all five tests of muscle function at 8 and 12 months after the ACL reconstruction. This is in line with previous studies reporting that 10–57% of patients achieve normal levels of muscle function [14, 32, 35] six to 12 months after ACL reconstruction. However, the apparent difference in the results of the present study and previous studies can be attributed to the younger population in the present study, including only patients who had returned to a knee-strenuous sport. Previous studies [11, 14, 17, 32, 35], as well as the present study, clearly demonstrate that the majority of the patients did not have recovered their muscle function once they returned to knee-strenuous sport after ACL reconstruction, in spite of the fact that the group’s mean LSIs are > 90% in all the individual tests in the battery. In a recently published study [35], the use of the LSI in RTS decisions has been questioned, as LSIs appear to overestimate knee function after ACL reconstruction and might not be sensitive enough to predict subsequent ACL injury. Furthermore, lower absolute levels of muscle function in the uninvolved leg might conceal an abnormal muscle function [18, 32]. Taken together, it appears that far too few patients have recovered their muscle function before returning to knee-strenuous sport. This is worrying and presents a major challenge that needs to be resolved. Considering the limitations of using the LSI, this problem can in fact be even worse. More effective rehabilitation and RTS criteria are suggestions of some areas that could be improved.
No difference in subjective knee function was found between the adolescent and the adult patients at either the 8- or the 12-month follow-up. No previous studies comparing adolescents and adults with respect to subjective knee function have been found. However, the results of the present study are in line with the results that have been suggested as a functional recovery among adult patients 12 months after ACL reconstruction, except for the KOOS subscale of knee-related quality of life [5, 24]. For this subscale, the patients in both age groups reported > 20-point lower scores at both the 8- and 12-month follow-up compared with scores that are considered to be equal to functional recovery. This could be an indication of a negative psychological response to the injury, the surgery, or the rehabilitation [7, 26]. However, knowledge of the psychological response in relation to return to sport among a young ACL population, aged < 20 years, is lacking.
Future studies may indicate whether the patients in the present study, who had returned to knee-strenuous sport as early as 8 months after ACL reconstruction, constitute a high-risk group for subsequent injuries. The high re-injury rate after ACL reconstruction among adolescent patients, as described in the literature [1, 2, 13, 23, 27, 34, 36], can be partly explained by the fact that the adolescent patients return to knee-strenuous sport too early, without achieving adequate muscle function.
This cross-sectional study has some limitations that were taken into account before conclusions were drawn. First, data relating to sport participation, as measured with Tegner, only reflect how knee strenuous the sports in which the patients participated actually were. Data relating to exposure, i.e., the frequency of participation, or whether the patients participated in modified or unrestricted training/competition, were not available. Second, two methods were used to assess the patients’ muscle strength. Both methods register peak torque at similar knee extension and flexion angles and in a similar seated position. Furthermore, the outcomes from the two methods are considered to be comparable, as they are presented as the LSI and not as absolute values. As a result, there is no reason to believe that this limits the opportunity to draw conclusions in the present study. Third, the adolescent patients comprised more women than men, as compared with the group of adults. However, a subgroup analysis of the adolescent and adult patients separately revealed no differences between genders in any of the outcome measurements. It was, therefore, assumed that the gender distribution in the present study did not limit the opportunity to draw conclusions. However, it is important to remember that the number of patients who performed the battery of tests was somewhat low when subgroups of ages were stratified by gender.
This is the first study to investigate differences in muscle function and subjective knee function between adolescents and adult patients who have undergone a primary ACL reconstruction. A large population of 270 and 203 young patients, respectively, was included at the two follow-ups. The patients were homogeneous in terms of age and pre-injury level of sport participation. Furthermore, the methods used for assessing strength and hop performance, as well the PROMs that were used, are all reliable and valid for evaluating patients after an ACL reconstruction.
Conclusions
The majority of young athletes make an early return to knee-strenuous sport after a primary ACL reconstruction, without recovering their muscle function. To set realistic expectations, clinicians are recommended to ensure that young athletes receive information about not to return before muscle function is recovered and that this may take longer time than 12 months.
Change history
16 November 2017
The author claims that his name is incorrectly listed on PubMed. The first name should be Eric and the last name should be Hamrin Senorski. On SpringerLink the name is listed correctly, but on PubMed he is listed as Senorski EH.
References
Allen MM, Pareek A, Krych AJ, Hewett TE, Levy BA, Stuart MJ et al (2016) Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med 44:2492–2498
Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K (2015) Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med 43:121–127
Ardern CL, Taylor NF, Feller JA, Webster KE (2014) Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 48:1543–1552
Barber-Westin SD, Noyes FR (2011) Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 27:1697–1705
Barenius B, Forssblad M, Engstrom B, Eriksson K (2013) Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 21:914–927
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37:890–897
Everhart JS, Best TM, Flanigan DC (2015) Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 23:752–762
Faltstrom A, Hagglund M, Kvist J (2015) Factors associated with playing football after anterior cruciate ligament reconstruction in female football players. Scand J Med Sci Sports. doi:10.1111/sms.12588
Faltstrom A, Hagglund M, Magnusson H, Forssblad M, Kvist J (2016) Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc 24:885–894
Feucht MJ, Cotic M, Saier T, Minzlaff P, Plath JE, Imhoff AB et al (2016) Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 24:201–207
Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D (2017) Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:192–199
Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I (2015) How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med 49:385–389
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. doi:10.1136/bjsports-2016-096031
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 50:804–808
Gustavsson A, Neeter C, Thomee P, Silbernagel KG, Augustsson J, Thomee R et al (2006) A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 14:778–788
Hamrin Senorski E, Samuelsson K, Thomee C, Beischer S, Karlsson J, Thomee R (2017) Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc 25:1364–1374
Herbst E, Hoser C, Hildebrandt C, Raschner C, Hepperger C, Pointner H et al (2015) Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery. Knee Surg Sports Traumatol Arthrosc 23:1283–1291
Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ (2000) Knee strength deficits after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Med Sci Sports Exerc 32:1472–1479
Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP (2015) Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med 43:1583–1590
Kvist J, Kartus J, Karlsson J, Forssblad M (2014) Results from the Swedish national anterior cruciate ligament register. Arthroscopy 30:803–810
Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E (2016) Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med 50:946–951
Lynch AD, Logerstedt DS, Grindem H, Eitzen I, Hicks GE, Axe MJ et al (2015) Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med 49:335–342
Nagelli CV, Hewett TE (2017) Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med 47:221–232
Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM (2006) Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord 7:38
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Ross CA, Clifford A, Louw QA (2017) Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother Theory Pract 33:103–114
Schilaty ND, Bates NA, Sanders TL, Krych AJ, Stuart MJ, Hewett TE (2017) Incidence of second anterior cruciate ligament tears (1990–2000) and associated factors in a specific geographic locale. Am J Sports Med 45:1567–1573
Shelbourne KD, Gray T, Haro M (2009) Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 37:246–251
Tagesson S, Oberg B, Good L, Kvist J (2008) A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med 36:298–307
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thomee R, Kaplan Y, Kvist J, Myklebust G, Risberg MA, Theisen D et al (2011) Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1798–1805
Thomee R, Neeter C, Gustavsson A, Thomee P, Augustsson J, Eriksson B et al (2012) Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:1143–1151
Undheim MB, Cosgrave C, King E, Strike S, Marshall B, Falvey E et al (2015) Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Br J Sports Med 49:1305–1310
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Wellsandt E, Failla MJ, Snyder-Mackler L (2017) Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. J Orthop Sports Phys Ther 47:334–338
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 44:1861–1876
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no conflict of interest.
Funding
This study was funded by Grants from the Swedish Research Council for Sport Science and by the Unit of Physiotherapy, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Beischer, S., Senorski, E.H., Thomeé, C. et al. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26, 1966–1974 (2018). https://doi.org/10.1007/s00167-017-4747-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4747-8