Abstract
Purpose
Controversy remains as to whether enteral supplementation of ω-3 fatty acids (FA) could improve outcomes in patients with acute respiratory distress syndrome (ARDS). Thus, we did a meta-analysis and aimed to investigate the benefit and harm of enteral ω-3 FA supplementation in adult patients with ARDS.
Methods
Databases including PubMed, Embase, the Cochrane Register of Controlled Trials, and Google Scholar were searched to find relevant articles. Randomized controlled trials (RCTs) comparing enteral ω-3 FA supplementation with a control or placebo intervention in adult patients with ARDS were included. The primary outcome was all-cause 28-day mortality. We used the Cochrane Collaboration methodology.
Results
Seven RCTs with 955 adult patients qualified for inclusion, and all the selected trials were considered as at high risk of bias. The use of enteral ω-3 FA did not significantly reduce all-cause 28-day mortality [relative risk (RR), 0.90; 95 % confidence intervals (CI), 0.68–1.18; p = 0.44; I 2 = 31 %; random effects]. Trial sequential analysis indicated lack of firm evidence for a 20 % RR reduction in all-cause 28-day mortality. PaO2/FiO2 ratio was significantly increased in the ω-3 FA group on day 4 [weighted mean difference (WMD), 45.14; 95 % CI, 16.77–73.51; p = 0.002; I 2 = 86 %; random effects] and day 7 (WMD, 33.10; 95 % CI, 1.67–64.52; p = 0.04; I 2 = 88 %; random effects). Meta-analysis using a random effects model showed no significant differences in ventilator-free days (VFD) (WMD, 2.47 days; 95 % CI, −2.85 to 7.79; p = 0.36; I 2 = 91 %) or intensive care unit-free days (ICU) (WMD, 2.31 days; 95 % CI, −2.34 to 6.97; p = 0.33; I 2 = 89 %) between the two groups.
Conclusions
Among patients with ARDS, enteral supplementation of ω-3 FA seemed ineffective regarding all-cause 28-day mortality, VFD, and ICU-free days. Routine use of enteral ω-3 FA cannot be recommended based on the available evidence.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is an acute life-threatening respiratory failure due to lung injury from a variety of critical illnesses, including sepsis, pneumonia, pancreatitis, and trauma [1]. ARDS is characterized by diffuse lung inflammation, increased alveolar-capillary membrane permeability, and pulmonary edema leading to the clinical manifestation of decreased lung compliance, decreased oxygenation (partial pressure of arterial oxygen to fraction of inspired oxygen [PaO2/FiO2] ≤300 with positive end-expiratory pressure [PEEP] ≥5 cmH2O), bilateral opacities on chest imaging [2]. Despite recent advances in overall support, ARDS still presents a high mortality rate of ~30 % [3, 4]. In the United States, ARDS causes 74,500 deaths each year [5]. Therefore, the development of effective therapy has important implication for the planning of critical care services, rehabilitation, and resource provision.
Nutritional input has been increasingly valued in critically ill patients, and early enteral nutrition is generally advised [6]. Enteral supplementation with ω-3 fatty acids (FA), such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), is thought to be beneficial in modulating the inflammatory processes [7]. Pontes-Arruda et al. [8] published a meta-analysis of trials conducted in patients with acute lung injury (ALI)/ARDS and found that enteral supplementation with ω-3 FA and γ-linolenic acid (GLA) could result in a significant reduction in the risk of mortality, duration of mechanical ventilation, and intensive care unit (ICU) stay. However, interpretation of these results is limited by small sample sizes and per-protocol analyses. Moreover, several recent randomized controlled trials (RCTs) reported conflicting findings, and the benefit and harm of enteral ω-3 FA is still uncertain [9–12].
We therefore conducted an updated systematic review of RCTs with meta-analysis and trial sequential analysis (TSA) to investigate the clinical efficacy and safety of enteral ω-3 FA supplementation in adult patients with ARDS.
Materials and methods
We followed the recommendations of the Cochrane handbook for systematic reviews of interventions and the preferred reporting Items for systematic reviews and meta-analyses (PRISMA) during all stages of the design, implementation and reporting of this meta-analysis [13, 14]. There was no formal protocol for this systematic review.
Search strategy and eligibility criteria
Two authors independently searched the following databases without language restrictions (updated to November 2013): Pubmed, Embase, and the Cochrane Register of Controlled Trials. The electronic search strategy combined terms related to omega-3 fatty acid (including MeSH search using exp “Fatty Acids, Omega-3”, and keyword search using words “omega-3 fatty acid”, “fish oil”, “unsaturated fatty acid”, “eicosapentaenoic acid”, “docosahexaenoic acid”) and terms related to acute respiratory distress syndrome (including MeSH search using exp “respiratory distress syndrome, adult”, and keyword search using words “acute respiratory distress syndrome”, “ARDS”, “ALI”, “acute lung injury”). We also checked the reference lists of RCTs and previous meta-analyses identified by the previous searches to include other potentially eligible trials. In addition, we reviewed the cited lists of eligible articles by Google Scholar to ensure that all appropriate studies were included.
Two authors independently included studies in the analysis if they met the following criteria: (1) study design: RCT; (2) population: adult patients (18 years or older) with ARDS (according to the Berlin Definition) [2]; (3) intervention: enteral supplementation of ω-3 FA compared with a control or placebo intervention; (4) outcome measures: all-cause 28-day mortality, ventilator-free days (VFD), ICU-free days, oxygenation status, and adverse events (as defined by the included trials). Studies were excluded if ω-3 FA were given for <24 h duration.
Data extraction
Using a predesigned data collection form and working in duplicate, two authors independently extracted the following data from each study: first author, year of publication, study design, patient characteristics, study methodology (e.g., inclusion/exclusion criteria, enteral nutrition [EN] administration protocol, and method of randomization and blinding), intervention (e.g., duration, form, and daily dose), and outcome measures. Authors of the included studies were contacted via E-mail if further study details were needed. Extracted data were checked by the third author, and any discrepancy was resolved by discussion.
Our primary outcome was all-cause 28-day mortality. Secondary outcomes included VFD and ICU-free days during the first 28 or 30 days, oxygenation status (defined by the PaO2/FiO2 ratio), and adverse events.
Assessment of risk bias
Methodological quality assessment was independently performed by two of the authors, and any disagreement was resolved by consensus. The risk of bias was assessed by using the components recommended by the Cochrane Collaboration: random sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; selective reporting; and other sources of bias [13]. Trials with high or unclear risk for bias for any one of the above components were considered as at high risk of bias. Otherwise, they were considered as low risk of bias.
Statistical analysis
The analyses were performed in Stata 11.2 (Stata Corporation, College Station, TX), RevMan 5.2 (The Nordic Cochrane Centre, Copenhagen, Denmark), and TSA 0.9 (The Copenhagen Trial Unit, Copenhagen, Denmark). We estimated the relative risk (RR) with 95 % confidence intervals (CI) for dichotomous outcomes, and the weighted mean difference (WMD) with 95 % CI for continuous outcomes. We used a fixed effect model if no statistical heterogeneity was present (I 2 = 0) and used both fixed effect model and random effects model in case of heterogeneity (I 2 > 0). Heterogeneity was expressed as the I 2 statistic, and I 2 > 50 % indicated significant heterogeneity [15].
To identify potential sources of heterogeneity, we a priori defined a hypothesis: the type of control formula (larger effect in trials using high-fat control formula vs. trials using lipid-poor control formula). This subgroup analysis allowed evaluating the effect of high-fat control formula which was high in pro-inflammatory ω-6 FA [16]. We estimated the difference between the estimates of the subgroups according to tests for interaction [17]. The p value <0.05 indicates that the effects of treatment differ between the tested subgroups.
The influence of trials with zero events in the treatment or control group was assessed by recalculating the meta-analyses with 0.5 empirical continuity corrections [18].
Meta-analyses may result in type I errors due to an increased risk of random error when few data are collected and due to repeated significance testing when a cumulative meta-analysis is updated with new trials [19]. We conducted TSA to reduce the risk of random error. TSA combines information size estimation for meta-analysis (cumulated sample size of included trials) with an adjusted threshold (trial sequential monitoring boundaries) for statistical significance in the cumulative meta-analysis. The idea in TSA is that if the cumulative Z-curve crosses the trial sequential monitoring boundary, a sufficient level of evidence has been reached and no further trials are needed. If the Z-curve does not cross the boundary and the required information size has not been reached there is insufficient evidence to reach a conclusion. The TSA was performed with a desire to maintain a type I error of 5 %, and we calculated the required information size [that is, the meta-analysis information size needed to detect or reject an anticipated intervention effect of a 20 % relative risk reduction (RRR) in all-cause 28-day mortality, with a risk of type II error of 20 %, at a power of 80 %] [20].
Graphic exploration with funnel plot was used to evaluate the small trial bias visually. The Egger’s test was used to assess small trial bias statistically. Results were considered as statistically significant for p < 0.05.
Results
Study selection
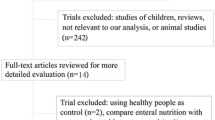
A total of 2,225 studies were retrieved, and 7 RCTs with a total of 955 adult patients qualified for inclusion (eFig. 1 in supplementary material) [9–12, 21–23]. The two authors had no disagreements for study selection.
Among these trials, four were conducted in North America [10–12, 21], and one each in Brazil [22], Israel [23], and Spain [9]. Five trials were multicenter studies [9–12, 21]. The mean age of the patients ranged from 49 to 66 years. Severity of illness at baseline was objectively defined by six trials using internationally recognized scoring systems [9–12, 22, 23]. All included trials reported the PaO2/FiO2 ratio at baseline and EN administration protocols. One trial used ω-3 FA alone [11], while six trials used ω-3 FA combined with GLA and antioxidants [9, 10, 12, 21–23]. Four trials used high-fat control EN [12, 21–23], and three trials used lipid-poor control EN or placebo [9–11]. The characteristics of the included trials are shown in Table 1.
Risk of bias in included studies
Among all the selected trials, randomized sequence and allocation sequence concealment were conducted adequately. Blinding was well conducted in five of seven trials [10–12, 21, 22], while two trials were open-label [9, 23]. Four trials were judged as being at high risk of attrition bias because they did not perform an intention-to-treat (ITT) analysis [9, 12, 22, 23]. One trial was at high risk of reporting bias because the outcomes were reported with inadequate detail [12]. Four trials were at high risk of other sources of bias because they had baseline imbalance [10, 11, 21, 23]. All the selected trials were considered as at high risk of bias (eTable 1 in supplementary material).
Primary outcome
In meta-analysis of seven trials with 955 participants, the use of enteral ω-3 FA did not significantly reduce all-cause 28-day mortality [RR (fixed effect), 0.90; 95 % CI, 0.73–1.12; p = 0.36; I 2 = 31 %; and RR (random effects), 0.90; 95 % CI, 0.68–1.18; p = 0.44] (Fig. 1).
Secondary outcomes
On the basis of the meta-analysis of four trials with 561 participants [10, 11, 21, 22], the use of enteral ω-3 FA increased both VFD (WMD, 1.83 days; 95 % CI, 0.24–3.42; p = 0.02; I 2 = 91 %) and ICU-free days (WMD, 1.72 days; 95 % CI, 0.21–3.23; p = 0.03; I 2 = 89 %) significantly in a fixed effect model, but these findings were associated with significant heterogeneity. When analysed in a random effects model, these significant effects were no longer present [WMD (VFD), 2.47 days; 95 % CI, −2.85 to 7.79; p = 0.36; and WMD (ICU-free days), 2.31 days; 95 % CI, −2.34 to 6.97; p = 0.33] (Table 2).
Six trials reported PaO2/FiO2 ratio at baseline (n = 789), day 4 (n = 615), and day 7 (n = 448) [9–11, 21–23]. No significant difference was detected between the groups at baseline [WMD (fixed effect), −5.62; 95 % CI, −11.58 to 0.34; p = 0.06; I 2 = 14 %; and WMD (random effects), −7.08; 95 % CI, −14.64 to 0.48; p = 0.07]. In contrast to control group, the PaO2/FiO2 ratio was significantly increased in the ω-3 FA group on day 4 [WMD (fixed effect), 65.74; 95 % CI, 59.86–71.61; p < 0.00001; I 2 = 86 %; and WMD (random effects), 45.14; 95 % CI, 16.77–73.51; p = 0.002] and day 7 [WMD (fixed effect), 58.46; 95 % CI, 50.62–66.31; p < 0.00001; I 2 = 88 %; and WMD (random effects), 33.10; 95 % CI, 1.67–64.52; p = 0.04], but these findings were associated with significant heterogeneity.
Table 3 gives details of adverse events. 5 trials involving 743 participants reported adverse events [9–11, 21, 22], including gastrointestinal events, cardiac events, respiratory disorders, hematologic disorders, and nosocomial infections. Since adverse events were variably reported, we did not combine these data.
Subgroup analysis
For outcomes of mortality, VFD, ICU-free days, PaO2/FiO2 ratio on day 4, and PaO2/FiO2 ratio on day 7, significant differences were observed between trials using high-fat control formula and trials using lipid-poor control formula by the test of interaction (random effects model, p = 0.009, 0.0006, 0.0007, 0.002, and 0.007, respectively). Larger effect was found in trials using high-fat control formula. Heterogeneity was decreased in these subgroup analyses (eTable 2 in supplementary material). For PaO2/FiO2 ratio at baseline, there was no significant interaction (random effects model, p = 0.84).
Sensitivity analysis
We included one trial with zero mortality in one arm [12]. To account for the potential influence of this trial, we calculated the RR with 0.5 as empirical continuity corrections. The fixed effect and random effects model RRs for the continuity corrections were: 0.9 (95 % CI, 0.73–1.12); 0.9 (95 % CI, 0.68–1.19), respectively.
TSA
For all-cause 28-day mortality, the required diversity (D 2 = 40 %, model variance based) adjusted information size (3,496 participants) was calculated based on a proportion of 26 % events in the control group, an RRR of 20 %, a type I error of 5 %, and a type II error of 80 %. The cumulative Z-curve did not crossed the trial sequential monitoring boundary and the required information size was not reached, suggesting a lack of firm evidence for an intervention effect of 20 % a RRR (Fig. 2). Only 27 % (955/3,496 patients) of the required information size was accrued.
Small trial bias
The funnel plot for mortality was symmetrical, indicating that small trial bias is unlikely to have had a major influence on the analysis of mortality (eFig. 2 in supplementary material). Furthermore, Egger’s test did not indicate significant small trial bias (p = 0.76).
Discussion
In the present systematic review using meta-analysis and TSA on enteral ω-3 FA supplementation in adult ARDS patients, enteral ω-3 FA supplementation was not statistically significantly different from placebo or control in terms of all-cause 28-day mortality, VFD and ICU-free days.
Differences between the current study and the previous one conducted by Pontes-Arruda et al. [8] should be noted. In their meta-analysis, only three trials with a total of 296 evaluable patients were included [21–23], which might have led to the indefinite conclusion. In addition, two included trials did not carry out analyses in an ITT manner [22, 23], thereby producing a potential for attrition bias. In our meta-analysis, seven trials with 955 patients were included, and analysis of the primary outcome was on an ITT basis. We also performed TSA to prevent premature statements of superiority or inferiority of the enteral ω-3 FA supplementation.
Our meta-analysis indicated that all-cause 28-day mortality was not significantly reduced by the enteral ω-3 FA supplementation, which was not in line with the result of Pontes-Arruda et al. [8]. There are several possible explanations for this discrepancy. First, the result of our meta-analysis was based on seven trials, whereas Pontes-Arruda et al. [8] included only three trials. Second, our meta-analysis included three trials (n = 522) which used a lipid-poor formula or placebo in the control group, while all three trials included in previous meta-analysis used an isonitrogenous-isocaloric high-fat formula as a control. This control formula contained predominately ω-6 FA to match the percentage of calories from fat, protein, and carbohydrate in the ω-3 FA formula. The high-fat formula is not standard of care in patients with acute respiratory failure, and it is richer in lipids than most of the currently used formula [6]. It is possible that the high-fat formula may be pro-inflammatory and alter pulmonary gas exchange, resulting in worsened clinical outcomes in the control group [24, 25]. Mortality of the control group in the trials using high-fat formula ranged 12.5–54.0 %, whereas mortality of the control group ranged 13.2–20.4 % in the trials using lipid-poor formula or placebo. In the subgroup analysis, significant interaction was observed between trials using high-fat control formula and trials using lipid-poor control formula, and ω-3 FA was associated with greater benefit in trials using high-fat control formula.
The results of TSA revealed absence of firm evidence for a 20 % RRR in all-cause 28-day mortality with enteral ω-3 FA supplementation. Mortality for ARDS has declined during the past two decades [26]. The decrease in mortality may have been a result of improvement in the management of patients, such as lung protective ventilation, prone positioning, conservative fluid management, and early antibiotics [27].
In the present meta-analysis, PaO2/FiO2 ratio was significantly increased in the ω-3 FA group on day 4, but the increase of PaO2/FiO2 ratio became marginally significant on day 7. In ARDS, one of the primary therapeutic goals is to increase oxygenation by reducing pulmonary inflammation, and it has been postulated that the inflammatory response might be modulated by nutritional substrates [28]. EPA and DHA can reduce inflammatory eicosanoid production and blunt the inflammatory response [29]. Consequently, it is plausible that supplementation with ω-3 FA could result in improvement of oxygenation status. However, the improved PaO2/FiO2 ratio did not accompany with an increase in VFD or ICU-free days. The PaO2/FiO2 ratio is a surrogate outcome measure which often tends to overestimate an intervention effect [30]. Thus, the short-term improvement in PaO2/FiO2 ratio might not be a reliable prediction of intervention benefit.
It is important to evaluate the safety of enteral ω-3 FA supplementation. In the included trials, enteral ω-3 FA supplementation was well tolerated without severe adverse events. Diarrhea is one of the most frequent adverse events associated with enteral ω-3 FA, and diarrhea rate of the ω-3 FA group ranged from 10 to 28.7 %.
On the basis of three trials [21–23], the Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN) provided a grade A recommendation to endorse the use of enteral ω-3 FA, GLA and antioxidants in the treatment of ARDS [6]. However, the results of the present study call into question the foundations of this recommendation. Given the lack of firm evidence for clinical benefits of enteral ω-3 FA supplementation, the current ASPEN guidelines might need to be reconsidered.
A strength of our systematic review was the TSA we performed. By using TSA we have demonstrated that the quantity of evidence on enteral ω-3 FA supplementation in adult ARDS patients is low. Another strength was that we conducted this systematic review with methodology following the recommendations of the Cochrane Collaboration. However, some limitations of this meta-analysis should be considered. First, there was considerable heterogeneity among the included trials. The included trials differed in EN formula, En administration, and treatment protocol. The primary cause of ARDS varied, including pneumonia, sepsis, aspiration, and trauma. Thus, caution should be taken when interpreting the results. Second, all the included trials were at high risk of bias and potentially prone to bias. Finally, the lack of a protocol could increase the risk of bias.
Conclusions
This systematic review using meta-analysis and TSA has demonstrated that the quality and quantity of evidence for the use of enteral ω-3 FA supplementation in adult ARDS patients is low and there is no firm evidence for benefit or harm as compared to placebo or control. Its routine use cannot be recommended based on the available evidence. Future large-scale, high-quality RCTs are still required to clarify the effectiveness of enteral ω-3 FA supplementation in ARDS.
References
Villar J, Pérez-Méndez L, Blanco J, Añón JM, Blanch L, Belda J, Santos-Bouza A, Fernández RL, Kacmarek RM (2013) Spanish Initiative for Epidemiology, Stratification, and Therapies for ARDS (SIESTA) Network: A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting––a prospective, multicenter validation study. Intensive Care Med 39(4):583–592
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM (2012) The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 38:1573–1582
Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP (2005) Causes and timing of death in patients with ARDS. Chest 128:525–532
Villar J, Blanco J, Anon JM, Santos-Bouza A, Blanch L, Ambros A, Gandia F, Carriedo D, Mosteiro F, Basaldua S, Fernandez RL, Kacmarek RM (2011) The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med 37:1932–1941
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G (2009) Guidelines for the provision and assessment of nutrition support therapy in the adult critically III patient: society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 33:277–316
Pacht ER, DeMichele SJ, Nelson JL, Hart J, Wennberg AK, Gadek JE (2003) Enteral nutrition with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants reduces alveolar inflammatory mediators and protein influx in patients with acute respiratory distress syndrome. Crit Care Med 31:491–500
Pontes-Arruda A, Demichele S, Seth A, Singer P (2008) The use of an inflammation-modulating diet in patients with acute lung injury or acute respiratory distress syndrome: a meta-analysis of outcome data. JPEN J Parenter Enteral Nutr 32:596–605
Grau-Carmona T, Moran-Garcia V, Garcia-de-Lorenzo A, Heras-de-la-Calle G, Quesada-Bellver B, Lopez-Martinez J, Gonzalez-Fernandez C, Montejo-Gonzalez JC, Blesa-Malpica A, Albert-Bonamusa I, Bonet-Saris A, Herrero-Meseguer JI, Mesejo A, Acosta J (2011) Effect of an enteral diet enriched with eicosapentaenoic acid, gamma-linolenic acid and anti-oxidants on the outcome of mechanically ventilated, critically ill, septic patients. Clin Nutr 30:578–584
Rice TW, Wheeler AP, Thompson BT, deBoisblanc BP, Steingrub J, Rock P (2011) Enteral omega-3 fatty acid, gamma-linolenic acid, and antioxidant supplementation in acute lung injury. JAMA 306:1574–1581
Stapleton RD, Martin TR, Weiss NS, Crowley JJ, Gundel SJ, Nathens AB, Akhtar SR, Ruzinski JT, Caldwell E, Curtis JR, Heyland DK, Watkins TR, Parsons PE, Martin JM, Wurfel MM, Hallstrand TS, Sims KA, Neff MJ (2011) A phase II randomized placebo-controlled trial of omega-3 fatty acids for the treatment of acute lung injury. Crit Care Med 39:1655–1662
Elamin EM, Miller AC, Ziad S (2012) Immune enteral nutrition can improve outcomes in medical-surgical patients with ARDS: a prospective randomized controlled trial. J Nutr Disord Ther 2:109. doi:10.4172/jndt.1000109
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration. http://handbook.cochrane.org. Accessed 28 Jan 2014
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Calder PC (2010) The 2008 ESPEN Sir David Cuthbertson Lecture: fatty acids and inflammation––from the membrane to the nucleus and from the laboratory bench to the clinic. Clin Nutr 29:5–12
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326:219
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23:1351–1375
Brok J, Thorlund K, Gluud C, Wetterslev J (2008) Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol 61:763–769
Wetterslev J, Thorlund K, Brok J, Gluud C (2009) Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol 9:86
Gadek JE, DeMichele SJ, Karlstad MD, Pacht ER, Donahoe M, Albertson TE, Van Hoozen C, Wennberg AK, Nelson JL, Noursalehi M (1999) Effect of enteral feeding with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants in patients with acute respiratory distress syndrome. Enteral Nutrition in ARDS Study Group. Crit Care Med 27:1409–1420
Pontes-Arruda A, Aragao AM, Albuquerque JD (2006) Effects of enteral feeding with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants in mechanically ventilated patients with severe sepsis and septic shock. Crit Care Med 34:2325–2333
Singer P, Theilla M, Fisher H, Gibstein L, Grozovski E, Cohen J (2006) Benefit of an enteral diet enriched with eicosapentaenoic acid and gamma-linolenic acid in ventilated patients with acute lung injury. Crit Care Med 34:1033–1038
Manzanares W, Dhaliwal R, Jurewitsch B, Stapleton RD, Jeejeebhoy KN, Heyland DK (2013) Alternative lipid emulsions in the critically ill: a systematic review of the evidence. Intensive Care Med 39:1683–1694
Lekka ME, Liokatis S, Nathanail C, Galani V, Nakos G (2004) The impact of intravenous fat emulsion administration in acute lung injury. Am J Respir Crit Care Med 169:638–644
Zambon M, Vincent JL (2008) Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest 133:1120–1127
Antonelli M, Bonten M, Chastre J, Citerio G, Conti G, Curtis JR, De Backer D, Hedenstierna G, Joannidis M, Macrae D, Mancebo J, Maggiore SM, Mebazaa A, Preiser JC, Rocco P, Timsit JF, Wernerman J, Zhang H (2012) Year in review in Intensive Care Medicine 2011: III. ARDS and ECMO, weaning, mechanical ventilation, noninvasive ventilation, pediatrics and miscellanea. Intensive Care Med 38:542–556
Umezawa Makikado LD, Flordelís Lasierra JL, Pérez-Vela JL, Montejo González JC (2013) Nutrition support during extracorporeal membrane oxygenation (ECMO) in adults. Intensive Care Med 39(12):2240
Giudetti AM, Cagnazzo R (2012) Beneficial effects of n-3 PUFA on chronic airway inflammatory diseases. Prostaglandins Other Lipid Mediat 99:57–67
Ciani O, Buyse M, Garside R, Pavey T, Stein K, Sterne JA, Taylor RS (2013) Comparison of treatment effect sizes associated with surrogate and final patient relevant outcomes in randomised controlled trials: meta-epidemiological study. BMJ 346:f457
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. Zhu, Y. Zhang, S. Li contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, D., Zhang, Y., Li, S. et al. Enteral omega-3 fatty acid supplementation in adult patients with acute respiratory distress syndrome: a systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Intensive Care Med 40, 504–512 (2014). https://doi.org/10.1007/s00134-014-3244-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3244-5