Abstract
Aims/hypothesis
Formation of epiretinal membranes (ERMs) in the posterior fundus results in progressive deterioration of vision. ERMs have been associated with numerous clinical conditions including proliferative diabetic retinopathy (PDR), but its pathogenic mechanisms are still unknown. This study was conducted to examine whether or not nuclear factor kappa B (NF-κB), a transcription factor that can be activated by various pathological conditions, is involved in the formation of ERMs after PDR.
Methods
ERM samples were obtained by vitrectomy from 22 cases with PDR aged 56±11 years with 18±10 years of diabetes and 15 cases with idiopathic ERM. They were processed for reverse transcription-polymerase chain reaction (RT-PCR) analysis. In addition, 5 ERM samples from PDR patients aged 51±16 years with 15±6 years of diabetes were processed for immunohistochemical analysis.
Results
NF-κB mRNA expression levels were higher (20 out of 22 cases vs. 9 out of 15 subjects in idiopathic ERM, p <0.05) in PDR subjects. Immunohistochemical analysis showed NF-κB protein expression in all the 5 ERMs derived from PDR patients, and that region was partially double-labelled with interleukin-8 (IL-8) and von Willebrand factor (vWF).
Conclusions/interpretation
These results suggest a possibility that NF-κB is involved in the formation of ERMs after PDR, especially for the development of vascular endothelial cell component.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Epiretinal membranes (ERMs) involving the macular or perimacular regions can cause a reduction in vision, metamorphopsia, micropsia, or occasionally monocular diplopia. The presence of ERMs has been associated with various clinical conditions including proliferative diabetic retinopathy (PDR), proliferative vitreoretinopathy (PVR), vitreous haemorrhage, congenital disorders, and idiopathic or spontaneous developments [1]. The prevalence of ERMs in PDR is reported to be about 20% in Type 1 diabetes and about 5% in Type 2 diabetes [2, 3]. Histopathological studies have shown that ERMs are composed of various cell types such as glial cells, fibroblasts and endothelial cells [4, 5, 6, 7], but their pathogenic mechanisms are still unknown. In contrast, trophic factors and cytokines, such as basic fibroblast growth factor (bFGF), vascular endothelial cell growth factor (VEGF) and interleukin-8 (IL-8) were detected in vitreous fluid and ERM samples derived from PDR patients [8, 9, 10, 11, 12]. In a previous study, we examined the expression of various trophic factor receptor genes in ERMs, and showed the possibility that glial cell line-derived neurotrophic factor (GDNF) is involved in the formation of glial cell component of ERMs after PDR [13]. However, we have not determined the possible molecular mechanisms in the formation of other cell types in PDR membranes.
Nuclear factor kappa B (NF-κB) is a transcription factor that can be activated by hypoxia, bacteria, viral proteins and proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-1β [14, 15]. NF-κB represents a group of structually related and evolutionarily conserved proteins, with five members in mammals: Rel (c-Rel), RelA (p65), RelB, NF-κB1 (p50 and its precursor p105), and NF-κB2 (p52 and its precursor p100) [16]. NF-κB/Rel proteins can exist as homo- or heterodimers. Among them, a heterodimeric complex of p65 and p50 subunits is thought to be central to the regulation of numerous inflammatory and proliferative response genes [17]. Therefore, we decided to investigate NF-κB p50 subunit using reverse transcription-polymerase chain reaction (RT-PCR) and immunohistochemical analysis. In resting cells, most NF-κB/Rel dimers are bound to IκB inhibitory proteins, but exposure to the above-mentioned stimuli generates a signal transduction cascade that leads to degradation of IκB. NF-κB released from IκB can then translocate to the nucleus and induce the transcription of genes that bear NF-κB-binding sites. The basis for the cytoplasmic localization of the inactive NF-κB/IκB complex is thought to be due to masking of the nuclear localizing signals (NLS) on the NF-κB subunits by the IκB proteins. Thus, IκB degradation leads to unmasking of the NLS, allowing free NF-κB dimers to enter the nuclear import pathway. The precise role of NF-κB in ocular diseases is not well understood. However, recent studies have shown that NF-κB regulates the expression of angiogenic factors such as IL-8 in the endothelial cells and induces neovascularization that could lead to proliferative vitreoretinal disorders such as PDR [18, 19, 20]. In addition, since endothelial cell is one of the main components of ERMs [4, 5, 6, 7], these findings suggest the possibility that NF-κB signalling is involved in the formation of PDR membranes.
In this study, we examined the expression of NF-κB p50 mRNAs in ERMs obtained from PDR and control patients, and found their high expression levels in PDR subjects. Interestingly, vascular endothelial cell component in PDR membranes were stained with NF-κB antibody raised against human p50 NLS region. Furthermore, NF-κB and IL-8 proteins were partially overlapped. We also proposed a possible relationship between NF-κB expression and ERM formation.
Subjects and methods
Subjects
This study was carried out in accordance with the tenets of the Helsinki Declaration. Informed consent was obtained from each patient for the collection of samples. Criteria for inclusion in the study were age less than 80 years old, absence of renal or haematological diseases or uremia, absent administration of chemotherapy or life-support measures, and the fewest possible chronic pathologies other than diabetes. The epiretinal membranes were surgically removed from consecutive eyes with secondary ERM following PDR (27 eyes) or idiopathic ERM (controls, 22 eyes) undergoing pars plana vitrectomy and membrane peeling in Toho University Sakura Hospital. Membranes were dissected from the retinal surface with horizontal scissors or membrane pick. Samples derived from 22 of the PDR patients (age 56±11 years, duration of diabetes 18±10 years) and 15 control subjects (age 68±7 years) were processed for reverse transcription-polymerase chain reaction (RT-PCR) analysis. The remainder of the PDR samples (age 51±16 years, duration of diabetes 15±6 years) and control samples (age 62±8 years) were processed for immunohistochemistry. These samples were embedded in optimum cutting temperature (OCT) compound (Miles Laboratories, Naperile, Ill., USA), flash-frozen in liquid nitrogen, and then stored at −80°C.
RNA extraction and amplification by RT-PCR
Total cellular RNA was prepared as previously reported [13]. 0.1 µg of RNA extracted from each sample was reverse transcribed into first-strand cDNA using the Superscript Preamplification System (Gibco, Paisley, Scotland) and oligo-dT primers.
RT-PCR analysis was carried out as previously described [13, 21]. Complementary DNA reverse transcribed from total RNA was amplified by using primers specific for human NF-κB p50 (sense: 5′-CAC TTA TGG ACA ACT ATG AGG TCT CTG G-3′; antisense: 5′-CTG TCT TGT GGA CAA CGC AGT GGA ATT TTA GG-3′) and glyceraldehyde-3-phosphate dehydrogenase (G3PDH) (sense: 5′-ACC ACA GTC CAT GCC ATC AC-3′; antisense: 5′-TCC ACC ACC CTG TTG CTG TA-3′). PCR was done after initial denaturation at 94°C for 3 min. Each cycle consisted of a heat-denaturation step at 94°C for 15 seconds, annealing of primers at 61°C for 2 min, followed by polymerization at 72°C for 2 min. The expected sizes of the amplified cDNA fragments of NF-κB and G3PDH were 406 and 452 bp, respectively. Human cDNA acquired from testis (Takara, Kyoto, Japan) was used as a positive control. Negative controls for PCR were done using "templates" derived from reverse transcription reactions lacking either reverse transcriptase or total RNA. After 35 cycles, 15 µl of each reaction mixture were electrophoresed on a 2% Tris borate-EDTA agarose gel and stained with ethidium bromide.
Immunohistochemistry
Frozen sections (7-µm thick) were cut by a cryostat, mounted on 3-aminopropyltriethoxysilane-coated glass slides, and air-dried at room temperature. For immunohistochemical analysis, the sections were fixed in ice cold acetone and then washed with phosphate buffered saline (PBS). The sections were incubated with normal donkey serum for 30 min to block non-specific staining. They were stained overnight at 4°C with an affinity-purified rabbit polyclonal antibody raised against amino acids 350 to 363 mapping within the nuclear location signal (NLS) region of human NF-κB p50 [22] (Santa Cruz Biotechnology, Santa Cruz, Calif., USA; 2.0 µg/ml). For double-labelling immunofluorescence studies, they were then incubated with a goat polyclonal antibody against IL-8 (Santa Cruz Biotechnology; 1.0 µg/ml) or von Willebrand factor (vWF) (Santa Cruz Biotechnology; 1.0 µg/ml) [23, 24, 25]. NF-κB was visualized with Cy3-conjugated donkey anti-rabbit IgG (Amersham Pharmacia Biotech, Piscataway, N.J., USA; 1000×), and IL-8 or vWF was visualized with FITC-conjugated donkey anti-goat IgG (Jackson Immunoresearch, West Groove, Pa, USA; 200×). The sections were examined by a confocal laser scanning microscope (Olympus, Tokyo, Japan). Primary antibody preabsorbed by blocking peptide (Santa Cruz Biotechnology) was used for negative controls. The adjacent section of each specimen was stained with haematoxylin and eosin.
Assessment of NF-κB-positive cell rate
NF-κB-positive cells were counted by a single observer who had no prior knowledge of the specimen information. Using a comparison with the adjacent section stained with haematoxylin and eosin, activated NF-κB-positive cells were counted in an immunohistochemistry profile. Measurements were performed with a calibrated reticle at 20X magnification as previously reported [26]. Since virtually all activated NF-κB is localized in the nucleus, cells were considered positive if any nuclear staining was present. The NF-κB-positive cell rate was defined as the percentage of activated NF-κB-positive cells relative to the total number of counted cells. In order to reduce sampling error, 60 to 100 cells were analyzed in each section.
Statistics
Data are shown as means ± SEM except as noted. The χ2 test was used to test for significance of the difference between presence of NF-κB mRNAs in PDR versus controls. For comparison of NF-κB-positive cell rate between PDR and controls, the Mann-Whitney's U test was used. A p of less than 0.05 was considered statistically significant.
Results
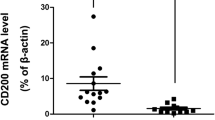
NF-κB p50 mRNA expression in ERMs was examined by RT-PCR analysis. NF-κB mRNA was detected in 20 of 22 (91%) PDR patients, but in only 9 of 15 (60%) idiopathic ERM (control) patients (p<0.05) (Table 1). Immunohistochemical analysis was carried out to identify the activated form of NF-κB p50 protein in ERMs after PDR. NF-κB protein was detected in all the five PDR subjects examined (Figs. 1A, 2A) and the immunoreactivity was completely abolished when primary antibody was preabsorbed with blocking peptide (data not shown). NF-κB protein was detected in five of the seven control subjects (data not shown), but its expression level was low. Quantitative analysis (Table 2) showed that the percentage of NF-κB-positive cells was 42±9% in PDR subjects, but only 10±3% in control subjects (p<0.01).
Expression of NF-κB (A) and von Willebrand factor (vWF) (B) in the ERM derived from a PDR patient age 49 years with an 8-year history of diabetes. (C) Double-labelling method shows the co-expression of NF-κB and vWF (arrow heads). (D) Haematoxylin and eosin staining of the adjacent section. Bar represents 100 µm
We next examined whether NF-κB protein is expressed in the neovascular region in PDR subjects. To assess this possibility, we used a vascular endothelial cell-specific marker, von Willebrand factor (vWF). ERMs contained many vWF-positive cells (Fig. 1B) and some of them were double-labelled with NF-κB (Fig. 1C). Since NF-κB could induce angiogenesis by regulating angiogenic factors such as IL-8, we also examined IL-8 protein expression. ERMs contained IL-8-positive cells (Fig. 2B) and some cells were double-labelled with NF-κB (Fig. 2C). Such IL-8 immunoreactivity was completely abolished when primary antibody was pre-absorbed with blocking peptide for IL-8 (data not shown).
Discussion
This study shows high expression levels of NF-κB mRNA in ERMs after PDR. In addition, we showed that NF-κB protein is partially overlapped with vascular endothelial cell-specific marker, vWF. Since NF-κB could regulate the expression of angiogenic factors [18, 19, 20], we also examined IL-8 protein expression in PDR subjects. Interestingly, in some cells, IL-8 was co-expressed with NF-κB. Together with previous findings that endothelial cell is one of the main components of ERMs [4, 5, 6, 7], NF-κB might be involved in the formation and development of neovascular component in PDR membranes.
One important issue is that NF-κB mRNA expression was detected in both primary and secondary ERMs (Table 1) although the number of NF-κB-positive cells was smaller in idiopathic (nonvascular) ERMs (Table 2). Previous studies have shown that IL-8 induced by NF-κB plays a key role in retinal angiogenesis after PDR [18, 19, 20]. In this context, it seems to be reasonable that NF-κB-positive cell number was larger in PDR (vascular) membranes. However, some NF-κB-positive cells were IL-8- or vWF-negative (Fig. 1 and Fig. 2). NF-κB is activated in glial cells, vascular endothelial cells, and macrophage/microglia, all of which are involved in neovascularization in diabetic retinopathy [19, 20]. Thus, NF-κB could be involved in the proliferation of various cell types other than vascular endothelial cells. In fact, we have determined that PDR membranes contain a large area composed of glial cells [13]. In any case, a more detailed role of NF-κB in the process of ERM formation should be determined. Another issue is that we collected ERM samples from patients whose disease had already manifested for several years. So, we cannot exclude the possibility that NF-κB activation in ERMs might be a secondary event. We will compare NF-κB expressions between newly-formed and relatively old ERM samples in future experiments.
In a previous study, we found high expression levels of GDNF receptor (GFRα2) in glial cell component and suggested the possibility that inhibiting the activity of this receptor could prevent the development of PDR membranes [13]. Since glial cells produce and store growth factors which activate endothelial cells [29, 30, 31, 32, 33, 34], this method might also inhibit the formation of neovascular component in ERMs. In contrast, the first step of the ERM formation is thought to be the neovascularization following the interaction of retinal vessels with the vitreous. In this process many angiogenic factors play an important role [9, 35, 36, 37]. Thus, blocking these angiogenic factors could inhibit ERM formation. In this context, IL-8 is one of the potential therapeutic targets. Recent studies have shown that transfection of IκB mutant, which blocks NF-κB activation [38], can inhibit angiogenesis by suppressing the production of IL-8 [39, 40]. These results suggest the possibility that inhibiting biological activity of NF-κB by specific blocker or antisence oligonucleotide could be useful in preventing the formation of PDR membranes, especially in avoiding membrane recurrence. However, before determining this possibility, further investigations about the precise role of NF-κB on retinal cells and all cell types in PDR membranes will be needed.
Abbreviations
- bFGF:
-
basic fibroblast growth factor
- ERM:
-
epiretinal membrane
- GDNF:
-
glial cell line-derived neurotrophic factor
- IL-8:
-
interleukin-8
- NF-κB:
-
nuclear factor kappa B
- PDR:
-
proliferative diabetic retinopathy
- PVR:
-
proliferative vitreoretinopathy
- TGF-α:
-
transforming growth factor-α
- VEGF:
-
vascular endothelial cell growth factor
- vWF:
-
von Willebrand factor
References
Margherio RR, Margherio AR (2000) Epiretinal macular membranes. In: Albert DM, Jakobiec FA, Azar DT, Gragoudas ES (eds) Principles and practice of ophthalmology, 2nd edn. W.B. Saunders, Philadelphia, p 2103
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 102:520–526
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol 102:527–532
Roth AM, Foos RY (1971) Surface wrinkling retinopathy in eyes enucleated at autopsy. Trans Am Acad Ophthalmol Otolaryngol 75:1047–1058
Bellhorn MB, Friedman AH, Wise GN, Henkind P (1975) Ultrastructure and clinicopathologic correlation of idiopathic preretinal macular fibrosis. Am J Ophthalmol 79:366–373
McLeod D, Hiscott PS, Grierson I (1987) Age-related cellular proliferation at the vitreoretinal juncture. Eye 1:263–281
Smiddy WE, Maguire AM, Green WR et al. (1989) Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology 96:811–821
Sivalingam A, Kenney J, Brown GC, Benson WE, Donoso L (1990) Basic fibroblast growth factor levels in the vitreous of patients with proliferative diabetic retinopathy. Arch Ophthalmol 108:869–872
Wiedemann P (1992) Growth factors in retinal diseases: proliferative vitreoretinopathy, proliferative diabetic retinopathy, and retinal degeneration. Surv Ophthalmol 36:373–384
Aiello LP, Avery RL, Arrigg PG et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Elner SG, Elner VM, Jaffe GJ, Stuart A, Kunkel SL, Strieter RM (1995) Cytokines in proliferative diabetic retinopathy and proliferative vitreoretinopathy. Curr Eye Res 14:1045–1053
Hueber A, Wiedemann P, Esser P, Heimann K (1996) Basic fibroblast growth factor mRNA, bFGF peptide and FGF receptor in epiretinal membranes of intraocular proliferative disorders (PVR and PDR). Int Ophthalmol 20:345–350
Harada T, Harada C, Mitamura Y et al. (2002) Neurotrophic factor receptors in epiretinal membranes after human diabetic retinopathy. Diabetes Care 25:1060–1065
Baeuerle PA, Henkel T (1994) Function and activation of NF-κB in the immune system. Annu Rev Immunol 12:141–179
Wang X, Jobin C, Allen JB, Roberts WL, Jaffe GJ (1999) Suppression of NF-κB-dependent proinflammatory gene expression in human RPE cells by a proteasome inhibitor. Invest Ophthalmol Vis Sci 40:477–486
Ghosh S, Karin M (2002) Missing pieces in the NF-κB puzzle. Cell 109 Suppl:S81–96
Grilli M, Chiu JJ, Lenardo MJ (1993) NF-κB and Rel: participants in a multiform transcriptional regulatory system. Int Rev Cytol 143:1–62
Stoltz RA, Abraham NG, Laniado-Schwartzman M (1996) The role of NF-κB in the angiogenic response of coronary microvessel endothelial cells. Proc Natl Acad Sci USA 93:2832–2837
Yoshida A, Yoshida S, Hata Y, Khalil AK, Ishibashi T, Inomata H (1998) The role of NF-κB in retinal neovascularization in the rat. Possible involvement of cytokine-induced neutrophil chemoattractant (CINC), a member of the interleukin-8 family. J Histochem Cytochem 46:429–436
Yoshida A, Yoshida S, Khalil AK, Ishibashi T, Inomata H (1998) Role of NF-κB-mediated interleukin-8 expression in intraocular neovascularization. Invest Ophthalmol Vis Sci 39:1097–1106
Harada T, Harada C, Sekiguchi M, Wada K (1998) Light-induced retinal degeneration suppresses developmental progression of flip-to-flop alternative splicing in GluR1. J Neurosci 18:3336–3343
Hammes HP, Hoerauf H, Alt A et al. (1999) N(epsilon)(carboxymethyl)lysin and the AGE receptor RAGE colocalize in age-related macular degeneration. Invest Ophthalmol Vis Sci 40:1855–1859
Wagner DD (1990) Cell biology of von Willebrand factor. Annu Rev Cell Biol 6:217–246
Asiyo-Vogel MN, El-Hifnawi ES, Bopp S, Laqua H (1998) The vascular component of proliferative vitreoretinopathy membranes: an immunohistochemical and ultrastructural study. Retina 18:56–61
Igarashi Y, Chiba H, Utsumi H et al. (2000) Expression of receptors for glial cell line-derived neurotrophic factor (GDNF) and neurturin in the inner blood-retinal barrier of rats. Cell Struct Funct 25:237–241
Harada T, Harada C, Watanabe M et al. (1998) Functions of the two glutamate transporters GLAST and GLT-1 in the retina. Proc Natl Acad Sci USA 95:4663–4666
Kelley J, Yerra L, Smith JK, Chi DS (1999) Human endothelium as a source of multifunctional cytokines: molecular regulation and possible role in human disease. J Interferon Cytokine Res 19:91–104
Roebuck KA (1999) Oxidant stress regulation of IL-8 and ICAM-1 gene expression: differential activation and binding of the transcription factors AP-1 and NF-kappaB (Review). Int J Mol Med 4:223–230
Ohira A, Juan E de Jr (1990) Characterization of glial involvement in proliferative diabetic retinopathy. Ophthalmologica 201:187–195
Laterra J, Goldstein GW (1991) Astroglial-induced in vitro angiogenesis: requirements for RNA and protein synthesis. J Neurochem 57:1231–1239
Amin RH, Frank RN, Kennedy A, Eliott D, Puklin JE, Abrams GW (1997) Vascular endothelial growth factor is present in glial cells of the retina and optic nerve of human subjects with nonproliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 38:36–47
Behzadian MA, Wang XL, Shabrawey M, Caldwell RB (1998) Effects of hypoxia on glial cell expression of angiogenesis-regulating factors VEGF and TGF-beta. Glia 24:216–225
Harada T, Harada C, Nakayama N et al. (2000) Modification of glial-neuronal cell interactions prevents photoreceptor apoptosis during light-induced retinal degeneration. Neuron 26:533–541
Harada T, Harada C, Kohsaka S et al. (2002) Microglia-Müller glia cell interactions control neurotrophic factor production during light-induced retinal degeneration. J Neurosci 22:9228–9236
BenEzra D (1978) Neovasculogenic ability of prostaglandins, growth factors, and synthetic chemoattractants. Am J Ophthalmol 86:455–461
Masferrer JL, Murphy RC, Pagano PJ, Dunn MW, Laniado-Schwartzman M (1989) Ocular effects of a novel cytochrome P-450-dependent arachidonic acid metabolite. Invest Ophthalmol Vis Sci 30:454–460
Heldin CH, Usuki K, Miyazono K (1991) Platelet-derived endothelial cell growth factor. J Cell Biochem 47:208–210
Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM (1996) Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science 274:787–789
Huang S, Robinson JB, Deguzman A, Bucana CD, Fidler IJ (2000) Blockade of nuclear factor-kappaB signaling inhibits angiogenesis and tumorigenicity of human ovarian cancer cells by suppressing expression of vascular endothelial growth factor and interleukin 8. Cancer Res 60:5334–5339
Oitzinger W, Hofer-Warbinek R, Schmid JA, Koshelnick Y, Binder BR, Martin R de (2001) Adenovirus-mediated expression of a mutant IkappaB kinase 2 inhibits the response of endothelial cells to inflammatory stimuli. Blood 97:1611–1617
Acknowledgements
Supported by Ministry of Education, Culture, Sports, Science and Technology of Japan; Ministry of Health, Labour and Welfare of Japan; Japan Diabetes Foundation (T.H.), and Japan Foundation for Aging and Health (C.H.).
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00125-003-1201-x
Rights and permissions
About this article
Cite this article
Mitamura, Y., Harada, T., Harada, C. et al. NF-κB in epiretinal membranes after human diabetic retinopathy. Diabetologia 46, 699–703 (2003). https://doi.org/10.1007/s00125-003-1084-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-003-1084-x