Abstract
Background
Radiosurgical treatment of brain metastases is well established in daily clinical routine. Utilization of flattening-filter-free beams (FFF) may allow for more rapid delivery of treatment doses and improve clinical comfort. Hence, we compared plan quality and efficiency of radiosurgery in FFF mode to FF techniques.
Materials and methods
Between November 2014 and June 2015, 21 consecutive patients with 25 brain metastases were treated with stereotactic radiosurgery (SRS) in FFF mode. Brain metastases received dose-fractionation schedules of 1 × 20 Gy or 1 × 18 Gy, delivered to the conformally enclosing 80 % isodose. Three patients with critically localized or large (>3 cm) brain metastases were treated with 6 × 5 Gy. Plan quality and efficiency were evaluated by analyzing conformity, dose gradients, dose to healthy brain tissue, treatment delivery time, and number of monitor units. FFF plans were compared to those using the FF method, and early clinical outcome and toxicity were assessed.
Results
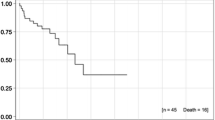
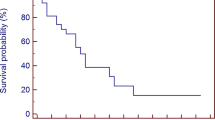
FFF mode resulted in significant reductions in beam-on time (p < 0.001) and mean brain dose (p = 0.001) relative to FF-mode comparison plans. Furthermore, significant improvements in dose gradients and sharper dose falloffs were found for SRS in FFF mode (−1.1 %, −29.6 %; p ≤ 0.003), but conformity was slightly superior in SRS in FF mode (−1.3 %; p = 0.001). With a median follow-up time of 5.1 months, 6‑month overall survival was 63.3 %. Local control was observed in 24 of 25 brain metastases (96 %).
Conclusion
SRS in FFF mode is time efficient and provides similar plan quality with the opportunity of slightly reduced dose exposure to healthy brain tissue when compared to SRS in FF mode. Clinical outcomes appear promising and show only modest treatment-related toxicity.
Zusammenfassung
Hintergrund
Die radiochirurgische Behandlung (SRS) von Hirnmetastasen wird vielfach in der klinischen Routine durchgeführt. Die zusätzliche Anwendung von ausgleichsfilterfreien Bestrahlungstechniken (FFF) kann die Bestrahlungszeit verkürzen und den Patientenkomfort erhöhen. Daher führten wir einen Plan- und Effizienzvergleich zwischen der Radiochirurgie in FFF-Technik und FF-Technik durch.
Material und Methode
Zwischen November 2014 und Juni 2015 wurden 21 Patienten mit 25 Hirnmetastasen mit SRS in FFF-Technik behandelt. Die Hirnmetastasen wurden mit 1 × 20 Gy oder 1 × 18 Gy auf die konformal umschließende 80 %-Isodose bestrahlt. Drei Patienten mit kritisch lokalisierten oder großen Metastasen (>3 cm) erhielten eine Bestrahlung mit 6 × 5 Gy. Konformität, Dosisgradienten, Behandlungszeiten, Normalgewebsdosis (Gehirn) sowie Anzahl an Monitoreinheiten wurden zur Evaluation der Planqualität herangezogen. Des Weiteren wurden Überleben und Toxizität analysiert.
Ergebnisse
Sowohl die Bestrahlungszeit sank signifikant um 57,9 % (p ≤ 0,001) für die SRS in FFF-Technik im Vergleich zur FF-Technik. als auch die durchschnittliche Bestrahlungsdosis des Gehirns (p = 0,001). Des Weiteren wurden signifikant verbesserte Dosisgradienten und folglich ein steilerer Dosisabfall für die SRS in FFF-Technik (−1,1 %, −29,6 %; p ≤ 0,003) festgestellt. Dagegen zeigte die SRS in FF-Technik einen leicht verbesserten Konformitätsindex (−1,3 %; p = 0,001). Bei einer medianen Nachbeobachtungzeit von 5,1 Monaten betrug das 6‑Monats-Gesamtüberleben 63,3 %. Bei den behandelten 25 Hirnmetastasen (96 %) waren 24 ohne lokalen Progress.
Schlussfolgerung
SRS in FFF-Technik ist zeiteffizient und ermöglicht gleiche Planqualität sowie eine leicht reduzierte Dosisbelastung des gesunden Hirngewebes im Vergleich zur SRS in FF-Technik. Entsprechend vielversprechend sind die ersten klinischen Ergebnisse bei moderater Toxizität.


Similar content being viewed by others
References
Leksell DG (1987) Stereotactic radiosurgery. Present status and future trends. Neurol Res 9(2):60–68
Lutz W, Winston KR, Maleki N (1988) A system for stereotactic radiosurgery with a linear accelerator. Int J Radiat Oncol Biol Phys 14(2):373–381
Sturm V, Kober B, Hover KH et al (1987) Stereotactic percutaneous single dose irradiation of brain metastases with a linear accelerator. Int J Radiat Oncol Biol Phys 13(2):279–282
Rades D, Hornung D, Blanck O et al (2014) Stereotactic radiosurgery for newly diagnosed brain metastases: comparison of three dose levels. Strahlenther Onkol 190(9):786–791. doi:10.1007/s00066-014-0625-1
Treuer H, Hoevels M, Luyken K et al (2014) Intracranial stereotactic radiosurgery with an adapted linear accelerator vs. robotic radiosurgery. Strahlenther Onkol 191(6):470–476. doi:10.1007/s00066-014-0786-y
Kocher M, Wittig A, Piroth MD et al (2014) Stereotactic radiosurgery for treatment of brain metastases. A report of the DEGRO Working Group on Stereotactic Radiotherapy. Strahlenther Onkol 190(6):521–532. doi:10.1007/s00066-014-0648-7
Lin X, DeAngelis LM (2015) Treatment of brain metastases. J Clin Oncol 33(30):3475–3484. doi:10.1200/jco.2015.60.9503
Soffietti R, Kocher M, Abacioglu UM et al (2013) A European Organisation for Research and Treatment of Cancer phase III trial of Adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life result. J Clin Oncol 31(1):65–72. doi:10.1200/jco.2011.41.0639
Nieder C, Grosu AL, Gaspar LE (2014) Stereotactic radiosurgery (SRS) for brain metastases: a systematic review. Radiat Oncol 9:155. doi:10.1186/1748-717X-9-155
Hartmann GH, Schlegel W, Sturm V et al (1985) Cerebral radiation surgery using moving field irradiation at a linear accelerator facility. Int J Radiat Oncol Biol Phys 11(6):1185–1192
Kragl G, af Wetterstedt S, Knäusl B et al (2009) Dosimetric characteristics of 6 and 10 MV unflattened photon beams. Radiother Oncol 93(1):141–146. doi:10.1016/j.radonc.2009.06.008
Cashmore J (2008) The characterization of unflattened photon beams from a 6 MV linear accelerator. Phys Med Biol 53(7):1933–1946. doi:10.1088/0031-9155/53/7/009
Vassiliev ON, Titt U, Ponisch F et al (2006) Dosimetric properties of photon beams from a flattening filter free clinical accelerator. Phys Med Biol 51(7):1907–1917. doi:10.1088/0031-9155/51/7/019
Sperduto PW, Kased N, Roberge D et al (2012) Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30(4):419–425. doi:10.1200/JCO.2011.38.0527
Audet C, Poffenbarger BA, Chang P et al (2011) Evaluation of volumetric modulated arc therapy for cranial radiosurgery using multiple noncoplanar arcs. Med Phys 38(11):5863–5872. doi:10.1118/1.3641874
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. J Neurosurg 93(supplement 3):219–222. doi:10.3171/jns.2000.93.supplement 3.0219
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201. doi:10.3171/sup.2006.105.7.194
Stieler F, Fleckenstein J, Simeonova A et al (2013) Intensity modulated radiosurgery of brain metastases with flattening filter-free beams. Radiotherapy and oncology. J Eur Soc Ther Radiol Oncol 109(3):448–451. doi:10.1016/j.radonc.2013.10.017
Sahgal A, Aoyama H, Kocher M et al (2015) Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol 91(4):710–717. doi:10.1016/j.ijrobp.2014.10.024
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29(2):134–141. doi:10.1200/JCO.2010.30.1655
Bhatnagar AK, Flickinger JC, Kondziolka D et al (2006) Stereotactic radiosurgery for four or more intracranial metastases. Int J Radiat Oncol 64(3):898–903. doi:10.1016/j.ijrobp.2005.08.035
Yamamoto M, Serizawa T, Shuto T et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395. doi:10.1016/S1470-2045(14)70061-0
Lang S, Shrestha B, Graydon S et al (2013) Clinical application of flattening filter free beams for extracranial stereotactic radiotherapy. Radiother Oncol 106(2):255–259. doi:10.1016/j.radonc.2012.12.012
Kragl G, Baier F, Lutz S et al (2011) Flattening filter free beams in SBRT and IMRT: Dosimetric assessment of peripheral doses. Z Med Phys 21(2):91–101. doi:10.1016/j.zemedi.2010.07.003
Reggiori G, Mancosu P, Castiglioni S et al (2012) Can volumetric modulated arc therapy with flattening filter free beams play a role in stereotactic body radiotherapy for liver lesions? A volume-based analysis. Med Phys 39(2):1112–1118. doi:10.1118/1.3679858
Navarria P, Ascolese AM, Mancosu P et al (2013) Volumetric modulated arc therapy with flattening filter free (FFF) beams for stereotactic body radiation therapy (SBRT) in patients with medically inoperable early stage non small cell lung cancer (NSCLC). Radiotherapy and oncology. J Eur Soc Ther Radiol Oncol 107(3):414–418. doi:10.1016/j.radonc.2013.04.016
Nicolini G, Ghosh-Laskar S, Shrivastava SK et al (2012) Volumetric modulation arc radiotherapy with flattening filter-free beams compared with static gantry IMRT and 3D Conformal radiotherapy for advanced esophageal cancer: A feasibility study. Int J Radiat Oncol 84(2):553–560. doi:10.1016/j.ijrobp.2011.12.041
Zwahlen DR, Lang S, Hrbacek J et al (2012) The use of photon beams of a flattening filter-free linear accelerator for Hypofractionated volumetric modulated arc therapy in localized prostate cancer. Int J Radiat Oncol 83(5):1655–1660. doi:10.1016/j.ijrobp.2011.10.019
Lu JY, Zheng J, Zhang WZ et al (2016) Flattening filter-free beams in intensity-modulated radiotherapy and volumetric modulated arc therapy for Sinonasal cancer. PLoS ONE 11(1):e0146604. doi:10.1371/journal.pone.0146604
Spruijt KH, Dahele M, Cuijpers JP et al (2013) Flattening filter free vs flattened beams for breast irradiation. Int J Radiat Oncol 85(2):506–513. doi:10.1016/j.ijrobp.2012.03.040
Gasic D, Ohlhues L, Brodin NP et al (2014) A treatment planning and delivery comparison of volumetric modulated arc therapy with or without flattening filter for gliomas, brain metastases, prostate, head/neck and early stage lung cancer. Acta Oncol 53(8):1005–1011. doi:10.3109/0284186X.2014.925578
Lechner W, Kragl G, Georg D (2013) Evaluation of treatment plan quality of IMRT and VMAT with and without flattening filter using Pareto optimal fronts. Radiother Oncol 109(3):437–441. doi:10.1016/j.radonc.2013.09.020
Kaul D, Badakhshi H, Gevaert T et al (2015) Dosimetric comparison of different treatment modalities for stereotactic radiosurgery of meningioma. Acta Neurochir (Wien) 157(4):559–563 (discussion 563–554) doi:10.1007/s00701-014-2272-9
Treuer H, Hoevels M, Luyken K et al (2014) Intracranial stereotactic radiosurgery with an adapted linear accelerator vs. robotic radiosurgery : Comparison of dosimetric treatment plan quality. Strahlenther Onkol. doi:10.1007/s00066-014-0786-y
Kim H, Potrebko P, Rivera A et al (2015) Tumor volume threshold for achieving improved conformity in VMAT and Gamma Knife stereotactic radiosurgery for vestibular schwannoma. Radiother Oncol 115(2):229–234. doi:10.1016/j.radonc.2015.03.031
Mayo CS, Ding L, Addesa A et al (2010) Initial experience with volumetric IMRT (RapidArc) for intracranial stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 78(5):1457–1466. doi:10.1016/j.ijrobp.2009.10.005
Alongi F, Cozzi L, Arcangeli S et al (2013) Linac based SBRT for prostate cancer in 5 fractions with VMAT and flattening filter free beams: preliminary report of a phase II study. Radiat Oncol 8(1):1–8. doi:10.1186/1748-717x-8-171
Alongi F, Fogliata A, Clerici E et al (2012) Volumetric modulated arc therapy with flattening filter free beams for isolated abdominal/pelvic lymph nodes: report of dosimetric and early clinical results in oligometastatic patients. Radiat Oncol 7(1):1–9. doi:10.1186/1748-717x-7-204
Scorsetti M, Alongi F, Castiglioni S et al (2011) Feasibility and early clinical assessment of flattening filter free (FFF) based stereotactic body radiotherapy (SBRT) treatments. Radiat Oncol 6:113. doi:10.1186/1748-717X-6-113
Stieb S, Lang S, Linsenmeier C et al (2015) Safety of high-dose-rate stereotactic body radiotherapy. Radiat Oncol 10(1):27. doi:10.1186/s13014-014-0317-0
Prendergast BM, Dobelbower MC, Bonner JA et al (2013) Stereotactic body radiation therapy (SBRT) for lung malignancies: preliminary toxicity results using a flattening filter-free linear accelerator operating at 2400 monitor units per minute. Radiat Oncol 8:273. doi:10.1186/1748-717X-8-273
Wang P‑M, Hsu W‑C, Chung N‑N et al (2014) Feasibility of stereotactic body radiation therapy with volumetric modulated arc therapy and high intensity photon beams for hepatocellular carcinoma patients. Radiat Oncol 9(1):1–9. doi:10.1186/1748-717x-9-18
Acknowledgements
This work was supported by the Medical Faculty providing a research grant for JR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Rieber, E. Tonndorf-Martini, O. Schramm, B. Rhein, S. Stefanowicz, J. Kappes, H. Hoffmann, K. Lindel, J. Debus and S. Rieken declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Ethical approval was obtained from the local Ethics Committee (S-140/2016).
Rights and permissions
About this article
Cite this article
Rieber, J., Tonndorf-Martini, E., Schramm, O. et al. Radiosurgery with flattening-filter-free techniques in the treatment of brain metastases. Strahlenther Onkol 192, 789–796 (2016). https://doi.org/10.1007/s00066-016-1012-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1012-x