Abstract
Background and purpose
Three doses were compared for local control of irradiated metastases, freedom from new brain metastases, and survival in patients receiving stereotactic radiosurgery (SRS) alone for one to three newly diagnosed brain metastases.
Patients and methods
In all, 134 patients were assigned to three groups according to the SRS dose given to the margins of the lesions: 13–16 Gy (n = 33), 18 Gy (n = 18), and 20 Gy (n = 83). Additional potential prognostic factors were evaluated: age (≤ 60 vs. > 60 years), gender, Karnofsky Performance Scale score (70–80 vs. 90–100), tumor type (non-small-cell lung cancer vs. melanoma vs. others), number of brain metastases (1 vs. 2–3), lesion size (< 15 vs. ≥ 15 mm), extracranial metastases (no vs. yes), RPA class (1 vs. 2), and interval of cancer diagnosis to SRS (≤ 24 vs. > 24 months).
Results
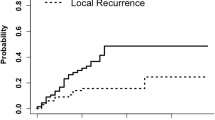
For 13–16 Gy, 18 Gy, and 20 Gy, the 1-year local control rates were 31, 65, and 79 %, respectively (p < 0.001). The SRS dose maintained significance on multivariate analysis (risk ratio: 2.25; 95 % confidence interval: 1.56–3.29; p < 0.001). On intergroup comparisons of local control, 20 Gy was superior to 13–16 Gy (p < 0.001) but not to 18 Gy (p = 0.12); 18 Gy showed a strong trend toward better local control when compared with 13–16 Gy (p = 0.059). Freedom from new brain metastases (p = 0.57) and survival (p = 0.15) were not associated with SRS dose in the univariate analysis.
Conclusion
SRS doses of 18 Gy and 20 Gy resulted in better local control than 13–16 Gy. However, 20 Gy and 18 Gy must be compared again in a larger cohort of patients. Freedom from new brain metastases and survival were not associated with SRS dose.
Zusammenfassung
Hintergrund und Ziel
Drei Dosislevel bei der alleinigen stereotaktischen Radiochirurgie (SRS) von 1 bis 3 neu diagnostizierten Hirnmetastasen wurden hinsichtlich lokaler Kontrolle der bestrahlten Metastasen, Nichtauftreten neuer Hirnmetastasen und Gesamtüberleben verglichen.
Material und Methoden
Nach der am Rand der Metastasen applizierten SRS-Dosis wurden 134 Patienten den Gruppen 13–16 Gy (n = 33), 18 Gy (n = 18) und 20 Gy (n = 83) zugeteilt. Weitere mögliche Prognosefaktoren wurden untersucht: Alter (≤ 60 vs. > 60 Jahre), Geschlecht, Karnofsky-Performance-Score (KPS 70–80 vs. 90–100), Primärtumor (nichtkleinzelliges Bronchialkarzinom vs. Melanom vs. andere), Anzahl der Hirnmetastasen (1 vs. 2–3), Größe der Läsionen (< 15 vs. ≥ 15 mm), extrakranielle Metastasen (nein vs. ja), RPA-Klasse (1 vs. 2) und Intervall von der Erstdiagnose der Tumorerkrankung bis zur SRS (≤ 24 vs. > 24 Monate).
Ergebnisse
In den 3 Gruppen 13–16 Gy, 18 Gy und 20 Gy betrugen die Raten für die lokale Kontrolle nach 1 Jahr 31 %, 65 % und 79 % (p < 0,001). Die SRS-Dosis war auch in der multivariaten Analyse signifikant (Risk-Ratio: 2,25; 95 % CI 1,56–3,29; p < 0,001). Nach den Vergleichen zwischen den Gruppen hinsichtlich der lokalen Kontrolle war 20 Gy signifikant 13–16 Gy überlegen (p < 0,001), nicht jedoch 18 Gy (p = 0,12). Der Vergleich 18 Gy vs. 13–16 Gy ergab einen deutlichen Trend zugunsten von 18 Gy (p = 0,059). Das Nichtauftreten neuer Hirnmetastasen (p = 0,57) und das Gesamtüberleben (p = 0,15) waren in der univariaten Analyse nicht mit der SRS-Dosis assoziiert.
Schlussfolgerung
SRS-Dosen von 20 Gy und 18 Gy waren mit einer besseren lokalen Kontrolle assoziiert als 13–16 Gy. 20 Gy und 18 Gy müssen erneut in einer größeren Patientenkohorte verglichen werden. Das Nichtauftreten neuer Hirnmetastasen und das Gesamtüberleben waren nicht mit der SRS-Dosis assoziiert.
Similar content being viewed by others
References
Abacioglu U, Caglar H, Atasoy BM et al (2010) Gamma knife radiosurgery in non small cell lung cancer patients with brain metastases: treatment results and prognostic factors. J Buon 15:274–280
Aoyama H, Shirato H, Tago M et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Dziggel L, Segedin B, Podvrsnik NH et al (2013) Validation of a survival score for patients treated with whole-brain radiotherapy for brain metastases. Strahlenther Onkol 189:364–366
Gaudy-Marqueste C, Regis JM, Muracciole X et al (2006) Gamma-Knife radiosurgery in the management of melanoma patients with brain metastases: a series of 106 patients without whole-brain radiotherapy. Int J Radiat Oncol Biol Phys 65:809–816
Golden DW, Lamborn KR, McDermott MW et al (2008) Prognostic factors and grading systems for overall survival in patients treated with radiosurgery for brain metastases: variation by primary site. J Neurosurg 109(Suppl):77–86
Kaplan EL, Meier P (1958) Non parametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29:134–141
Likhacheva A, Pinnix CC, Parikh NR et al (2013) Predictors of survival in contemporary practice after initial radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 85:656–661
Marcus DM, Lowe M, Khan MK et al (2013) Prognostic factors for overall survival after radiosurgery for brain metastases from melanoma. Am J Clin Oncol (in press)
Nieder C, Andratschke NH, Geinitz H et al (2012) Use of the Graded Prognostic Assessment (GPA) score in patients with brain metastases from primary tumours not represented in the diagnosis-specific GPA studies. Strahlenther Onkol 188:692–695
Rades D, Kueter JD, Hornung D et al (2008) Comparison of stereotactic radiosurgery (SRS) alone and whole brain radiotherapy (WBRT) plus a stereotactic boost (WBRT + SRS) for one to three brain metastases. Strahlenther Onkol 184:655–662
Rades D, Kueter JD, Gliemroth J et al (2012) Resection plus whole-brain irradiation versus resection plus whole-brain irradiation plus boost for the treatment of single brain metastasis. Strahlenther Onkol 188:143–147
Shehata MK, Young B, Reid B et al (2004) Stereotatic radiosurgery of 468 brain metastases ⤠2 cm: implications for SRS dose and whole brain radiation therapy. Int J Radiat Oncol Biol Phys 59:87–93
Skeie BS, Skeie GO, Enger PØ et al (2011) Gamma knife surgery in brain melanomas: absence of extracranial metastases and tumor volume strongest indicators of prolonged survival. World Neurosurg 75:684–691
Vogelbaum MA, Angelov L, Lee SY et al (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104:907–912
Wen PY, Black PM, Loeffler JS (2001) Metastatic brain cancer. In: deVita V, Hellman S, Rosenberg SA (eds) Cancer: principles and practice of oncology, 6th edn. Lippincott, Williams & Wilkins, Philadelphia, pp 2655–2670
Zindler JD, Rodrigues G, Haasbeek CJ et al (2013) The clinical utility of prognostic scoring systems in patients with brain metastases treated with radiosurgery. Radiother Oncol 106:370–374
Compliance with ethical guidelines
Conflict of interest
D. Rades, D. Hornung, O. Blanck, K. Martens, M. Trong Khoa, N. Thuy Trang, M. Hüppe, P. Terheyden, J. Gliemroth, and S. E. Schild state that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rades, D., Hornung, D., Blanck, O. et al. Stereotactic radiosurgery for newly diagnosed brain metastases. Strahlenther Onkol 190, 786–791 (2014). https://doi.org/10.1007/s00066-014-0625-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0625-1
Keywords
- Brain metastases
- Stereotactic radiosurgery dose
- Local control
- Freedom from new brain metastases
- Survival