Abstract
Objective
To present an updated and evidence-based guideline for the use of dual-energy x-ray absorptiometry (DXA) to assess body composition in clinical practice.
Materials and methods
This Official Position was developed by the Scientific Committee of the Brazilian Association of Bone Assessment and Metabolism (Associação Brasileira de Avaliação Óssea e Osteometabolismo, ABRASSO) and experts in the field who were invited to contribute to the preparation of this document. The authors searched current databases for relevant publications in the area of body composition assessment. In this second part of the Official Position, the authors discuss the interpretation and reporting of body composition parameters assessed by DXA and the use of DXA for body composition evaluation in special situations, including evaluation of children, persons with HIV, and animals.
Conclusion
This document offers recommendations for the use of DXA in body composition evaluation, including indications, interpretation, and applications, to serve as a guiding tool in clinical practice and research for health care professionals in Brazil.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
In clinical practice, body composition may be assessed by different methods such as air or water displacement, bioelectrical impedance (BIA), computed tomography (CT), magnetic resonance imaging (MRI), and dual-energy x-ray absorptiometry (DXA). Anthropometric measurements can also be used as a surrogate approach for estimating body composition. Each of these methods has strengths and limitations in terms of accessibility, accuracy, and comprehensiveness [1].
Systems of BIA measure the resistance to a harmless electric current flow passing through the body. The electricity conducted through the water in the body provides an estimate of the total body water and predicts an individual's fat-free mass (FFM) based on assumed constant hydration, as used in the deuterium dilution method. However, BIA is not a reference method to measure body composition since it relies on specific assumptions, of which the most important is constant hydration [2].
In contrast, MRI and CT offer more detailed measurements of specific tissues and small areas, e.g., fat infiltration and visceral adiposity. Critical limitations of both methods include radiation exposure related to CT scanning, and high cost and limited availability related to MRI scanning [1].
Ultrasound has inconsistent image reproducibility that may be caused by variations in the pressure applied by the transducer on the skin, measurement site, anisotropy, and protocol feasibility, limiting the diagnostic and monitoring application of ultrasound for assessment of nutritional status [3]. According to the current best evidence, only anthropometric measurements correlate with cardiovascular risk and metabolic syndrome [4].
Originally developed to measure bone mineral density (BMD) and bone mineral content (BMC), DXA is also used to measure lean and fat mass. DXA systems straddle the line between a three-compartment model and a two-compartment model (FFM = BMC + lean mass) of the body [2]. DXA is preferable for body composition assessment, as it performs whole-body scanning in a short time, emits low radiation, provides regional analyses, and is likely to be more accessible and affordable than CT or MRI. Compared with other methods, DXA has been recommended as the standard method for assessing body composition in most patient groups (Table 1) [1, 3, 5, 6].
Materials and methods
This document is a result of efforts by the Brazilian Association of Bone Assessment and Metabolism (Associação Brasileira de Avaliação Óssea e Osteometabolismo/Brazilian Society on Bone and Osteometabolism Evaluation, ABRASSO) for the development of recommendations based on the current evidence available in the scientific literature regarding measurement of body composition using DXA. The ABRASSO Scientific Committee invited experts in the field to contribute to the preparation of this document. The authors were invited by ABRASSO to provide scientific information on body composition measurements. ABRASSO was chosen as the official organization for the preparation of this document considering its national expression and the fact that it congregates professionals from several medical areas related to bone and mineral metabolism (rheumatology, endocrinology, gynecology, orthopedics, geriatric and gerontology, physiatry, sports medicine and rehabilitation, nephrology, infectious diseases, pediatrics, veterinary medicine) along with supporting health care professionals (nutritionists, dietitians, biomedical scientists, biologists, pharmacists, physical therapists, psychologists, and basic researchers). The main criteria for inviting collaborators were their areas of expertise, contributions to the field, association with medical organizations related to the topics covered in this document, and publication of papers and practical management on the covered topic, thus fulfilling the endorsement by ABRASSO and other participating medical societies. The invited authors were divided into small groups (with 2 to 6 authors per group) according to their areas of expertise and questions to be addressed. Additionally, all the authors composed the steering committee for the development of the study that resulted in the present document and designed the protocol to address specific questions related to the applicability of body composition measurements (including technical and practical issues). All the authors wrote the manuscript with input from each other, critically reviewed the manuscript, and approved its final version for submission (fulfilling the criteria for authorship). Only one of the authors had a conflict of interest to disclose related to the topic of body composition measurements (reported at the end of the paper), and all the authors participated actively in the discussions and are responsible for the information reported in this document.
The aim of this position statement is to answer routine questions about body composition assessment and serve as a guideline for clinicians and researchers in Brazil. The authors searched current databases for relevant publications and described their findings below using a narrative review format. The search strategy was similar among all authors and was conducted by each group using the electronic databases MEDLINE (via PubMed), Embase, and SciELO. The expressions used included “adult and pediatric normative data,” “lean mass measurements,” “fat mass measurements,” “basic area and technical science,” “other anthropometrical measurements,” “other non-DXA body composition measurements,” among others. The authors also searched for other potential studies not retrieved by the search strategies by consulting review articles, meta-analyses/systematic reviews, and guidelines issued by specialty societies, particularly the International Society for Clinical Densitometry (ISCD) Official Position. To increase the search sensitivity, MeSH search terms were used for clinical conditions and therapeutic interventions but not for comparators or outcomes. Only studies published in Portuguese, English, and Spanish were considered. The search was limited to studies published between January 1st, 2000, and July 31st, 2021. The search in each electronic database included the following descriptors (key words): “body composition measurements,” “DXA,” “other measurements NO DXA,” “skinfold,” “plethysmography,” “ultrasound,” “computed tomography,” “magnetic resonance imaging,” “bioelectrical impedance analysis,” “absorptiometry,” “x-ray,” “methodology,” “artifacts,” “technical procedures,” “fat mass,” “bone mass,” “lean mass,” “sarcopenia,” “DXA,” “clinical conditions,” “elderly,” “obesity,” “adiposity,” “children and adolescents,” “HIV,” “animals,” “physical parameters,” “transgenders,” “Brazilian normality data,” and “clinical applicability.” Due to the extent of the position statement, it was divided into two parts. Part I was dedicated to a revision of methods for evaluation of body composition and their technical aspects, and Part II focused on the interpretation of results and clinical applications.
A total of 131 articles were reviewd for the preparation of this second part of the Position Statement. All articles were carefully analyzed first by the groups of authors and then by the ABRASSO Steering Committee. Using electronic correspondence (email), the collaborators in each group discussed the articles based on their expertise until they reached a consensus regarding the best and most current scientific evidence. The final questions presented in this second part of the Position Statement were chosen by the ABRASSO Steering Committee and by experts in body composition assessment using DXA. These questions were based on the main questions and problems encountered in clinical practice concerning the clinical aspects of body composition assessment by DXA and are presented into the following sections: clinical aspects, interpretation, reporting, and special situations. Finally, the authors and the ABRASSO Steering Committee prepared a statement answering each question based on current scientific evidence. Using a Likert scale, the final agreement level (from 0 to 100%) was reached through electronic voting among all collaborators for all 10 statements (Table 2).
Section I: Interpretation
1. What are the validated criteria for bone mass assessment?
The Official Position of the International Society for Clinical Densitometry (ISCD) recommends reports of DXA body composition in adults to include measurement of whole-body (including head) BMD and BMC [7, 8]. However, these measurements are not used as isolated skeletal health markers nor as diagnostic of osteoporosis or low bone mass in adults [7, 9]. Both the ISCD and our guidelines establish that the diagnostic criteria of the World Health Organization (WHO) for densitometric osteoporosis only apply to the skeletal sites of the proximal femur (femoral neck and total hip), lumbar spine (L1–L4), and 33% radius. [7,8,9] The only exception is the use of total body less head (TBLH) bone mass Z-score values as a diagnostic criterion of low bone mass in pediatric patients (5–19 years of age), with an adopted cutoff value of − 2.0 standard deviations (SDs) of the mean value obtained from individuals of the same age [7, 9]. The 1999–2004 National Health and Nutrition Examination Survey (NHANES) reference data for total body BMC should be adopted when DXA is used for body composition assessment in children. The data comprise calculated Z-scores and percentiles for children as young as 8 years of age and adults aged up to 85 years, men and women, and Whites, Blacks, and Mexican Americans. Still, NHANES reference data are not available for many ethnic minorities. Also, more country-specific reference datasets should be developed [10].
In summary, reports of body composition assessed by DXA should include the following:
-
BMC results (in grams), which should always be reported.
-
BMD values (in grams/cm2) and Z-scores (SDs) should be reported for adults but without establishing a diagnosis of osteopenia or osteoporosis.
-
TBLH and Z-scores should be reported in children and adolescents.
-
The sentence “The diagnostic criteria proposed by the WHO are not applicable to whole-body DXA analyses.”
Statement 1
The WHO criteria for densitometric osteoporosis only apply to the skeletal sites of the proximal femur (femoral neck and total hip), lumbar spine (L1–L4), and 33% radius. The only exception is the use of total body less head (TBLH) bone mass Z-score values as a diagnostic criterion of low bone mass in pediatric patients, with an adopted cutoff value of − 2.0 standard deviations (SDs) of the mean value obtained from individuals of the same age. The NHANES III reference database for total body BMC should be adopted when DXA is used for body composition assessment in children.
Body composition DXA reports regarding bone mass should include:
-
BMC results (in grams);
-
BMD values (in g/cm2) and Z-scores (SDs) should be reported for adults, but without establishing a diagnosis of osteopenia or osteoporosis. For individuals with Z-score values below − 2.0 SD, the sentence “low bone mass for age” may be reported;
-
TBLH and Z-scores should be reported in children and adolescents.
2. What are the criteria for assessing fat mass?
Body mass index (BMI) is a measure of weight adjusted for height or length. In some circumstances, BMI values may reveal an individual's excess weight, which is not always reflective of excessive fat, for example, in the case of heavily muscled persons. For this reason, DXA body composition has been recommended for assessing parameters including fat mass index (FMI), abdominal visceral adipose tissue (VAT), and android-to-gynoid (A/G) fat ratio.
-
FMI This index evaluates the ratio of total body fat (in kilograms) to squared height (in square meters) [11]. FMI is advantageous over BMI since BMI may correlate poorly with body fat in some populations [12]. In this sense, patients with increased lean mass may be falsely classified as overweight based on BMI but not on FMI. For calculation of FMI, 1999–2004 NHANES data are used [13]. The criteria for classifying body fat based on FMI are shown in Table 3, with different cutoff values for men and women. Clinical applications for FMI have not been clearly established yet, and prospective studies are still needed to better evaluate and validate this method. Of note, consensuses on cutoff values for defining obesity categories using FMI are currently lacking [10].
-
Estimated abdominal VAT visceral fat is associated with cardiometabolic risk factors including diabetes mellitus, dyslipidemia, hypertension, and metabolic syndrome [14] and is a predictor of coronary heart disease, according to a prospective European study [15]. Compared with subcutaneous fat, VAT is a better predictor of mortality [16]. Only a few DXA systems are able to measure VAT. This measurement is performed in an area 5-cm thick located 1 cm above the iliac crest, approximately at the level of the L4 vertebra, and is calculated as android fat minus subcutaneous fat. VAT measured by DXA correlates highly with visceral fat measured by CT [17, 18], is associated with lower radiation exposure, and is highly accurate. In a cross-sectional study including healthy women, VAT correlated positively with glycemia levels and with the homeostatic model assessment insulin resistance index (HOMA; a method for assessing insulin resistance) and negatively with HDL-cholesterol [19]. Other studies have analyzed the association between VAT measured by DXA and cardiovascular risk parameters [20, 21]. A cross-sectional study including 2,317 US adults aged 18–74 years determined, based on receiver operating characteristic (ROC) curves, a VAT threshold of 126 cm2 (76% sensitivity, 68% specificity) to identify individuals with two or more cardiometabolic risk factors [22]. Indeed, VAT may replace the A/G ratio in assessing cardiometabolic risk factors. Although population studies have established reference values for VAT [23,24,25], the values still need to be standardized, especially with prospective studies assessing cardiometabolic risk factors and cardiovascular outcomes [10].
-
A/G fat ratio this ratio is analogous to the waist/hip ratio and correlates with dyslipidemia in men and women, mortality in women, and risk of myocardial infarction [26, 27]. The A/G fat ratio may be assessed with DXA. The android region comprises the area located between the ribs and the pelvis, with an upper demarcation at 20% of the distance between the iliac crest and the neck and a lower demarcation at the top of the pelvis. The gynoid region comprises the area located between the hip and the upper thighs, with an upper demarcation below the top of the iliac crest at a distance of 1.5 times that of the android height. The total height of the gynoid region is two times the height of the android region [28]. A study analyzing 2005–2006 NHANES data has shown that the correlation with cardiometabolic risk factors was much stronger for the A/G percent fat ratio compared with the android percent fat, gynoid percent fat, or BMI [29]. In contrast, another study showed that DXA-measured abdominal fat and A/G fat ratio were not superior to waist circumference or CT-measured intra-abdominal fat areas in detecting metabolic risk factors in obese women [30]. The A/G ratio varies among individuals of different ethnicities [31].
Statement 2
Recommendations for assessment of fat mass include the fat mass index (FMI; in kg/m2), interpreted according to the NHANES III cutoff values, the estimated abdominal visceral adipose tissue (VAT; in g/cm3 if assessed with a GE-Lunar device or g/cm2 if assessed with a Hologic device), and the android-to-gynoid (A/G) fat ratio.
3. What are the validated criteria for assessing lean mass?
Several validated criteria are available for assessing lean mass using DXA, e.g., the Baumgartner criteria, the Newman criteria, and the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project criteria. However, the accuracy of DXA-measured lean mass is still questionable [32, 33]. Appendicular lean mass (ALM), a sum of lean mass values in the upper and lower limbs, has shown a consistent correlation with muscle mass throughout life [34]. The sections below include a discussion about the criteria defining sarcopenia.
(a) Baumgartner criteria
Baumgartner et al. [35] were pioneers in proposing a method to identify low ALM using DXA. Based on the fact that absolute lean mass correlates strongly with height, the authors calculated the relative muscle mass (or ALM index [ALMI]) as ALM (in kg) divided by the squared height (in square meters, m2), similarly to using BMI to estimate weight excess. The authors defined low muscle mass/sarcopenia as an ALMI ≥ 2 SDs below the sex-specific mean values from the Rosetta Study, a reference population of 18–40-year-old adults. Therefore, according to Baumgartner et al. [35], the cutoff values for sarcopenia were ALMI < 7.26 kg/m2 in men and < 5.45 kg/m2 in women. Further analysis of the elderly population included in the cross-sectional study by Baumgartner et al. [35] found that the prevalence of low muscle mass/sarcopenia increased with age and was associated with higher degrees of self-reported physical disability. Since reference values for low ALM in young Black and White adults have not been established, recent consensuses recommend the definition of low ALM as the finding of lean mass value below the 20th percentile of distribution of values for healthy young adults, with some authors considering the cutoff values of ≤ 7.23 kg/m2 in men and ≤ 5.67 kg/m2 in women [36, 37]. Also, studies have shown significant differences in the prevalence of low lean mass in Asian compared with White populations when the same definition was used, highlighting the importance of reference values based on population-specific data [10].
(b) Newman criteria
The Baumgartner criteria appear to underestimate the prevalence of sarcopenia in several elderly populations [36,37,38,39,40], including community-dwelling older women in Brazil [40]. This is because the formula proposed by Baumgartner et al. (ALM/squared height) is unable to adequately identify sarcopenia in overweight and obese individuals. Lean mass is generally greater in obese compared with lean individuals because both lean mass and fat mass increase with weight gain, usually at an approximate proportion of 1:4 [41]. Due to the interrelation between lean mass and fat mass, obese individuals may not be considered sarcopenic, but their muscle mass may be inadequate for their body size and physical performance [36]. Therefore, Newman et al. proposed ALM to be adjusted for both height and total fat mass. The authors' methodology includes a statistical linear regression model to characterize the association between ALM and height (in meters) and fat mass (in kilograms). Linear regression residuals are used to identify individuals whose ALM value (obtained with DXA) is below the expected value (obtained from the equation resulting from the model) for a given amount of fat mass. The ALM value resulting from the equation (expected muscle mass) must be subtracted from the ALM value obtained by DXA (actual muscle mass), resulting in the ALM residual. Thus, positive residuals indicate adequate muscle mass, while negative residuals indicate relative sarcopenia [36]. Most studies adopting this classification used the 20th percentile of the residuals distribution as a cutoff value for sarcopenia, since the mean values of lean mass and fat mass in younger populations are not considered as reference values [40, 42]. This approach correlates with functional limitation and inflammation markers in older individuals [43].
The prevalence of low lean mass/sarcopenia is generally higher when assessed using the Newman criteria compared with the Baumgartner criteria, especially in overweight/obese populations. For example, in community-dwelling women over the age of 65 years in Brazil, the prevalence of low lean mass was 3% according to the Baumgartner criteria and 19% according to the Newman criteria, in which lean mass is adjusted for body fat [40].
The Newman criteria are relevant in epidemiology but have limited applicability to individual cases in clinical practice since they rely on the construction of a linear regression model specific to each population analyzed. Thus, the equation for calculating the expected ALM obtained from the regression model and, consequently, the residuals (cutoff values for definition of sarcopenia) vary according to the study population. For example, in the São Paulo Aging Health (SPAH) study, the equations obtained for calculating the expected ALM for elderly individuals in Brazil according to sex were as follows: [40]
The residuals (cutoff values below which an individual is considered sarcopenic) are − 1.45 in women and − 2.06 in men [40, 42].
(c) Foundation for the National Institutes of Health (NIH) criteria
Both the Newman and Baumgartner criteria are based exclusively on the statistical distribution of lean mass within a single population [35, 36]. However, the correlation of lean mass with muscle strength and function, which are directly linked to physical performance, remains unclear. Additionally, none of these criteria have been validated on their ability to predict relevant clinical outcomes, such as immobility, fractures, and mortality.
The FNIH has compiled and analyzed longitudinal data from different studies to develop definitions of low lean mass and muscle weakness [44,45,46,47,48]. The project was based on the clinical paradigm of differential diagnosis among physically limited individuals because of weakness and individuals who are weak from having low muscle mass. The project sought to determine the degree of muscle mass that contributes to muscle weakness (clinically relevant low lean mass). Gathering data from eight longitudinal cohort studies and six clinical trials using a regression model (classification and regression trees [CART]), the project defined specific cutoff values for manual handgrip strength, which is associated with lower functional capacity defined by gait speed < 0.8 m/s, and for ALM, measured by DXA, which in turn is associated with handgrip strength. Since sensitivity analyses also indicated that obesity influences the relationship between lean mass and muscle strength, the cutoff values were further adjusted for BMI.
Thus, clinically relevant cutoff values for low ALM adjusted for BMI (ALM [in kg] divided by BMI in [kg/m2]) for elderly individuals according to sex are: < 0.512 for women and < 0.789 for men [46]. These are the first criteria based on a clinically relevant outcome (gait speed), which is directly related to muscle dysfunction, and the most comprehensive criteria in terms of populations, since they derive from multiple cohorts of community-dwelling elderly individuals from different populations worldwide [44,45,46,47,48].
(d) Appendicular lean mass adjusted for fat mass index
Since adjusting lean mass values for adiposity appears to improve the association of lean mass with physical function, the NHANES developed a method to define adiposity-adjusted low lean mass, i.e., the adipose mass index, defined as total body fat mass (in kilograms) divided by squared height (in square meters) [49]. Data from whole-body DXA scanning of 14,850 adults (20–85 years) comprised a database that generated specific SDs for ALMI (kg/m2) and FMI (kg/m2) according to sex and race (Z-score) and relative to age (T-score relative to the age of 25 years). Sarcopenia was defined as a T-score below − 2.0 and low lean mass for age as a Z-score below − 1.0. The results of this study reinforce the importance of adjusting lean mass for body fat in addition to height, as approximately twice more individuals are categorized as sarcopenic based on FMI-adjusted lean mass compared with the unadjusted criteria.
(e) Physical parameters
Considering that the currently validated criteria for defining low lean mass (Baumgartner, FNIH, and Newman) only identify an individual as having low lean mass or lean mass within normal values and are limited in analyzing sarcopenia or cachexia, we provide a brief comment regarding the main physical tests used to assess muscle strength and performance in clinical practice.
Lean mass can also be assessed using muscle strength parameters. Muscle mass and strength are known to decline with aging [50], especially after the age of 40 years, with a 5% decline at each decade after that. After 40 years, the lean mass assessment becomes even more important, considering that low lean mass is an important risk factor for sarcopenia and bone mass loss [51]. The most affected muscles are the knee extensors and hip flexors, which are fundamental for walking and balance maintenance. A decline in these muscles' function is accompanied by an increased rate of falls and their consequences (e.g., fractures), especially in the elderly population [52, 53]. Additionally, muscle strength assessed by the handgrip test correlates strongly with DXA-assessed BMD [54].
Muscle strength in the trunk and upper and lower limbs can be measured by dynamometry. Dynamometers are instruments that measure isometric muscle strength in the upper limbs (handgrip), trunk (trunk extensors), and lower limbs (hip flexors and knee extensors). Muscle strength can also be measured by indirect and dynamic physical fitness and functional capacity tests evaluating static and dynamic balance, mobility, and flexibility [55,56,57]. These tests identify indirect parameters of muscle strength, such as the chair-stand test, which evaluates lower limb strength and dynamic balance.
The Cybex (or isokinetic chair) can also be used to assess lean mass. This method measures muscle strength and variables such as muscle power and resistance, which can be analyzed for each muscle group alone with fixed speed and variable resistance. Disadvantages of the isokinetic chair include high cost and limited availability in clinical practice. Thus, dynamometers are more advantageous than Cybex since they are portable, reliable, less expensive, and easy to access and handle [58].
The long and short versions of the International Physical Activity Questionnaire (IPAQ) (simplified version) is widely used in Brazil and other countries for assessing physical activity level, measured as a report of the time spent on activities of moderate and vigorous intensity for at least 10 continuous minutes in one usual week. The questionnaire considers physical activities related to work, household chores, transportation, exercise, sports, leisure, family care, and time spent seated [59].
Table 4 shows the main physical fitness tests that can be performed, including the muscle groups evaluated and the tests' objectives, methodology, and results [60, 61].
These tests and questionnaires can draw a physical fitness profile of the patients in terms of muscle strength, functional mobility, and static and dynamic balance. They also identify the patients as sedentary or physically active and assess their cardiovascular fitness and risk of falls for planning physical training and treatment strategies.
3.1. Sarcopenia
Sarcopenia, a syndrome closely related to aging, is characterized by progressive and generalized loss of skeletal muscle mass and strength that increases the risk of adverse outcomes, including falls and fractures, physical disability and mobility disorders, cardiorespiratory disease, cognitive impairment, loss of quality of life and independence, and death [62, 63]. Physical performance evaluation and qualitative assessment are required for a complete diagnosis of sarcopenia. In the absence of this qualitative evaluation, the DXA report should be limited to mentioning the occurrence of “low muscle mass” without establishing a diagnosis of sarcopenia [10].
The most widely accepted consensus on the definition of sarcopenia is by the European Working Group on Sarcopenia in Older People (EWGSOP), first published in 2010 and updated in 2019 (EWGSOP2) [62, 63]. Muscle strength is the most reliable measure of muscle function, and the EWGSOP2 adopts low muscle strength as the primary parameter of sarcopenia. The occurrence of sarcopenia is likely when low muscle strength is detected, and the diagnosis is confirmed in the presence of low muscle quality or quantity. When low muscle strength, low muscle quality or quantity, and low physical performance are all detected, sarcopenia is considered severe [62]. Of note, muscle strength is not dependent on muscle mass alone, and the relationship between strength and muscle mass is not linear [64]. Thus, the definition of sarcopenia comprises several factors, including hormonal, inflammatory, biochemical, nutritional, and functional parameters considered in terms of muscle mass quantity and quality.
The first step of the EWGSOP2 algorithm for case finding is the 5-item SARC-F questionnaire, a self-reported screening test for sarcopenia. The SARC-F is a convenient and inexpensive method for screening sarcopenia and has a low-to-moderate sensitivity and a very high specificity to predict low muscle strength (Table 5) [62, 65, 66]. The second step of the algorithm is to assess muscle strength through handgrip strength and compare the results with data from reference populations [62, 67]. If the handgrip strength assessment is not feasible due to hand disability, the chair-stand test can be used as a proxy to assess leg (quadriceps) muscle strength [62]. The next step is to confirm the diagnosis of sarcopenia by measuring muscle mass, preferably by DXA, the recommended method in clinical practice. According to the EWGSOP2, cutoff values for low muscle mass assessed by CT and MRI have not been well defined yet. The cutoff values for DXA-assessed ALMI adjusted for squared height are < 7.0 kg/m2 in men and < 5.5 kg/m2 in women [62].
Assessment of sarcopenia severity should include physical performance evaluation using the timed up and go (TUG) test or, preferably, the gait speed test (speed values ≤ 0.8 m/s identify a compromised gait speed). Other tests that can also assess sarcopenia severity are the 400-m walk test and the Short Physical Performance Battery (SPPB) [62].
More recently, the FNIH Sarcopenia Project defined normative cutoff values for handgrip strength in men and women older than 65 years (Table 6) [44, 45].
According to the Sarcopenia Definition and Outcomes Consortium, DXA-assessed lean mass measurements should not be included in the definition of sarcopenia as they are not good predictors of self-reported mobility limitations and other health-related outcomes such as falls, hip fracture, and mortality [68].
Still lacking a clear definition, sarcopenic obesity is a distinct condition marked by fat infiltration of muscle and associated with decreased physical function and increased risk of mortality and physical disability [62].
3.2. Cachexia
Cachexia is a complex metabolic syndrome associated with an underlying disease and characterized by loss of muscle with or without loss of fat mass. Cachexia is associated with cancer, congestive cardiomyopathy, end-stage renal disease, and other diseases, and is often associated with inflammation, insulin resistance, anorexia, and muscle proteolysis [69]. Thus, most individuals with cachexia also have sarcopenia, while most individuals with sarcopenia may not have cachexia. Sarcopenia is one of the elements of the definition proposed for cachexia [69]. According to the Cachexia Consensus Working Group, after excluding some conditions such as starvation, malabsorption, major depression, lipoatrophy, hyperthyroidism, and age-related muscle loss, cachexia is diagnosed in adults by weight loss ≥ 5% (corrected for fluid retention) over ≤ 12 months (or BMI < 20 kg/m2, if undocumented weight loss) in the presence of underlying illness, plus three of the following criteria: [69].
-
Decreased muscle strength (lowest tertile).
-
Fatigue.
-
Anorexia (total caloric intake < 20 kcal/kg of body weight/day, < 70% of the usual food intake), or lack of appetite.
-
Low FFM index.
-
Abnormal biochemical tests: anemia (< 12 g/dL), low serum albumin (< 3.2 g/dL), and increased inflammatory markers (C-reactive protein > 5.0 mg/L or interleukin-6 > 4.0 pg/mL).
A cachexia score (CASCO) has been designed for cancer patients, but this subject is outside of the scope of the present document [70].
Statement 3
Several validated criteria are available for assessing appendicular lean mass using DXA, including the Baumgartner criteria, the Newman criteria, and the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project criteria.
Lean mass can also be assessed using muscle strength parameters, including dynamometry and indirect and dynamic physical fitness and functional capacity tests evaluating static and dynamic balance, mobility, and flexibility, such as the chair-stand test and isokinetic chair.
Section II: Reporting
4. Which parameters should be included in the DXA body composition report?
For adults older than 20 years, report whole-body (including head) values of:
-
Anthropometry weight (kg), height (m), and BMI (kg/m2).
-
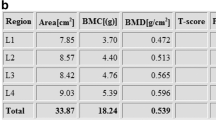
Bone mass compartment BMD (g/cm2), BMC (g), and Z-score (in SDs).
-
Fat mass compartment total fat mass (in kilograms), percentage of fat (in %), FMI (total fat mass/height2, in kg/m2), A/G ratio, and VAT (in g and cm3).
-
Lean mass compartment total lean mass (kg), ALM (kg), ALMI (adjusted by height [ALM/height2] and adjusted by BMI in patients over 65 years old [ALM/BMI]); should be cited in all reports [10, 46].
Figure 1 shows a DXA report proposed by ABRASSO.
Statement 4
For adults older than 20 years, report whole-body (including head) values of:
-
Anthropometry weight (kg), height (m), and BMI (kg/m2).
-
Bone mass compartment BMD (g/cm2), BMC (g), and Z-score (in SDs).
-
Fat mass compartment total fat mass (in kilograms), percentage of fat (in %), FMI (total fat mass/height2, in kg/m2), A/G ratio, and VAT (in g and cm3).
-
Lean mass compartment total lean mass (kg), ALM (kg), ALMI (adjusted by height [ALM/height2] and adjusted by BMI in patients over 65 years old [ALM/BMI]).
5. What should be taken into account regarding quality control, accuracy, and least significant change (LSC)?
The quality control program should adhere to the manufacturer's guidelines for system maintenance. According to the ISCD recommendations, quality control should include: [71].
-
Periodic (at least once a week) phantom scans for any DXA system as an independent assessment of system calibration.
-
Plotting and reviewing of data from calibration and phantom scans.
-
Establishment and enforcement of corrective action thresholds that trigger a call for service.
About precision, ISCD recommends that:
-
The precision error supplied by the manufacturer should not be used.
-
Each DXA device should have its own precision error determined and LSC calculated. The LSC is calculated the same way as done for BMD sites according to ISCD protocol: 15 patients three times, or 30 patients two times, repositioning the patient after each scan, calculate the root mean square standard deviation (RMS-SD) for the group and finally calculate the LSC with 95% confidence intervals for the group. A change is considered significant when the difference between the previous and the new values of total fat mass and total lean mass is above the LSC.
-
The technician should perform an in vivo precision assessment for all body composition values of interest using patients representative of the population of patients from the clinic. This procedure should be repeated when the technician's level changes. The minimum acceptable precision values for an individual technician are 3%, 2%, and 2% for total fat mass, total lean mass, and percent fat mass, respectively. If more than one technician works on the same DXA device, an average precision error combining data from the entire team should be used to establish precision error and LSC for the facility, providing the precision error for each technician is within a pre-established range of acceptable performance.
-
The precision assessment should be repeated when a new DXA system is installed, and cross-calibration should be done by a technician by performing 10 phantom scans with repositioning, before and after a hardware change. If a difference greater than 2% in the mean fat mass, percent fat mass, or lean mass is observed, the manufacturer should be contacted for service [71].
The imprecision of body composition measurements, especially in subregions, can be much larger and more variable than for regional BMD scans. Precision may vary according to device and scan mode, subregion and compartment, body habitus, and age. Caution is advised when considering soft tissue results from subregions of whole-body scans. In general, lean mass precision is better than fat mass precision. A trend has been observed for greater precision for recent models of Hologic and GE-Lunar systems [28].
Although body composition phantoms are part of any body composition teaching course, they were not completely addressed in this manuscript because they are unavailable in most centers. The procedure of quality control in bone mass studies follows a schedule set by the equipment manufacturer and uses either phantoms with density similar to lean and fat mass (GE-Lunar) or an internal calibration system through lean and fat tissue equivalents (Hologic).
Statement 5
The quality control program should adhere to the manufacturer's guidelines for system maintenance. The quality control should include:
-
Periodic (at least once a week) phantom scans for any DXA system as an independent assessment of system calibration.
-
Plotting and reviewing of data from calibration and phantom scans.
-
Establishment and enforcement of corrective action thresholds that trigger a call for service.
-
The precision error supplied by the manufacturer should not be used.
-
Each DXA device should have its own in vivo precision error determined and LSC calculated for all body composition variables.
6. What are the differences between normative data for the Brazilian compared with other populations?
There is currently a lack of normative data regarding body composition assessed by DXA for the Brazilian population or comparing such data with those from other populations. Data from a few Brazilian studies (Brazilian Osteoporosis Study [BRAZOS] and from the Brazilian Institute of Geographic and Statistics [Instituto Brasileiro de Geografia e Estatística, IBGE]) [72, 73] and international studies [74, 75] have reported a similar increment of overweight and obesity rates defined by BMI categories.
A Brazilian study conducted by Sousa et al. evaluated body composition data of 500 women older than 20 years (245 of whom were premenopausal) with BMI between 18.5 and 34.9 kg/m2 using DXA (GE-Lunar) and reported a bimodal variation for body fat, with increasing values until the age of 50–59 years followed by a reduction to the lowest levels at the age of 80 and above. The authors also reported that FMI was consistently higher in African American and Hispanic American women compared with Brazilian women, and that ALMI (ALM/height2, Baumgartner criteria) was consistently lower in women in Brazil compared with those in the US, regardless of age or ethnicity. Lean body mass showed minor deterioration and decreased from the ages of 50–59 years onward, reaching the lowest values in older (≥ 80 years) women [76].
In another Brazilian study, Ushida et al. assessed 403 men older than 20 years and found that the distribution of body composition assessed by DXA (GE-Lunar System) and adjusted to BMI differed between the study population and other ethnic groups [77]. Compared with the NHANES III data assessed with DXA Hologic [13], fat and lean mass index tended to be lower in men in Brazil compared with those in North America. When the authors used NHANES III DXA data converted from Hologic to Lunar-GE [78], the values between the populations remained different for fat mass, especially in older age groups, but became similar regarding lean mass [77]. The authors reported FMI values similar to those for the US population (3–6 kg/m2) as normative for men in Brazil [77]. However, the cutoff value for ALMI recommended by Baumgartner et al. [35] was higher than that reported in the Brazilian study (7.26 kg/m2 for individuals aged 20–29 years and 6.6 kg/m2 for normal BMI).
Carvalho et al. evaluated 689 adults aged 20–59 years in Brazil using DXA (GE-Lunar) to establish percentile curves for measures and indices of body composition by age and sex. The cutoff values for ALMI, derived from 204 men and 221 women aged 20–39 years and considering an SD of − 2.0, were 6.34 kg/m2 and 4.45 kg/m2, respectively. [79].
Barbosa-Silva et al., in turn, adopted a − 1 SD cutoff value relative to a reference young population to determine low ALMI in elderly individuals, different than the EWGSOP recommendation. The mean ± SD values of ALMI in young adults obtained by DXA in a follow-up study conducted in 2012 (when the participants were 30 years old) were 8.76 ± 0.99 and 6.44 ± 0.82 kg/m2 for men and women, respectively. Based on that, cutoff values of 7.77 kg/m2 and 5.62 kg/m2 (− 1 SD) were determined for men and women, respectively. Barbosa-Silva et al. also proposed a combination of calf circumference (≤ 34 cm for males and ≤ 33 cm for females) and SARC-F into a modified index that significantly improved the performance of SARC-F for screening sarcopenia [66, 80, 81].
Machado et al. followed up 433 community-dwelling women (mean age 72.8 ± 4.7 years) and found 28 incident nonspinal osteoporotic fractures during a mean period of 4.3 ± 0.8 years. After adjustments for age, race, previous fractures, and BMD, the authors found a significant association between the participants' VAT (mass, area, volume) and the incidence of nonspinal fractures among nonobese elderly women, suggesting a potential negative effect of visceral adiposity on bone health in this particular group [82].
Additional population studies including functional analyses are still needed to define cutoff thresholds for sarcopenia and low lean mass in the Brazilian population.
Statement 6
Based on Brazilian normative database studies in adult men and women, the Brazilian population, compared with other populations, has some significant differences in body composition parameters, particularly regarding appendicular lean mass adjusted for height. Cutoff values of 7.77 kg/m2 and 5.62 kg/m2 (− 1 SD) are suggested for men and women. The combination of calf circumference (≤ 34 cm for males and ≤ 33 cm for females) and SARC-F into a modified index significantly improves the performance of SARC-F for screening sarcopenia.
Section III: Special situations
7. What is the application of body composition assessment in pediatrics?
In pediatrics, body composition assessment is important in clinical practice and research settings both as a routine follow-up and in specific diseases. Numerous conditions may potentially interfere with body compartment distribution (lean, fat, and bone mass), including exogenous and endogenous overweight and obesity, environmental and disease-related undernutrition, anorexia, chronic drug therapy (e.g., corticosteroids, chemotherapy), and chronic diseases (e.g., systemic inflammatory disorders, inborn errors of metabolism, muscular dystrophies, and endocrine, gastrointestinal, heart, and pulmonary diseases).
The most frequently used parameter for estimating body composition in routine practice in pediatrics is BMI. However, this index has some limitations, for example, it is unable to identify the percentage of distribution of each body compartment. In some clinical conditions, it is desirable to differentiate and quantify the different body compartments for diagnostic purposes, define therapeutic interventions, or evaluate the impact of a procedure on the overall health of children and adolescents [83, 84]. For instance, it is important to evaluate the extension of fat mass loss in lipodystrophy syndromes. On the other side, greater BMI may signal excessive weight that may not necessarily result from excess fat, e.g., a heavily muscular adolescent. In other scenarios, differentiating subcutaneous from VAT in a pediatric patient with obesity leads to a more emphatic approach to prevent the onset of cardiometabolic disorders.
Other anthropometric measurements, including skinfolds, waist-hip ratio, and abdominal, arm and neck circumferences, are technically easy to perform but are highly observer-dependent and may also present limitations in interpretation [85].
Body composition assessment in pediatrics can also be performed by other methods, including DXA, CT, MRI, plethysmography, and BIA, as done in other stages of life. The advantages and limitations of each method described in previous sessions also apply to the pediatric population [86, 87].
DXA is considered the method of choice for quantitative assessment of body composition in pediatrics due to precision, accuracy, reproducibility, low radiation doses (1–5 µSv), accessibility, cost-effectiveness, and practicability. However, this method has considerable limitations, including age (the child must be older than 2–5 years, depending on the densitometer software), lack of integrative sex/age/pubertal stage and population-specific normative data, and lower precision and accuracy for VAT assessment [1].
Interpretation of pediatric DXA data may be challenging due to physiological changes in body composition during growth. This is especially critical during adolescence, when each pubertal stage has different patterns of lean, fat, and bone mass distribution and acquisition, associated not only with chronological age, but also dependent on bone age and hormonal and metabolic status [88, 89].
Establishing reference data for specific populations is fundamental for an accurate analysis of DXA-acquired body composition, considering the impact of ethnicity, diet, sex, and pubertal stage on body compartment profile and distribution [90, 91]. However, the number of available regional/country reference data on the quantification of pediatric body composition by DXA is limited worldwide; among the few data available for children and adolescents are those from the US [84], Chile [92], Argentina [93], UK [94], China [95], and India [96].
The most robust pediatric DXA database currently available is from the 1999–2004 NHANES, compiling data on BMC, areal mineral density, and lean and fat mass of 412 boys and 931 girls aged 8–19 years in the US [13]. Specifically in Brazil, a recent study reported age- and sex-specific DXA-acquired reference data for lean and fat mass based on the evaluation of 541 adolescents (aged 12–17 years, 170 girls) in the state of Parana [97].
The Brazilian population has unique features compared with other populations. Brazil is a large country with specific genetic background and phenotypic patterns clustered in some regions, and an overall population with substantial ethnic miscegenation, all of which affect body composition. Based on that, a nationwide reference database of DXA-assessed body composition representative of Brazilian children and adolescents would be desirable [98].
In pediatrics, assessment of body composition using DXA should follow the same ISCD standards as those used for adult scanning: fasting, adequate hydration, empty bladder, clothing, and body positioning [28].
Research studies have contributed to a better understanding of the physiological changes in body composition during growth. However, body composition assessment using DXA should be performed judiciously in children and adolescents, considering that no consensually established references are currently available for precise and accurate quantification of different body compartments in this population. Still, the currently available data may be applicable in clinical practice to evaluate the impact of diseases on body composition, offer parameters to define specific interventions on nutritional health, and evaluate the impact of clinical procedures on global health and growth [86, 99, 100].
Increasingly more studies are providing new data on the assessment of body composition by DXA in adolescent athletes, elucidating some of the mechanisms driving the impact of diet and physical activity on body compartments. Results from such studies can optimize the guidance for sports performance and recognize situations that could potentially trigger health risks [101,102,103].
Currently available pediatric data still do not support the analysis of body composition by DXA for population screening or comprehensive monitoring of clinical conditions involving the risk of metabolic and nutritional disorders. The use of the method for assessing nutritional disorders, if carried out, should be judicious, observing the clinical context of each patient [86].
In summary, understanding the advantages and limitations of body composition analysis by DXA and other methods in pediatrics and the changing nature of body composition during childhood and adolescence are essential steps for choosing the best measurement technique for each individual, population, or clinical issue in research settings, as well as the correct interpretation of the obtained data.
Statement 7
Numerous conditions may potentially interfere with body compartment distribution (lean, fat, and bone mass), including exogenous and endogenous overweight and obesity, environmental and disease-related undernutrition, anorexia, chronic drug therapy (e.g., corticosteroids, chemotherapy), and chronic diseases (e.g., systemic inflammatory disorders, inborn errors of metabolism, muscular dystrophies, and endocrine, gastrointestinal, heart, and pulmonary diseases). The most frequently used parameter for estimating body composition in routine practice in pediatrics is the BMI.
Interpretation of pediatric DXA data may be challenging due to physiological changes in body composition during growth, particularly in the absence of Brazilian normative reference data for children and adolescents. Thus, the NHANES III database is also recommended for use in pediatric patients (ages 5–19 years) in Brazil.
8. What is the clinical application of body composition assessment in patients infected with HIV?
Adequate nutritional status is essential for patients infected with HIV since compromised nutrition in this population has been negatively associated with immune system dysregulation, disease progression, morbidity, and mortality. Due to complex and unclear mechanisms, patients infected with HIV may present body composition changes even without weight loss [104, 105]. Therefore, noninvasive methods for body composition assessment are useful to monitor and identify possible changes in this population [105].
HIV-associated lipodystrophy is a condition characterized by abnormal body fat redistribution. Subtypes of this condition included lipoatrophy (peripheral fat wasting, with subcutaneous fat loss in the face, arms, legs, and buttocks), lipohyperthophy (abdominal visceral fat accumulation, neck enlargement, gynecomastia, and development of dorsocervical fat pad or “buffalo hump”), and a phenotype of mixed (combined) lipodystrophy, with the clinical presentation of both lipoatrophy and lipohypertrophy [104,105,106]. Although first described in adults, HIV-associated lipodystrophy can also occur early in life [107, 108].
Some studies have reported early body composition changes detectable by DXA in pediatric patients infected with HIV, even in those without typical clinically visual signs of lipodystrophy [109, 110]. A study following HIV-infected children into adolescence reported progressive subcutaneous fat loss and greater accumulation of visceral adiposity in those with lipodystrophy [111]. BIA is a cost-effective method to predict lean body mass and total body fat in HIV-infected children but requires specific prediction equations [105, 112], is unable to assess body fat redistribution, and may be imprecise in patients with lipodystrophy [104]. A Brazilian study comparing body composition assessment with BIA versus DXA in pre-pubertal HIV-infected children showed a high homogeneity between both methods for total body fat but no concordance regarding FFM [112].
Anthropometric measurements are also useful in assessing body composition in HIV-infected persons [105]. The trunk-to-arm skinfold ratio (the sum of the subscapular and suprailiac skinfolds divided by the sum of the biceps and triceps skinfolds) may be a useful parameter of body fat redistribution [107] and correlates inversely with the limb-to-trunk fat ratio (the sum of the fat mass in the arms and legs divided by the fat mass in the trunk) obtained by DXA [108]. Of note, ratios such as trunk/limb fat, trunk/leg fat, fat mass ratio, and even trunk or limb fat as a percent of total fat are unable to fully differentiate between peripheral fat loss and central fat gain; however, they may be useful and must be interpreted with caution [10].
Bone metabolism in HIV-infected persons can be affected by several factors, including antiretroviral drugs and the infection itself. Low BMD for chronologic age is reported in HIV-infected children and adolescents and may result in suboptimal peak bone mass in adulthood [113, 114]. Additionally, adults with HIV have a high risk of osteopenia, osteoporosis, and low BMD [115, 116].
According to the American Dietetic Association (ADA) [105], there is plenty of evidence for assessing body composition in HIV-infected children, adolescents, and adults. The Adult Official Positions of the ISCD recommend DXA total body composition with regional analysis to evaluate fat distribution in patients with HIV using antiretroviral drugs associated with a risk of lipoatrophy (currently stavudine and zidovudine) [71]. The Osteo Renal Exchange Program (OREP), which addresses bone disease in HIV-infected patients, recommends DXA to be performed in the following adults with HIV infection: men aged ≥ 50 years, postmenopausal women, and patients at high risk of falls, with a history of fragility fracture, or receiving chronic corticosteroid treatment [117].
Statement 8
Body composition assessment is recommended in patients infected with HIV for monitoring of body composition changes related to the disease and adverse effects associated with antiretroviral therapy, particularly abnormal body fat redistribution in the HIV-associated lipodystrophy spectrum.
The following parameters may be useful for assessing the presence of lipodystrophy in HIV-infected patients: limb-to-trunk fat ratio, trunk/leg fat ratio, and fat mass ratio.
9. How should body composition be assessed in transgender individuals?
A systematic review has evaluated the bone mass effects of long-term cross-sex hormone therapy (CSHT) in transgender individuals. However, the conclusions had moderate- to low-quality evidence due to studies with an observational design, small sample sizes, and variations in hormone therapy protocols [118].
According to the ISCD statement: (1) gender data should be obtained on the intake questionnaire; (2) T-scores should be calculated using a uniform Caucasian (non-race adjusted) female normative database for all transgender individuals of all ethnic groups and be used in all transgender individuals age 50 years or older, regardless of hormonal status; (3) Z-scores should be calculated using the normative database that matches the gender identity of the individual (both male and female databases if requested); (4) in gender-nonbinary individuals, the normative database that matches the sex recorded at birth should be used [71].
Several factors can interfere with bone, lean, and fat mass in transgender individuals, e.g., the time elapsed since gonadectomy and beginning of hormone therapy, use of GnRH analogs, adherence or use of inadequate CSHT doses, presence of other risk factors for bone loss, associated diseases, and medications (e.g., corticosteroids) [71, 119]. However, no consistent data about body composition in transgender individuals are available at this time.
Statement 9
Consistent data on body composition assessment in transgender individuals are currently unavailable. Until studies with more consistent data are published, we recommended the calculation of T-scores using a uniform Caucasian (non-race adjusted) female normative database for all transgender individuals of all ethnic groups and all transgender individuals aged 50 years or older, regardless of hormonal status. Z-scores should be calculated using the normative database that matches the gender identity of the individual (or based on both male and female databases, if requested by the physician). In gender-nonbinary individuals, the normative database that matches the sex recorded at birth should be used.
Perspective
10. What is the role of DXA in veterinary medicine and zootechnics?
The topic of DXA use in animal studies has not been explored much in the literature and brings an interesting perspective regarding other innovative applications of this technique.
The relatively recent introduction of DXA in veterinary medicine and animal sciences demonstrates the vast potential of applicability of the method in these areas. Historically, Kronacher and Hogreve were pioneers in using noninvasive diagnostic methods in animals, using x-ray to analyze the pelvis in pigs [120]. In vivo body composition measurement by DXA has been obtained from porks [121], broilers [122], and sheep [123]. There are also examples of the application of DXA as a reliable technique and alternative to traditional methods in the evaluation of body composition in ovine carcasses [124], pigs [125, 126], broilers [127], and beef carcass sides and primal cuts [128].
Mawby et al. [129] used DXA to analyze the body composition of dogs with obesity due to malnutrition. German et al. [130] evaluated the body condition score (BCE) and DXA scanning in dogs to estimate changes in weight and body composition and found that the animals had increased lean mass, lower fat mass, and decreased weight and BCE. Reference values for body composition and age and gender differences can be obtained from healthy adult cats using DXA scanning; these values allow for monitoring of nutritional status, assessment of skeletal muscle development, and investigation of metabolic and endocrine disorders [131]. The reference values also have the potential to evaluate the effectiveness of feeding interventions on the amount of lean and fat mass, for example, with the commercial purpose of selling animals with less fat and greater lean content or vice versa.
Of note, the recent use of DXA in veterinary medicine has proven to be valid, reliable [123, 125, 126, 129], and reproducible, confirming that DXA is an excellent potential instrument for applications in animal health and production. However, reference values at different animal ages are still required to monitor body changes during lactation, analysis of data after use of nutritional additives, monitoring of dietary regimes, or even experimentally- or naturally-induced obesity.
Statement 10
DXA can be used in veterinary medicine and animal sciences for measurement of whole-body composition in pigs, broilers, cats, dogs, and sheep, among others. Although normative data in these animals are scarce, this technique has a great potential in accurately evaluating the effectiveness of feeding interventions on the amount of lean and fat mass.
Conclusion
Of all current technologies for body composition assessment, DXA should be the preferred method since it performs whole-body analyses in a shorter time and with less radiation exposure, providing a particularly accurate analysis of fat parameters. In general, BMD and total body BMC (including head) should not be used as isolated skeletal health markers or to diagnose osteoporosis and low bone mass in adults. BMI may be a measure of weight gain, but not necessarily of excess fat.
The following results should be included in DXA-assessed body composition reports: anthropometric data, total fat mass, percentage of fat mass, FMI, VAT, A/G ratio, ALMI (Baumgartner criteria), and BMI-adjusted lean mass index (FNIH for over 65-year-old individuals).
The diagnosis of sarcopenia is based on low muscle mass associated with low muscle strength or performance; these parameters can be evaluated by handgrip strength and gait speed, which are the tests mostly used for this purpose in clinical practice. Lean mass measurement has some limitations and is not included in the definition of sarcopenia issued by some medical societies.
Special care is recommended regarding quality control and LSC calculation to allow for accurate and reproducible measurements and longitudinal control when the patient's condition requires follow-up assessments.
Data interpretation in pediatric patients is challenging, partially due to continuous physiological changes in body composition during linear growth, especially during adolescence. DXA-assessed body composition in pediatrics is particularly interesting in chronic diseases, mainly those involving nutritional disorders and muscle mass. Trunk/limb fat ratio, trunk/leg fat ratio, and fat mass ratio assessed by DXA may be useful in HIV-infected patients to assess the presence of lipodystrophy.
No consistent data on body composition assessment in transgender individuals are available currently.
In veterinary medicine, DXA has been proven valid, reproducible, and a potential tool for assessing animal health.
Availability of data and materials
Not applicable.
References
Kendler DL, Borges JL, Fielding RA, et al. The official positions of the International Society for Clinical Densitometry: indications of use and reporting of DXA for body composition. J Clin Densitom. 2013;16:496–507.
Ward LC. Human body composition: yesterday, today, and tomorrow. Eur J Clin Nutr. 2018;72:1201–7.
Teigen LM, Kuchnia AJ, Mourtzakis M, Earthman CP. The use of technology for estimating body composition: strengths and weaknesses of common modalities in a clinical setting [formula: see text]. Nutr Clin Pract. 2017;32:20–9.
Prospective Studies C, Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Lemos T, Gallagher D. Current body composition measurement techniques. Curr Opin Endocrinol Diabetes Obes. 2017;24:310–4.
Sinha J, Duffull SB, Al-Sallami HS. A review of the methods and associated mathematical models used in the measurement of fat-free mass. Clin Pharmacokinet. 2018;57:781–95.
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S. Executive summary of the 2013 international society for clinical densitometry position development conference bone densitometry. J Clin Densitom. 2013;16:455–66.
Shuhart CR, Yeap SS, Anderson PA, et al. Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom. 2019;22:453–71.
Brandao CM, Camargos BM, Zerbini CA, et al. 2008 official positions of the Brazilian Society for Clinical Densitometry–SBDens. Arq Bras Endocrinol Metabol. 2009;53:107–12.
Petak S, Barbu CG, Yu EW, et al. The Official Positions of the International Society for Clinical Densitometry: body composition analysis reporting. J Clin Densitom. 2013;16:508–19.
VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr. 1990;52:953–9.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701.
Kelly TL, Wilson KE, Heymsfield SB. Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS ONE. 2009;4:e7038.
Rothney MP, Catapano AL, Xia J, et al. Abdominal visceral fat measurement using dual-energy X-ray: association with cardiometabolic risk factors. Obesity (Silver Spring). 2013;21:1798–802.
Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation. 2007;116:2933–43.
Kang SM, Yoon JW, Ahn HY, et al. Android fat depot is more closely associated with metabolic syndrome than abdominal visceral fat in elderly people. PLoS ONE. 2011;6:e27694.
Kaul S, Rothney MP, Peters DM, et al. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring). 2012;20:1313–8.
Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity (Silver Spring). 2012;20:1109–14.
Miazgowski T, Krzyzanowska-Swiniarska B, Dziwura-Ogonowska J, Widecka K. The associations between cardiometabolic risk factors and visceral fat measured by a new dual-energy X-ray absorptiometry-derived method in lean healthy Caucasian women. Endocrine. 2014;47:500–5.
Bi X, Seabolt L, Shibao C, et al. DXA-measured visceral adipose tissue predicts impaired glucose tolerance and metabolic syndrome in obese Caucasian and African-American women. Eur J Clin Nutr. 2015;69:329–36.
Schousboe JT, Langsetmo L, Schwartz AV, et al. Comparison of associations of DXA and CT visceral adipose tissue measures with insulin resistance, lipid levels, and inflammatory markers. J Clin Densitom. 2017;20:256–64.
Katzmarzyk PT, Greenway FL, Heymsfield SB, Bouchard C. Clinical utility and reproducibility of visceral adipose tissue measurements derived from dual-energy X-ray absorptiometry in White and African American adults. Obesity (Silver Spring). 2013;21:2221–4.
Hirsch KR, Blue MNM, Trexler ET, Smith-Ryan AE. Visceral adipose tissue normative values in adults from the United States using GE Lunar iDXA. Clin Physiol Funct Imaging. 2019;39:407–14.
Miazgowski T, Kucharski R, Soltysiak M, Taszarek A, Miazgowski B, Widecka K. Visceral fat reference values derived from healthy European men and women aged 20–30 years using GE Healthcare dual-energy x-ray absorptiometry. PLoS ONE. 2017;12:e0180614.
Ofenheimer A, Breyer-Kohansal R, Hartl S, et al. Reference values of body composition parameters and visceral adipose tissue (VAT) by DXA in adults aged 18–81 years-results from the LEAD cohort. Eur J Clin Nutr. 2020;74:1181–91.
Wiklund P, Toss F, Weinehall L, et al. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J Clin Endocrinol Metab. 2008;93:4360–6.
Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170:1293–301.
Hangartner TN, Warner S, Braillon P, Jankowski L, Shepherd J. The Official Positions of the International Society for Clinical Densitometry: acquisition of dual-energy X-ray absorptiometry body composition and considerations regarding analysis and repeatability of measures. J Clin Densitom. 2013;16:520–36.
Okosun IS, Seale JP, Lyn R. Commingling effect of gynoid and android fat patterns on cardiometabolic dysregulation in normal weight American adults. Nutr Diabetes. 2015;5:e155.
Lee K, Lee S, Kim YJ, Kim YJ. Waist circumference, dual-energy X-ray absortiometrically measured abdominal adiposity, and computed tomographically derived intra-abdominal fat area on detecting metabolic risk factors in obese women. Nutrition. 2008;24:625–31.
Novotny R, Going S, Teegarden D, et al. Hispanic and Asian pubertal girls have higher android/gynoid fat ratio than whites. Obesity (Silver Spring). 2007;15:1565–70.
Scafoglieri A, Clarys JP. Dual energy X-ray absorptiometry: gold standard for muscle mass? J Cachexia Sarcopenia Muscle. 2018;9:786–7.
Sheean P, Gonzalez MC, Prado CM, McKeever L, Hall AM, Braunschweig CA. American society for parenteral and enteral nutrition clinical guidelines: the validity of body composition assessment in clinical populations. JPEN J Parenter Enteral Nutr. 2020;44:12–43.
Hansen RD, Raja C, Aslani A, Smith RC, Allen BJ. Determination of skeletal muscle and fat-free mass by nuclear and dual-energy x-ray absorptiometry methods in men and women aged 51–84 y (1–3). Am J Clin Nutr. 1999;70:228–33.
Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Newman AB, Kupelian V, Visser M, et al. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51:1602–9.
Delmonico MJ, Harris TB, Lee JS, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55:769–74.
Zoico E, Di Francesco V, Guralnik JM, et al. Physical disability and muscular strength in relation to obesity and different body composition indexes in a sample of healthy elderly women. Int J Obes Relat Metab Disord. 2004;28:234–41.
Lau EM, Lynn HS, Woo JW, Kwok TC, Melton LJ 3rd. Prevalence of and risk factors for sarcopenia in elderly Chinese men and women. J Gerontol A Biol Sci Med Sci. 2005;60:213–6.
Domiciano DS, Figueiredo CP, Lopes JB, et al. Discriminating sarcopenia in community-dwelling older women with high frequency of overweight/obesity: the Sao Paulo Ageing & Health Study (SPAH). Osteoporos Int. 2013;24:595–603.
Heymsfield SB, Wang Z, Baumgartner RN, Ross R. Human body composition: advances in models and methods. Annu Rev Nutr. 1997;17:527–58.
Figueiredo CP, Domiciano DS, Lopes JB, et al. Prevalence of sarcopenia and associated risk factors by two diagnostic criteria in community-dwelling older men: the Sao Paulo Ageing and Health Study (SPAH). Osteoporos Int. 2014;25:589–96.
Cesari M, Kritchevsky SB, Baumgartner RN, et al. Sarcopenia, obesity, and inflammation–results from the Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors study. Am J Clin Nutr. 2005;82:428–34.
Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69:547–58.
Alley DE, Shardell MD, Peters KW, et al. Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol A Biol Sci Med Sci. 2014;69:559–66.
Cawthon PM, Peters KW, Shardell MD, et al. Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci. 2014;69:567–75.
McLean RR, Shardell MD, Alley DE, et al. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. J Gerontol A Biol Sci Med Sci. 2014;69:576–83.
Dam TT, Peters KW, Fragala M, et al. An evidence-based comparison of operational criteria for the presence of sarcopenia. J Gerontol A Biol Sci Med Sci. 2014;69:584–90.
Proctor DN, O’Brien PC, Atkinson EJ, Nair KS. Comparison of techniques to estimate total body skeletal muscle mass in people of different age groups. Am J Physiol. 1999;277:E489-495.
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159:413–21.
Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol. 2012;3:260.
Edwards MH, Dennison EM, Aihie Sayer A, Fielding R, Cooper C. Osteoporosis and sarcopenia in older age. Bone. 2015;80:126–30.
Moreira LD, Oliveira ML, Lirani-Galvao AP, Marin-Mio RV, Santos RN, Lazaretti-Castro M. Physical exercise and osteoporosis: effects of different types of exercises on bone and physical function of postmenopausal women. Arq Bras Endocrinol Metabol. 2014;58:514–22.
Marin RV, Pedrosa MAC, Moreira-Pfrimer LDF, Matsudo SMM, Lazaretti-Castro M. Association between lean mass and handgrip strength with bone mineral density in physically active postmenopausal women. J Clin Densitom. 2010;13:96–101.
Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. 1999;7:129–61.
Pavasini R, Guralnik J, Brown JC, et al. Short physical performance battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016;14:215.
Vestergaard S, Patel KV, Bandinelli S, Ferrucci L, Guralnik JM. Characteristics of 400-meter walk test performance and subsequent mortality in older adults. Rejuvenation Res. 2009;12:177–84.
Martin HJ, Yule V, Syddall HE, Dennison EM, Cooper C, Aihie SA. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology. 2006;52:154–9.
Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Wallmann HW, Evans NS, Day C, Neelly KR. Interrater reliability of the five-times-sit-to-stand test. Home Health Care Manag Pract. 2013;25:13–7.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23.
Delmonico MJ, Harris TB, Visser M, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–85.
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7:28–36.
Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC, Grupo de Estudos em Composicao Corporal e N. Enhancing SARC-F: improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc. 2016;17:1136–41.
Roberts HC, Denison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9.
Bhasin S, Travison TG, Manini TM, et al. Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. J Am Geriatr Soc. 2020;68:1410–8.
Evans WJ, Morley JE, Argiles J, et al. Cachexia: a new definition. Clin Nutr. 2008;27:793–9.
Argiles JM, Lopez-Soriano FJ, Toledo M, Betancourt A, Serpe R, Busquets S. The cachexia score (CASCO): a new tool for staging cachectic cancer patients. J Cachexia Sarcopenia Muscle. 2011;2:87–93.
2019 ISCD official position—adults. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult/. Accessed 13 April 2020.
Pinheiro MM, Ciconelli RM, Jacques Nde O, Genaro PS, Martini LA, Ferraz MB. The burden of osteoporosis in Brazil: regional data from fractures in adult men and women–the Brazilian Osteoporosis Study (BRAZOS). Rev Bras Reumatol. 2010;50:113–27.
Instituto Brasileiro de Geografi a e Estatística (IBGE). Antropometria e Estado Nutricional de Crianças, Adolescentes e Adultos no Brasil. 2010.
World Health Organization. Global status report on noncommunicable diseases 2010—description of the global burden of NCDs, their risk factors and determinants. In: 2010.
Nielson CM, Marshall LM, Adams AL, et al. BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res. 2011;26:496–502.
Sousa M, Pinheiro MM, Szejnfeld VL, Castro CHM. Body composition parameters in healthy Brazilian women differ from white, black, and Hispanic American women reference range. J Clin Densitom. 2013;16:360–7.
Ushida M, de Medeiros PM, de Moura Castro CH, Szejnfeld VL. Body composition analysis by DXA (dual X-ray absorptiometry) in Brazilian men: normative data. J Bone Miner Metab. 2017;35:554–61.
Fan B, Shepherd JA, Levine MA, et al. National Health and Nutrition Examination Survey whole-body dual-energy X-ray absorptiometry reference data for GE Lunar systems. J Clin Densitom. 2014;17:344–77.
Carvalho CJ, Longo GZ, Juvanhol LL, et al. Body composition indices in Brazilian adults: age-specific and sex-specific percentile curves. Arch Endocrinol Metab. 2019;63:358–68.
Victora CG, Barros FC. Cohort profile: the 1982 Pelotas (Brazil) birth cohort study. Int J Epidemiol. 2006;35:237–42.
Barbosa-Silva TG, Bielemann RM, Gonzalez MC, Menezes AM. Prevalence of sarcopenia among community-dwelling elderly of a medium-sized South American city: results of the COMO VAI? study. J Cachexia Sarcopenia Muscle. 2016;7:136–43.
Machado LG, Domiciano DS, Figueiredo CP, et al. Visceral fat measured by DXA is associated with increased risk of non-spine fractures in nonobese elderly women: a population-based prospective cohort analysis from the Sao Paulo Ageing & Health (SPAH) Study. Osteoporos Int. 2016;27:3525–33.
Wells JC. Toward body composition reference data for infants, children, and adolescents. Adv Nutr. 2014;5:320S-329S.
Weber DR, Moore RH, Leonard MB, Zemel BS. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am J Clin Nutr. 2013;98:49–56.
Lohman TG, Hingle M, Going SB. Body composition in children. Pediatr Exerc Sci. 2013;25:573–90.
Weber DR, Leonard MB, Zemel BS. Body composition analysis in the pediatric population. Pediatr Endocrinol Rev. 2012;10:130–9.
Orsso CE, Silva MIB, Gonzalez MC, et al. Assessment of body composition in pediatric overweight and obesity: a systematic review of the reliability and validity of common techniques. Obes Rev. 2020;21:e13041.
Staiano AE, Broyles ST, Gupta AK, Katzmarzyk PT. Ethnic and sex differences in visceral, subcutaneous, and total body fat in children and adolescents. Obesity (Silver Spring). 2013;21:1251–5.
Loomba-Albrecht LA, Styne DM. Effect of puberty on body composition. Curr Opin Endocrinol Diabetes Obes. 2009;16:10–5.
Gordon CM, Leonard MB, Zemel BS, International Society for Clinical D. 2013 pediatric position development conference: executive summary and reflections. J Clin Densitom. 2014;17:219–24.
2019 ISCD Official Positions—Pediatric. https://iscd.app.box.com/s/ae9gusunsr6e0fmxkqxosaczmnuhujx4. Accessed 13 April 2020.
Cossio Bolanos MA, Andruske CL, de Arruda M, et al. Muscle mass in children and adolescents: proposed equations and reference values for assessment. Front Endocrinol (Lausanne). 2019;10:583.
Lifshitz F, Hecht JP, Bermudez EF, et al. Body composition analysis by dual-energy X-ray absorptiometry in young preschool children. Eur J Clin Nutr. 2016;70:1203–9.
Ward KA, Ashby RL, Roberts SA, Adams JE, Zulf MM. UK reference data for the Hologic QDR Discovery dual-energy x ray absorptiometry scanner in healthy children and young adults aged 6–17 years. Arch Dis Child. 2007;92:53–9.
Guo B, Wu Q, Gong J, et al. Relationships between the lean mass index and bone mass and reference values of muscular status in healthy Chinese children and adolescents. J Bone Miner Metab. 2016;34:703–13.
Marwaha RK, Garg MK, Bhadra K, Mahalle N, Mithal A, Tandon N. Assessment and relation of total and regional fat mass with bone mineral content among Indian urban adolescents. J Pediatr Endocrinol Metab. 2015;28:1085–93.
Ripka WL, Orsso CE, Haqq AM, Luz TG, Prado CM, Ulbricht L. Lean mass reference curves in adolescents using dual-energy x-ray absorptiometry (DXA). PLoS ONE. 2020;15:e0228646.
Moura RR, Coelho AV, Balbino Vde Q, Crovella S, Brandao LA. Meta-analysis of Brazilian genetic admixture and comparison with other Latin America countries. Am J Hum Biol. 2015;27:674–80.
Muller MJ, Lagerpusch M, Enderle J, Schautz B, Heller M, Bosy-Westphal A. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev. 2012;13(Suppl 2):6–13.
Helba M, Binkovitz LA. Pediatric body composition analysis with dual-energy X-ray absorptiometry. Pediatr Radiol. 2009;39:647–56.
Nana A, Slater GJ, Stewart AD, Burke LM. Methodology review: using dual-energy X-ray absorptiometry (DXA) for the assessment of body composition in athletes and active people. Int J Sport Nutr Exerc Metab. 2015;25:198–215.
Bilsborough JC, Greenway K, Opar D, Livingstone S, Cordy J, Coutts AJ. The accuracy and precision of DXA for assessing body composition in team sport athletes. J Sports Sci. 2014;32:1821–8.
Ackland TR, Lohman TG, Sundgot-Borgen J, et al. Current status of body composition assessment in sport: review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical Commission. Sports Med. 2012;42:227–49.
Polsky B, Kotler D, Steinhart C. HIV-associated wasting in the HAART era: guidelines for assessment, diagnosis, and treatment. AIDS Patient Care STDS. 2001;15:411–23.
Fields-Gardner C, Campa A, American DA. Position of the American Dietetic Association: nutrition intervention and human immunodeficiency virus infection. J Am Diet Assoc. 2010;110:1105–19.
Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12:F51-58.
Jaquet D, Levine M, Ortega-Rodriguez E, et al. Clinical and metabolic presentation of the lipodystrophic syndrome in HIV-infected children. AIDS. 2000;14:2123–8.
Palchetti CZ, Patin RV, Gouvea Ade F, Szejnfeld VL, Succi RC, Oliveira FL. Body composition and lipodystrophy in prepubertal HIV-infected children. Braz J Infect Dis. 2013;17:1–6.
Brambilla P, Bricalli D, Sala N, et al. Highly active antiretroviral-treated HIV-infected children show fat distribution changes even in absence of lipodystrophy. AIDS. 2001;15:2415–22.
Vigano A, Mora S, Testolin C, et al. Increased lipodystrophy is associated with increased exposure to highly active antiretroviral therapy in HIV-infected children. J Acquir Immune Defic Syndr. 2003;32:482–9.
Palchetti CZ, Succi RCM, Szejnfeld VL, et al. Body composition changes and predictors of lipodystrophy in a cohort of pre-pubertal HIV-infected children. Br J Med Med Res. 2015;8:601–11.
Palchetti CZ, Patin RV, Machado DM, Szejnfeld VL, Succi RC, Oliveira FL. Body composition in prepubertal, HIV-infected children: a comparison of bioelectrical impedance analysis and dual-energy X-ray absorptiometry. Nutr Clin Pract. 2013;28:247–52.
DiMeglio LA, Wang J, Siberry GK, et al. Bone mineral density in children and adolescents with perinatal HIV infection. AIDS. 2013;27:211–20.
Palchetti CZ, Szejnfeld VL, de Menezes Succi RC, et al. Impaired bone mineral accrual in prepubertal HIV-infected children: a cohort study. Braz J Infect Dis. 2015;19:623–30.
Bernardino JI, Mocroft A, Mallon PW, et al. Bone mineral density and inflammatory and bone biomarkers after darunavir-ritonavir combined with either raltegravir or tenofovir-emtricitabine in antiretroviral-naive adults with HIV-1: a substudy of the NEAT001/ANRS143 randomised trial. Lancet HIV. 2015;2:e464-473.
Escota GV, Mondy K, Bush T, et al. High prevalence of low bone mineral density and substantial bone loss over 4 years among HIV-infected persons in the era of modern antiretroviral therapy. AIDS Res Hum Retroviruses. 2016;32:59–67.
Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242–51.
Fighera TM, Ziegelmann PK, Rasia da Silva T, Spritzer PM. Bone mass effects of cross-sex hormone therapy in transgender people: updated systematic review and meta-analysis. J Endocr Soc. 2019;3:943–64.
Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869–903.
Kronacher C HF. Investigations on the causes of rump shape in different breeds of pigs from X-rays studies. Z Zücht. 1936;35.
Mitchell AD, Scholz AM, Pursel VG. Prediction of pork carcass composition based on cross-sectional region analysis of dual energy X-ray absorptiometry (DXA) scans. Meat Sci. 2003;63:265–71.
Gonçalves CA, Sakomura NK, Pereira da Silva E, Artoni SMB, Suzuki RM, Gous RM. Dual energy X-ray absorptiometry is a valid tool for assessing in vivo body composition of broilers. Anim Prod Sci. 2019;59:993–1000.
Miller DW, Bennett EJ, Harrison JL, Anderson F, Adam CL. Dual-energy X-ray absorptiometry scans accurately predict differing body fat content in live sheep. J Anim Sci Biotechnol. 2018;9:80.
Clarke RDKA, Bartle CM, Dobbie PM. Application of dual-energy X-ray absorptiometry for ovine carcass evaluation. Proc N Z Soc Anim Prod. 1999;59:272–4.
Kipper M, Marcoux M, Andretta I, Pomar C. Assessing the accuracy of measurements obtained by dual-energy X-ray absorptiometry on pig carcasses and primal cuts. Meat Sci. 2019;148:79–87.
Soladoye OP, Lopez Campos O, Aalhus JL, Gariepy C, Shand P, Juarez M. Accuracy of dual energy X-ray absorptiometry (DXA) in assessing carcass composition from different pig populations. Meat Sci. 2016;121:310–6.
Salas CER, England J, Cerrate S, Noon CN. Determination of chicken body composition measured by dual energy X-ray absorptiometry. Int J Poult Sci. 2012;11:462–8.
Lopez-Campos O, Roberts JC, Larsen IL, et al. Rapid and non-destructive determination of lean fat and bone content in beef using dual energy X-ray absorptiometry. Meat Sci. 2018;146:140–6.
Mawby DI, Bartges JW, d’Avignon A, Laflamme DP, Moyers TD, Cottrell T. Comparison of various methods for estimating body fat in dogs. J Am Anim Hosp Assoc. 2004;40:109–14.
German AJ, Holden SL, Bissot T, Morris PJ, Biourge V. Use of starting condition score to estimate changes in body weight and composition during weight loss in obese dogs. Res Vet Sci. 2009;87:249–54.
Lauten SD, Cox NR, Baker GH, Painter DJ, Morrison NE, Baker HJ. Body composition of growing and adult cats as measured by use of dual energy X-ray absorptiometry. Comp Med. 2000;50:175–83.
Acknowledgements
Brazilian Association of Bone Assessment and Osteometabolism (ABRASSO; Brazilian Society of Bone Metabolism), and Milena Braga-Basaria, MD (Voxmed Medical Communications) for critical review and suggestions of improvements to the manuscript.
Funding
Brazilian Association of Bone Assessment and Osteometabolism (ABRASSO; Brazilian Society of Bone Metabolism).
Author information
Authors and Affiliations
Contributions
B-HA, VLS, ML-C, HPA, MU, DSD, RMRP, RVM-M, ML de O, LMC de M, M do P, GC de S, CZP, ROSS, MTT, LCG de C, SMBA, LA, DEK, CMM do P, MCG contributed with each of the items. MCG and CMM do P contributed with a critical analysis. SSM, M de MP were the concievers of the manuscript and made a final revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maeda, S.S., Albergaria, BH., Szejnfeld, V.L. et al. Official Position of the Brazilian Association of Bone Assessment and Metabolism (ABRASSO) on the evaluation of body composition by densitometry—part II (clinical aspects): interpretation, reporting, and special situations. Adv Rheumatol 62, 11 (2022). https://doi.org/10.1186/s42358-022-00240-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-022-00240-9