Abstract
Pediatric applications of body composition analysis (BCA) have become of increased interest to pediatricians and other specialists. With the increasing prevalence of morbid obesity and with an increased awareness of anorexia nervosa, pediatric specialists are utilizing BCA data to help identify, treat, and prevent these conditions. Dual-energy X-ray absorptiometry (DXA) can be used to determine the fat mass (FM) and lean tissue mass (LTM), as well as bone mineral content (BMC). Among the readily available BCA techniques, DXA is the most widely used and it has the additional benefit of precisely quantifying regional FM and LTM. This review evaluates the strengths and limitations of DXA as a pediatric BCA method and considers the utilization of DXA to identify trends and variations in FM and LTM measurements in obese and anorexic children.


Similar content being viewed by others
References
Dehghan M, Akhtar-Danesh N, Merchant AT (2005) Childhood obesity, prevalence and prevention. Nutr J 4:24
Franks PW, Hanson RL, Knowler WC et al (2007) Childhood predictors of young-onset type 2 diabetes. Diabetes 56:2964–2972
Gunnell DJ, Frankell SJ, Nanchahal K et al (1998) Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 6:1111–1118
Reaven G, Abbasi F, McLaughlin T (2004) Obesity, insulin resistance, and cardiovascular disease. Recent Prog Horm Res 59:207–223
Xu Z, Jiaqing A, Yuchuan L et al (2008) A case-control study of obstructive sleep apnea-hypopnea syndrome in obese and nonobese Chinese children. Chest 133:684–689
Wells J (2003) Body composition in childhood: effects of normal growth and disease. Proc Nutr Soc 62:521–528
Wells JCK, Fewtrell MS (2008) Is body composition important for pediatricians? Arch Dis Child 93:168–172
Fox CS, Massaro JM, Hoffman U et al (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116(1):39–48
Blake GM, Naeem M, Boutros M (2006) Comparison of effective dose to children and adults from dual x-ray absorptiometry examinations. Bone 38:935–942
Mazess RB, Barden HS, Bisek JP et al (1990) Dual-energy x-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am J Clin Nutr 51:1106–1112
Margulies L, Horlick H, Thornton JC et al (2005) Reproducibility of pediatric whole body bone and body composition measures by dual-energy x-ray absorptiometry using the GE Lunar Prodigy. J Clin Densitom 8:298–304
Njeh CF, Samat SB, Nightingale A et al (1997) Radiation dose and in vitro precision in paediatric bone mineral density measurement using dual x-ray absorptiometry. Br J Radiol 70:719–727
Ellis KJ, Shypailo RJ, Pratt JA et al (1994) Accuracy of dual-energy x-ray absorptiometry for body-composition measurements in children. Am J Clin Nutr 60:660–665
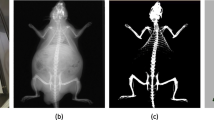
Black A, Tilmont EM, Baer DJ et al (2001) Accuracy and precision of dual-energy x-ray absorptiometry for body composition measurements in rhesus monkeys. J Med Primatol 30:94–99
Svendsen OL, Harbo J, Hassanger C et al (1993) Accuracy of measurement of body composition by dual-energy x-ray absorptiometry in vivo. Am J Nutr 57:605–608
Laskey MA, Flaxman ME, Barber RW et al (1991) Comparative performance in vitro and in vivo of Lunar DPX and Hologic QDR-1000 dual energy X-ray absorptiometers. Br J Radiol 64:1023–1029
Tothill P, Avenell A, Love J et al (1994) Comparisons between Hologic, Lunar and Norland dual-energy x-ray absorptiometers and other techniques used for whole-body soft tissue measurements. Eur J Clin Nutr 48:781–794
Moore FD, Boyden CM (1963) Body cell mass and limits of hydration of the fat-free body: their relation to estimated skeletal weight. Ann N Y Acad Sci 110:62–71
Laskey MA (1996) Dual-energy x-ray absorptiometry and body composition. Nutrition 12:45–51
Laskey MA, Lyttle KD, Flaxman ME et al (1992) The influence of tissue depth and composition on the performance of the Lunar dual-energy x-ray absorptiometer whole-body scanning mode. Eur J Clin Nutr 46:39–45
Jebb SA, Goldberg GR, Elia M (1993) DXA measurements of fat and bone mineral density in relation to depth and adiposity. Basic Life Sci 60:115–119
Tothill P, Avenell A, Reid DM (1994) Precision and accuracy of measurements of whole-body bone mineral: comparisons between Hologic, Lunar and Norland dual-energy x-ray absorptiometers. Br J Radiol 67:1210–1217
Pritchard JE, Nowson BJ, Strauss JS et al (1993) Evaluation of dual energy x-ray absorptiometry as a method of measurement of body fat. Eur J Clin Nutr 47:216–228
Van Loan MD, Keim NL, Berg K et al (1995) Evaluation of body composition by dual energy x-ray absorptiometry and two different software packages. Med Sci Sports Exerc 27:587–591
Treuth MS, Butte NF, Wong WW et al (2001) Body composition in prepubertal girls: comparison of six methods. Int J Obes Relat Metab Disord 25:1352–1359
Campanozzi A, Dabbas M, Ruiz JC et al (2007) Evaluation of lean body mass in obese children. Eur J Pediatr 167:533–540
Sopher AB, Thornton JC, Wang J et al (2004) Measurement of percentage of body fat in 411 children and adolescents: a comparison of dual-energy x-ray absorptiometry with a four-compartment model. Pediatrics 113:1285–1290
Fields DA, Goran MI (2000) Body composition techniques and the four-compartment model in children. J Appl Physiol 89:613–620
Elberg J, McDuffie JR, Sebring NG et al (2004) Comparison of methods to assess change in children's body composition. Am J Clin Nutr 80:64–69
Wang Y, Lobstein T (2006) Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 1:11–25
Wells JC, Coward WA, Cole TJ et al (2002) The contribution of fat and fat-free tissue to body mass index in contemporary children and the reference child. Int J Obes Relat Metab Disord 26:1323–1328
Koo WW, Walters JC, Hockman EM (2000) Body composition in human infants at birth and postnatally. J Nutr 130:2188–2194
Chumlea WC, Siervogel RM, Roche AF et al (1983) Increments across age in body composition for children 10 to 18 years of age. Hum Biol 55:845–852
Shaw NJ, Crabtree NJ, Kibirige MS et al (2007) Ethnic and gender differences in body fat in British schoolchildren as measured by DXA. Arch Dis Child 92:872–875
van der Sluis IM, de Ridder MAJ, Boot AM et al (2002) Reference data for bone density and body composition measured with dual energy x-ray absorptiometry in white children and young adults. Arch Dis Child 87:341–347
Frisch RE (1987) Body fat, menarche, fitness and fertility. Hum Reprod 2:521–533
Frisch RE, Revelle R (1970) Height and weight at menarche and a hypothesis of critical body weights and adolescent events. Science 169:397–399
Sherar LB, Baxter-Jones AD, Mirwald RL (2007) The relationship between body composition and onset of menarche. Ann Hum Biol 34:673–677
Qing HE, Horlick M, Thornton J et al (2002) Sex and race differences in fat distribution among Asian, Africa-American, and Caucasian prepubertal Children. J Clin Endocrinol Metab 87:2164–2170
Pludowski P, Matusik H, Olszaniecka M et al (2005) Reference values for the indicators of skeletal and muscular status of healthy Polish children. J Clin Densitom 8:164–177
Yanovski JA, Yanovski SZ, Filmer KM et al (1996) Differences in body composition of black and white girls. Am J Clin Nutr 64:833–839
Ellis KJ (1997) Body composition of a young, multiethnic, male population. Am J Clin Nutr 66:1323–1331
Boot AM, Bouquey J, de Ridder MA et al (1997) Determinants of body composition measured by dual-energy x-ray absorptiometry in Dutch children and adolescents. Am J Clin Nutr 66:232–238
Bonnick SL, Johnstom CC Jr, Kleerekoper M et al (2001) Importance of precision in bone density measurements. Clin Densitom 4:105–110
Wells JC (2001) A critique of the expression of paediatric body composition data. Arch Dis Child 85:67–72
Wells JC (2000) A Hattori chart analysis of body mass index in infants and children. Int J Obes Relat Metab Disord 24:325–329
Lohman TG, Going SB (2006) Body composition assessment for development of an international growth standard for preadolescent and adolescent children. Food Nutr Bull 27(4 Suppl Growth Standard):S314–S325
Ford ES, Mokdad AH (2008) Epidemiology of obesity in the Western Hemisphere. J Clin Endocrinol Metab 93(11 Suppl 1):S1–S8
Shear CL, Freedman SD, Burke GL et al (1988) Secular trends of obesity in early life: the Bogalusa heart study. Am J Public Health 78:75–77
Campaigne BN, Morisson JA, Schumann BC et al (1994) Indexes of obesity and comparisons with previous national survey data in 9 and 10 year old black and white girls: the National Heart, Lung, and Blood Institute growth and health study. J Pediatr 124:675–680
Troiano RP, Flegal KM, Kuczmarski RJ et al (1995) Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolescent Med 149:1085–1091
Yip SK, Scanlon K, Trowbridge F (1993) Trends and patterns in height and weight status of low-income U.S. children. Crit Rev Food Sci Nutr 33:409–421
Webber LS, Srinivasn SA, Berenson GS (1995) Obesity studies in Bogalusa. Am J Med Sci 310:S53–S61
Allison DB, Fontaine KR, Manson JE et al (1999) Annual deaths attributable to obesity in the United States. JAMA 282:1530–1538
Colditz GA (1999) Economic costs of obesity and inactivity. Med Sci Sports Exerc 31:S663–S667
Drash A (1973) Relationship between diabetes mellitus and obesity in the child. Metabolism 22:337–344
Rhodes SK, Shimoda KC, Waid LR et al (1995) Neurocognitive deficits in morbidly obese children with obstructive sleep apnea. J Pediatr 127:741–744
Hill A, Silver E (1995) Fat, friendless, and unhealthy: 9-year old children's perception of body shape stereotypes. Int J Obes Relat Metab Disord 19:423–430
Fontaine KR, Barofsky I (2001) Obesity and health-related quality of life. Obes Rev 2:173–182
Wabitsch M (2000) Overweight and obesity in European children: definition and diagnostic procedures, risk factors, and consequences for later health outcome. Eur J Pediatr 159(Suppl 1):S8–S13
Croft JB, Parker FS, Berenson GS (1994) Recruitment and participation of children in a long term study of cardiovascular disease: the Bogalusa heart study, 1973–1982. Am J Epidemiol 120:436–448
Walton C, Lees B, Crook D et al (1995) Body fat distribution, rather than overall adiposity, influences serum lipids and lipoproteins in healthy men independently of age. Am J Med 99:459–464
Despres JP (1990) Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 10:497–511
Goulding A, Cannan R, Williams SM et al (1998) Bone mineral density in girls with forearm fractures. J Bone Miner Res 13:143–148
Goulding A, Jones IE, Taylor RW et al (2001) Bone mineral density and body composition in boys with distal forearm fractures: a dual-energy x-ray absorptiometry study. Pediatrics 139:509–515
Han TS, Tijhuis M, Lean ME et al (1998) Quality of life in relation to overweight and body fat distribution. Am J Pub Health 88:1814–1820
Doll HA, Petersen SE, Stewart-Brown SL (2000) Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res 8:160–170
Larsson U, Karlsson J, Sullivan M (2002) Impact of overweight and obesity on health-related quality of life – a Swedish population study. Int J Obes Relat Metab Disord 26:417–424
Barofsky I, Cheskin LJ (1997) Pain in the obese: impact on health-related quality-of-life. Ann Behav Med 19:408–410
Hulens M, Vansant G, Lysens R et al (2001) Exercise capacity in lean versus obese women. Scand J Med Sci Sports 11:305–309
Lafortuna CL, Vangeli V, Sartorio A (2002) Lower limb alactic anaerobic power output assessed with different techniques in morbid obesity. J Endocrinol Invest 25:134–141
Voors AW, Harsha D, Webber LS et al (1981) Obesity and external sexual maturation – the Bogalusa heart study. Prev Med 10:50–61
Slyper AH (1998) Childhood obesity, adipose distribution, and the pediatric practitioner. Pediatrics 102:e4
Pi-Sunyer FX (1999) Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc 31:S602–S608
National Task Force on the Prevention and Treatment of Obesity (2000) Overweight, obesity and health risk. Arch Intern Med 160:898–904
Lafortuna CL, Maffiuletti NA, Agosti F et al (2005) Gender variations of body composition, muscle strength and power output in morbid obesity. Int J Obes (Lond) 29:833–841
Bray GA (1992) Pathophysiology of obesity. Am J Clin Nutr 55:488s–494s
Dencker M, Thorsson O, Linden C et al (2007) BMI and objectively measured body fat and body fat distribution in prepubertal children. Clin Physiol Funct Imaging 27:12–16
Taylor RW, Jones IE, Williams SM et al (2002) Body fat percentages measured by dual-energy x-ray absorptiometry corresponding to recently recommended body mass index cutoffs for overweight and obesity in children and adolescents aged 3–18 y. Am J Clin Nutr 76:1416–1421
Ellis KJ, Abrams SA, Wong WW (1997) Body composition of a young, multiethnic female population. Am J Clin Nutr 65:724–731
National Institutes of Health (1998) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults – The Evidence Report. Obes Res 6(Suppl 2):51S–209S
Coupaye M, Bouillot J, Poitou C et al (2007) Is lean body mass decreased after obesity treatment by adjustable gastric banding? Obes Surg 17:427–433
Dixon JB, Strauss BJ, Laurie C et al (2007) Changes in body composition with weight loss: obese subjects randomized to surgical and medical programs. Obesity (Silver Spring) 15:1187–1198
Strauss BJ, Marks SJ, Growcott JP et al (2003) Body composition changes following laparoscopic gastric banding for morbid obesity. Acta Diabetol 40(Suppl 1):S266–S269
Olbers T, Bjorkman S, Lindroos AK et al (2006) Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg 244:715–722
First MB (ed) (1994) Diagnostic and statistical manual of mental disorders, 4th edn. The American Psychiatric Association, Washington DC
Lucas AR, Beard MC, O'Fallon WM et al (1991) 50-year trends in the incidence of anorexia nervosa in Rochester, Minn.: a population-based study. Am J Psychiatry 148:917–922
Signorini A, De Filippo E, Panico S et al (2007) Long-term mortality in anorexia nervosa: a report after an 8-year follow-up and a review of the most recent literature. Eur J Clin Nutr 61:119–122
Probst M, Goris M, Vandereycken W et al (1996) Body composition in female anorexia nervosa patients. Br J Nutr 76:639–647
Trocki O, Shepard RW (2000) Change in body mass index does not predict change in body composition in adolescent girls with anorexia nervosa. J Am Diet Assoc 100:457–460
Kerruish KP, O’Connor J, Humphries IR et al (2002) Body composition in adolescents with anorexia nervosa. Am J Clin Nutr 75:31–37
Mayer L, Walsh BT, Pierson RN et al (2005) Body fat redistribution after weight gain in women with anorexia nervosa. Am J Clin Nutr 81:1286–1291
Kooh SW, Noriega E, Leslie K et al (1996) Bone mass and soft tissue composition in adolescents with anorexia nervosa. Bone 19:181–188
Krahn DD (1993) Changes in resting energy expenditure and body composition in anorexia nervosa patients during refeeding. J Am Diet Assoc 93:434–438
Nicholls D, Wells CJ, Singhal A et al (2002) Body composition in early onset eating disorders. Eur J Clin Nutr 56:865–867
Polito A, Cuzzolaro M, Raguzzini A et al (1998) Body composition changes in anorexia nervosa. Eur J Clin Nutr 52:655–662
Tothill P, James Hannan W (2004) Dual-energy X-ray absorptiometry measurements of fat and lean masses in subjects with eating disorders. Int J Obes Relat Metab Disord 28:912–919
Shypailo RJ, Butte NF, Ellis KJ (2008) DXA: can it be used as a criterion reference for body fat measurements in children? Obesity 16:457–462
Trocki O, Theodoros MT, Shepherd RW (1998) Lack of sensitivity of weight targets compared to body cell mass for determining recovery from malnutrition in adolescents with anorexia nervosa. Int J Eat Disord 23:169–175
Iketani T, Kirike N, Nagata T et al (1999) Altered body fat distribution after recovery of weight in patients with anorexia nervosa. Int J Eat Disord 26:275–282
Pike KM (1998) Long-term course of anorexia nervosa: response, relapse, remission, and recovery. Clin Psychol Rev 18:447–475
Sala A, Webber CE, Morrison J et al (2007) Whole-body bone mineral content, lean body mass, and fat mass measured by dual-energy x-ray absorptiometry in a population of normal Canadian children and adolescents. Can Assoc Radiol J 58:46–52
Rigo J, Nyambugabo K, Picaud JC et al (1998) Reference values of body composition obtained by dual energy x-ray absorptiometry in preterm and term neonates. J Pediatr Gastroenterol Nutr 27:184–190
Nelson DA, Barondess DA (1997) Whole body bone, fat and lean mass in children: comparison of three ethnic groups. Am J Phys Anthropol 103:157–162
Ogle GD, Allen JR, Humphries IRJ et al (1995) Body-composition assessment by dual-energy x-ray absorptiometry in subjects aged 4–26 y. Am J Clin Nutr 61:746–753
National Center for Health Statistics (2009) National health and nutrition examination survey. Centers for Disease Control and Prevention, Hyattsville, MD. http://www.cdc.gov/nchs/about/major/nhanes/dxx/dxa.htm. Accessed 30 Mar 2009
Wells JC, Fewtrell MS (2006) Measuring body composition. Arch Dis Child 91:612–617
Ellis KJ (2001) Selected body composition methods can be used in field studies. J Nutr 131:1589S–1595S
Goldfield GS, Cloutier P, Mallory R et al (2006) Validity of foot-foot bioelectrical impedance analysis in overweight and obese children and parents. J Sports Med Phys Fitness 46:447–453
Fields DA, Goran MI (2000) Body composition techniques and the four-compartment model in children. J Appl Physiol 89:613–620
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
BCA techniques have been grouped as either predictive or compartment models [107]. Predictive models make a direct measurement, such as subcutaneous skinfold anthropometry or the body’s bioelectrical impedance to a small electrical current, and then predict body composition using reference data, algorithms and underlying assumptions. Compartment models measure one or more components of body composition, such as total body water (a surrogate for fat-free mass) and then predict the other body components using separate reference data, algorithms and underlying assumptions.
SFT measurements are easy to perform on children but lack precision and have been found to be a poor predictor of FM by many investigators [107, 108]. This is especially true in obese individuals and in the setting of subcutaneous edema. Accuracy can be improved with better mathematical prediction models. The sheer number of such models (more than 100 published) indicates the complexity of the relationships between body fat and SFT measurements and suggests the need for appropriately matching patient parameters to those of the control group upon which the modeling was based.
The flow of an electric current through the body is proportional to its water content. With the assumption that the body is a cylinder and using appropriate calibration models, total body water can be predicted by BIA. Additional assumptions regarding the water content of lean and fat tissues allow BIA to estimate LTM and FM [107, 108]. The technique is easy to perform and requires little operator training or patient cooperation. However, it has significant limitations that include poor accuracy, imprecision caused by variations in tissue hydration and numerous calibration models based on normal data that might not be appropriate for an individual patient [109].
Compartment models tend to be more complicated and invasive than predictive techniques because up to four body compartments (fat, lean, bone mineral and water) are determined separately. Total body mineral content can be measured with DXA. With the assumption that there is no water in fat and that there is a constant level of hydration and density of lean tissues, techniques that measure total body water can be used to estimate LTM and FM given a patient’s weight. DXA is a two-compartment technique initially developed to use differential absorption of X-rays to distinguish bone mineral from overlying soft tissues. Using the above-mentioned assumptions allows the DXA absorption data to estimate fat and fat-free tissue mass. Three- and four-compartment models require a measurement of total body water [107, 110]. Following the injection of a tracer agent of known quantity and biodistribution, the measured concentration of the agent in a body fluid, such as urine or saliva, can be used to determine total body water. Given the patient's weight and measurement of the patient’s body volume, body density can be determined using assumptions about tissue hydration, body fat and lean tissue. Body volume can be measured using displacement techniques such as underwater weighing or air plethysmography. An underlying assumption of compartment models is that the composition of lean tissue is constant for a given patient age and gender. Tissue composition is fairly constant in healthy individuals but varies with age and particularly with pubertal status and gender. This assumption might not hold for patients with altered hydration status or more severe metabolic derangements.
Alternative imaging techniques for BCA include CT and MRI. CT can provide accurate assessment of subcutaneous and visceral fat within the area imaged but is expensive, requires fairly high radiation doses and does not provide total body assessment. MRI provides highly detailed images of fat and lean tissue, from which fat volume can be derived. To be converted to mass values, assumptions regarding levels of hydration and density of lean and fat tissues are made. Because of this, MRI-derived BCA data are not directly comparable to data derived from the above-mentioned techniques [108]. The technique is relatively expensive and many children require sedation.
All of these techniques have advantages and disadvantages [108]. SFT is easy to perform but is imprecise and particularly inaccurate in obese individuals and provides no direct information regarding LTM. BIA lacks sufficient accuracy for individual patients, though it may be suitable to population studies and its results are particularly sensitive to hydration status and changes in body weight. Dilution and displacement techniques can yield accurate results and, when combined with DXA determination of total body mineral, yield a four-compartment technique that is considered the gold standard against which other techniques are measured. They are not suitable for field work, however. Traditional methods for determination of body volume are not feasible for most children. DXA is highly reproducible, easy to perform and uses minimum radiation. Its accuracy can be improved with further refinement of the algorithms used for its body composition modeling. It is not able to differentiate muscle from other lean tissues, such as liver, spleen and other organ tissue, nor can it distinguish adipose tissue from bone marrow fat or fat within solid viscera. Regional FM analysis with DXA does not give a reliable assessment of visceral fat. However, it is widely available and has the largest body of research and clinical data associated with it. It is highly reproducible and accurate and can provide complementary body composition data for patients who require DXA for assessment of BMD and bone mineral content.
Rights and permissions
About this article
Cite this article
Helba, M., Binkovitz, L.A. Pediatric body composition analysis with dual-energy X-ray absorptiometry. Pediatr Radiol 39, 647–656 (2009). https://doi.org/10.1007/s00247-009-1247-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-009-1247-0