Abstract
Background
Healthcare-associated infections involving Gram-negative bacteria (GNB) with difficult-to-treat resistance (DTR) phenotype are associated with impaired patient-centered outcomes and poses daily therapeutic challenges in most of intensive care units worldwide. Over the recent years, four innovative β-lactam/β-lactamase inhibitor (BL/BLI) combinations (ceftolozane–tazobactam, ceftazidime–avibactam, imipenem–relebactam and meropenem–vaborbactam) and a new siderophore cephalosporin (cefiderocol) have been approved for the treatment of certain DTR-GNB infections. The literature addressing their microbiological spectrum, pharmacokinetics, clinical efficacy and safety was exhaustively audited by our group to support the recent guidelines of the French Intensive Care Society on their utilization in critically ill patients. This narrative review summarizes the available evidence and unanswered questions on these issues.
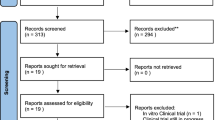
Methods
A systematic search for English-language publications in PUBMED and the Cochrane Library database from inception to November 15, 2022.
Results
These drugs have demonstrated relevant clinical success rates and a reduced renal risk in most of severe infections for whom polymyxin- and/or aminoglycoside-based regimen were historically used as last-resort strategies—namely, ceftazidime–avibactam for infections due to Klebsiella pneumoniae carbapenemase (KPC)- or OXA-48-like-producing Enterobacterales, meropenem–vaborbactam for KPC-producing Enterobacterales, ceftazidime–avibactam/aztreonam combination or cefiderocol for metallo-β-lactamase (MBL)-producing Enterobacterales, and ceftolozane–tazobactam, ceftazidime–avibactam and imipenem–relebactam for non-MBL-producing DTR Pseudomonas aeruginosa. However, limited clinical evidence exists in critically ill patients. Extended-infusion scheme (except for imipenem–relebactam) may be indicated for DTR-GNB with high minimal inhibitory concentrations and/or in case of augmented renal clearance. The potential benefit of combining these agents with other antimicrobials remains under-investigated, notably for the most severe presentations. Other important knowledge gaps include pharmacokinetic information in particular situations (e.g., pneumonia, other deep-seated infections, and renal replacement therapy), the hazard of treatment-emergent resistance and possible preventive measures, the safety of high-dose regimen, the potential usefulness of rapid molecular diagnostic tools to rationalize their empirical utilization, and optimal treatment durations. Comparative clinical, ecological, and medico-economic data are needed for infections in whom two or more of these agents exhibit in vitro activity against the causative pathogen.
Conclusions
New BL/BLI combinations and cefiderocol represent long-awaited options for improving the management of DTR-GNB infections. Several research axes must be explored to better define the positioning and appropriate administration scheme of these drugs in critically ill patients.
Similar content being viewed by others
Introduction
Carbapenems stand as the main option for the treatment of severe infections due to Gram-negative bacteria (GNB) exhibiting resistance to broad-spectrum penicillins and cephalosporins [1,2,3]. Yet, the dissemination of carbapenem-resistant GNB, either at an endemic state or during outbreak phenomenon, now poses daily therapeutic challenges in most of intensive care units (ICU) worldwide [4,5,6,7,8]. Infections involving carbapenem-resistant GNB are associated with a substantial rise in fatality rates, length of hospital stay and costs of care when compared to those caused by carbapenem-susceptible isolates [9,10,11,12,13,14]. These impaired outcomes may result from a higher likelihood of inadequate empirical therapy, toxicity attributable to historical last-resort agents (e.g., polymyxin-related acute kidney injury), and the frailty of individuals in whom such conditions predominantly occur [15]. In addition, most of carbapenem-resistant GNB are resistant to other antimicrobial classes, further complicating the management of infected patients—hence, co-resistance to carbapenems, all other first-line β-lactams and fluoroquinolones is consensually defined as difficult-to-treat resistance (DTR) [1,2,3].
Over the recent years, four innovative β-lactam/β-lactamase inhibitor (BL/BLI) combinations (namely, ceftolozane–tazobactam, ceftazidime–avibactam, imipenem–relebactam and meropenem–vaborbactam) and a new siderophore cephalosporin (cefiderocol) have been introduced and approved for the treatment of certain DTR-GNB infections. The literature addressing their microbiological spectrum, pharmacokinetics, clinical efficacy and safety in critically ill patients has been exhaustively audited by our group to support the guidelines of the French Intensive Care Society, elaborated during a consensus conference held in Paris on November 30, 2022 and published in this issue of Annals of Intensive Care. In this narrative review, we summarize the available evidence and knowledge gaps on these questions, with a focus on DTR-GNB infections.
Methods
We systematically searched PubMed and the Cochrane Library database from inception to November 15, 2022. The search terms are listed in Additional file 1 of this article. We manually searched the reference lists of the included studies and systematic reviews to select additional relevant articles. Studies published in languages other than English were not retained.
Current epidemiology of DTR-GNB in critically ill patients
Critically ill patients present a marked predisposition for DTR-GNB infection as a combined result of massive exposure to broad-spectrum antimicrobials damaging the resident microbiotas and their inherent colonization resistance functions, and repeated opportunities for cross-transmission ensuing from invasive procedures and prolonged hospitalization [16, 17]. Enterobacterales (primarily Klebsiella pneumoniae and Escherichia coli), Pseudomonas aeruginosa, Acinetobacter baumannii and Stenotrophomonas maltophilia account for virtually all healthcare-associated DTR-GNB infections in the ICU.
Carbapenem resistance in Enterobacterales depends almost exclusively on the acquisition and expression of plasmid-borne carbapenemases belonging to the A (mostly Klebsiella pneumoniae carbapenemase [KPC]), B (metallo-β-lactamases [MBL], especially New-Delhi MBL [NDM]) or D (oxacillinases, mainly OXA-48-like carbapenemases) classes of the Ambler’s scheme (Table 1) [18, 19]. The prevalence of carbapenemase-producing Enterobacterales (CPE) is increasing globally, with a marked trend for MBL-producing isolates—this pandemic shows large geographical disparities, with a North/South gradient and higher prevalence in low- and middle-income countries (Table 2) [8, 20,21,22,23]. Endemic states have been reached in Italy, Greece and the United States for KPC producers, in the India/Pakistan region for NDM producers, and in the India/Pakistan and Mediterranean regions for OXA-48 producers; however, sporadic outbreaks are now regularly reported in other areas, including Latin America, Oceania, Africa and Northern Europe [24]. In 2017, in the 37 European countries contributing to the eCDC surveillance program, the prevalence of carbapenem resistance among invasive isolates of K. pneumoniae and E. coli ranged from 0 to 65% and from 0% to 1.6%, respectively; 16 (43%) countries reported regional or interregional spread of CPE while four countries (Greece, Italy, Turkey and Malta) declared an endemic situation [25]. In France, CPE infections remain infrequent, with less than 1000 cases reported annually [26], in line with a low prevalence of colonization—indeed, in a recent study including 2396 hospitalized patients, the rate of intestinal carriage of CPE was still 1.2% [27].
In Pseudomonas aeruginosa, carbapenem resistance rests on both plasmid-borne carbapenemases (mostly MBL such as VIM, IMP, NDM or SPM) and chromosomal mutations leading to over-expression of efflux pump systems or impermeability through porin D2 alterations [18]. The overall prevalence of carbapenem resistance in invasive isolates of P. aeruginosa fluctuates between 10 and 20% in most geographic areas [8, 20, 22, 23], with a variable proportion of DTR phenotypes that may locally increase owing to outbreaks related to certain high-risk clones (Table 2) [28, 29]. Next, as for Enterobacterales, carbapenem resistance in Acinetobacter baumannii is predominantly driven by plasmid-borne carbapenemases, with OXA-23 as the leading type [19]. Rates of carbapenem resistance in invasive isolates of A. baumannii have reached critical levels in the Mediterranean area, South-East Asia and, to a lesser extent, Southern Europe (Table 2). In a recent global study including 350 critically ill patients with hospital-acquired bloodstream infection due to A. baumannii, 296 (84.6%) were infected by CR isolates [23]. Lastly, Stenotrophomonas maltophilia expresses a chromosomally encoded MBL that confers intrinsic carbapenem resistance to the species [18]. Infections due to this pathogen mostly occur in critically ill and/or immunocompromised hosts, especially in those with prior exposure to carbapenems or other broad-spectrum β-lactams [30]. Resistance to both cotrimoxazole and fluoroquinolones may pragmatically correspond to a DTR phenotype though there is no consensual definition for this species.
Bacterial spectrum of cefiderocol and new BL/BLI combinations
In vitro activity against carbapenemase-producing Enterobacterales
Avibactam is a potent inhibitor of serine-β-lactamases (that is, Ambler’s classes A, C and D); therefore, ceftazidime–avibactam is active in vitro against 96–99% of KPC- and OXA-48-like-producing Enterobacterales (Table 1) [31,32,33,34,35]. Yet, resistance to ceftazidime–avibactam may emerge following mutations in KPC-encoding genes (mainly blaKPC-2 and blaKPC-3) or genes encoding outer membrane proteins (OmpK35-37), especially when associated with a high number of blaKPC-2 copies [36,37,38,39]. MBL-producing Enterobacterales are resistant to ceftazidime–avibactam since avibactam has no inhibitory effect on these enzymes. However, the combination of ceftazidime–avibactam plus aztreonam is active against around 80% of MBL-producing Enterobacterales [40], aztreonam being not hydrolyzed by MBL and avibactam inhibiting the other β-lactamases commonly co-produced by such isolates (e.g., hyperproduced AmpC cephalosporinases, extended-spectrum β-lactamases [ESBL], or class A carbapenemases such as KPC, all including aztreonam in their hydrolysis spectrum) [41, 42].
Relebactam and vaborbactam inhibit class A β-lactamases, without effect on MBL or OXA carbapenemases [43]. Imipenem–relebactam and meropenem–vaborbactam are active in vitro against 88–95% and 95–99% of KPC-producing Enterobacterales, respectively [43,44,45]. Certain KPC variants and ESBL co-expression have been linked with a rise in minimal inhibitory concentrations (MIC) of imipenem–relebactam while over-expression of blaKPC may increase those of meropenem–vaborbactam; in addition, porin mutations (OmpK35, OmpK 36) can reduce the activity of both drugs [46,47,48]. Importantly, these combinations remain occasionally active against isolates producing KPC-2 or KPC-3 variants with reduced susceptibility to the inhibitory effect of avibactam [45, 49].
Cefiderocol is a poor substrate for all β-lactamase classes and shows in vitro activity against 84–81%, 88–93%, 79–81% and 41–51% of KPC-, OXA-48-, VIM- and NDM-producing Enterobacterales, ESBL co-expression and porin mutations being associated with a reduced activity of the drug [50, 51]. Also, the inoculum effect—that is, an elevation of MIC values for high bacterial concentrations [52]—appears more pronounced with cefiderocol than with other new agents though the clinical significance of this finding is not yet elucidated [53].
The MIC cut-off values of novel BL/BLI combinations and cefiderocol for Enterobacterales, as defined by the European Committee on Antimicrobial Susceptibility Testing (EUCAST), are exposed in Table 3. Importantly, ceftolozane is hydrolyzed by all described carbapenemases, none of which being inhibited by tazobactam; therefore, ceftolozane–tazobactam exerts no activity against CPE [54, 55].
In vitro activity against carbapenem-resistant non-fermenting GNB
Ceftolozane circumvents two major mechanisms of β-lactam resistance in P. aeruginosa—namely, efflux and AmpC-mediated hydrolysis [56]. This fifth-generation cephalosporin, independently of its association with tazobactam, is active in vitro against 75–90% of non-carbapenemase-producing carbapenem-resistant P. aeruginosa isolates and, more globally, against 40–80% of DTR isolates within this species [54, 57,58,59,60,61]. Resistance to ceftolozane–tazobactam in P. aeruginosa depends on either certain plasmid-borne β-lactamases (e.g., MBL, OXA-14, OXA-19, OXA-35, GES-9, or PER-1) or extreme over-expression of chromosomal AmpC [62]. A. baumannii and S. maltophilia are intrinsically resistant to ceftolozane.
Both avibactam and relebactam inhibit chromosomal AmpC in P. aeruginosa. Ceftazidime–avibactam and imipenem–relebactam are active against 65%-85% of DTR isolates of P. aeruginosa [57,58,59, 63, 64]. Avibactam does not restore ceftazidime activity in MBL-producing isolates or in those with over-expressed efflux pump systems for which ceftazidime is a substrate. Relebactam may restore imipenem activity is isolates with mutated D2 porin and derepressed AmpC, likely due to the limited but significant hydrolysis of imipenem by this enzyme [65]. These two combinations lack activity against carbapenemase-producing isolates of A. baumannii and against S. maltophilia, this later species being intrinsically poorly susceptible to ceftazidime and resistant to imipenem [18]. Meropenem–vaborbactam is not active against meropenem-resistant isolates of P. aeruginosa or A. baumannii due to the lack of inhibitory effect of vaborbactam on mechanisms of meropenem resistance in these species (that is efflux, impermeability, or carbapenemase production).
Cefiderocol is active in vitro against 90% to 95% of carbapenem-resistant isolates of P. aeruginosa [66,67,68,69]. No MIC threshold of cefiderocol is currently defined by the EUCAST for A. baumannii and S. maltophilia; however, more than 90% of isolates within these species show MIC values below 2 mg/L (i.e., the cut-off value for Enterobacterales and P. aeruginosa) [69].
A key-point is that the multiplicity of potentially involved resistance mechanisms makes unpredictable the activity of new β-lactams in DTR P. aeruginosa. Indeed, a substantial proportion of isolates exhibiting resistance to one agent remains susceptible to others, which implies to perform susceptibility tests for all novel BL/BLI combinations and cefiderocol in isolates with such phenotypes [70]. Of note, gradient test strips are not accurate to measure cefiderocol MICs [71, 72], which should be determined using broth microdilution methods [73].
Interestingly, a combination of ceftazidime–avibactam and aztreonam may have high in vitro activity against cotrimoxazole- and fluoroquinolone-resistant isolates of S. maltophilia, a species that expresses a chromosomal AmpC cephalosporinase susceptible to the inhibitory effect of avibactam in addition to its chromosomal MBL [74, 75].
In vitro activity against other relevant pathogens responsible for infections in critically ill patients
ESBL are class A serine-β-lactamases that are susceptible to the inhibitory effect of both tazobactam and avibactam. Avibactam also inhibits AmpC cephalosporinases while tazobactam does not. Therefore, both ceftolozane–tazobactam and ceftazidime–avibactam are active against ESBL-producing Enterobacterales without AmpC co-expression but only the latter combination is active against isolates co-producing ESBL and derepressed ampC (e.g., Enterobacter spp) [76]. Imipenem–relebactam and meropenem–vaborbactam are highly active against ESBL-producing Enterobacterales due to the intrinsic activity of carbapenems on these pathogens [43, 77].
Gram-positive bacteria and most of cultivable anaerobes are intrinsically resistant to ceftolozane–tazobactam, ceftazidime–avibactam and cefiderocol [78,79,80]. The activity of imipenem–relebactam and meropenem–vaborbactam on these pathogens does not differ from the one of imipenem and meropenem, respectively.
Clinical efficacy of cefiderocol and new BL/BLI combinations in DTR-GNB infections
Data from randomized controlled trials
Most of randomized controlled trials (RCT) evaluating the clinical efficacy and safety of cefiderocol and novel BL/BLI combinations were not focused on DTR-GNB infections and used a carbapenem as comparator [81,82,83,84,85,86]. Only three RCTs addressed the input of these new agents in the specific context of DTR-GNB infections.
In the TANGO II trial [87], 47 patients with documented CPE infection (mostly KPC-producing K. pneumoniae) were treated for 7 to 14 days by either meropenem–vaborbactam or best available therapy (BAT), most often including an aminoglycoside and/or a polymyxin according to susceptibility test results. Rates of clinical success were 66% and 33% (difference, 32%; 95% confidence interval [CI], 3% to 61%) at end of therapy and 59% and 27% (difference, 33%; 95% CI, 5% to 61%) at test-of-cure (ToC) visit for meropenem–vaborbactam and BAT, respectively. Day-28 all-cause mortality rates were 16% and 33% (difference, 18%; 95% CI − 45% to 9%). A composite endpoint of clinical failure and nephrotoxicity occurred less frequently with meropenem–vaborbactam when compared to the BAT arm (31% versus 80%; 95% CI for difference, − 75% to − 23%). In this trial, the efficacy of meropenem–vaborbactam was not evaluated according to the baseline MIC of this combination for the causative pathogen. Only one patient in the BAT arm received ceftazidime–avibactam (single-drug regimen), excluding any comparison between the two BL/BLI combinations.
In the RESTORE-IMI 1 trial [88], 47 patients infected with DTR-GNB (mostly DTR P. aeruginosa susceptible to both imipenem–relebactam and colistin) were treated with imipenem–relebactam or an imipenem/colistin combination. The overall rates of clinical success at Day 28 were 71% and 40% in patients receiving imipenem–relebactam and controls, respectively (difference, 26%; 95% CI 1% to 51%) while those of Day-28 all-cause fatality were 10% and 30% (difference, − 17%; 95% CI − 46% to 7%). Drug-related adverse events—especially nephrotoxicity—were considerably more common in the imipenem/colistin arm. Of note, MICs of imipenem–relebactam ranged from 0.5 to 4 mg/L for P. aeruginosa isolates; however, whether this baseline MIC impacted the clinical response to the drug was not investigated.
In the CREDIBLE-CR trial [89], 152 patients with a documented DTR-GNB infection (A. baumannii, 46%; K. pneumoniae, 33%; P. aeruginosa, 19%; MIC90 of cefiderocol, 1, 4 and 2 mg/L, respectively) received either cefiderocol (single-drug therapy, 85%) or BAT (colistin-based, 67%; combination therapy, 45%) for 5 to 21 days. Overall rates of clinical success at ToC visit were similar in the two arms (53% versus 50%), including in patients with hospital-acquired pneumonia. Rates of microbiological eradication (31% versus 24%) and of relapse (3% versus 11%) were, respectively, higher and lower in the cefiderocol arm. However, the rate of all-cause fatality was numerically higher in the cefiderocol arm at Day 14 (19% versus 12%), Day 28 (25% versus 18%) and at follow-up termination (34% versus 18%). This finding, which could not be linked to any of baseline patient characteristics, was mostly attributable to an excess mortality in patients infected with A. baumannii (fatality rate, 49% versus 18% in the cefiderocol and BAT arms, respectively)—no difference was observed between the two arms for patients infected with P. aeruginosa or K. pneumoniae, except in those with A. baumannii co-infection. The baseline MIC value did not correlate with the likelihood of clinical or microbiological failure, which was observed even for isolates with MIC < 0.5 mg/L. Hetero-resistance has been evocated as an underlying mechanism for such observations, notably for A. baumannii [90]; nonetheless, whether this phenomenon correlates with the hazard of treatment failure is debated and necessitates further investigations. Following the publication of this trial, the Food and Drug Administration issued a warning statement that advocated for restricting the use of cefiderocol to patients in whom no other therapeutic option is available [91].
Data from observational and post hoc studies
Regarding CPE, several cohort studies reported clinical success rates above 65–70% with ceftazidime–avibactam for severe infections due to KPC- or OXA-48-like-producing Enterobacterales [92,93,94,95,96,97,98,99,100,101] and with meropenem–vaborbactam for severe infections due to KPC-producing Enterobacterales [102,103,104,105]. An ancillary study from the CREDIBLE-CR and ASPEK-NP RCT evaluated cefiderocol versus BAT for infections due to MBL-producing Enterobacterales and reported numerically higher rate of clinical success and lower rate of mortality with cefiderocol [106]. Another ancillary study from the same trials and including 10 patients infected with OXA-48-like-producing Enterobacterales reported clinical cure in 7 of them [107]. The clinical efficacy of cefiderocol in CPE infections has also been reported in numerous case-reports and small observational studies [108]. Relevant clinical success rates—similar to those observed with cefiderocol—have equally been observed with the combination of ceftazidime–avibactam and aztreonam for infections due to MBL-producing Enterobacterales [109,110,111]. No clinical study focused on the efficacy of imipenem–relebactam for infections due to KPC-producing Enterobacterales has been published so far.
To our knowledge, the efficacy of novel BL/BLI combinations in CPE infections has been directly compared in only one study. This work focused on infections due to KPC-producing Enterobacterales (72% of cases) and including roughly half of critically ill patients, ceftazidime–avibactam (n = 105) and meropenem–vaborbactam (n = 26) showed similar results in terms of clinical and microbiological successes, length of hospital stay, incidence of adverse events, and mortality [112].
Most of cohort studies centered on patients infected with non-MBL-producing DTR P. aeruginosa reported clinical success rates above 60% with ceftolozane–tazobactam [92, 113,114,115,116,117] and ceftazidime–avibactam [101, 118,119,120,121,122,123]. Observational data on the clinical efficacy of imipenem–relebactam are lacking for this patient population.
Lastly, a single-center study with propensity-score analyses using inverse probability of treatment weighting reported a lower mortality rate with cefiderocol versus colistin-based regimen in patients with DTR A. baumannii infection (except for those with ventilator-associated pneumonia), contrasting with the results of the CREDIBLE-CR trial [124]. In this work, microbiological failure was twice more frequent in the cefiderocol arm. Nephrotoxicity was more common in the colistin arm [124].
The cohort studies cited above were mostly retrospective and not devoted to critically ill patients. To date, real-life data on the efficacy of these new β-lactams in patients with life-threatening DTR-GNB infection (e.g., septic shock) are dramatically scarce.
Combination therapy—what clinical evidence?
Enhanced bacterial killing and a reduced risk of resistance emergence are usual arguments for the use of antimicrobial combinations in critically ill patients with GNB infection. Nevertheless, combining antibiotics may also raises concerns related to safety issues including toxicity, drug–drug interactions, and potential ecological impact. Hence, despite decades of extensive research in the field, the benefit-to-risk ratio of combination therapy in this population is still debated, with fragmentary evidence for improved survival only in the most severe presentations [125].
Two meta-analyses of observational studies and RCT found no survival benefit with ceftazidime–avibactam combined with one or more antimicrobials (i.e., fosfomycin, tigecycline, gentamicin, or meropenem) when compared to ceftazidime–avibactam alone for the treatment of DTR-GNB infections [126, 127]. Two large retrospective multicentre cohort studies including patients with infections due to KPC-producing K. pneumoniae and published after the above-mentioned meta-analyses yielded similar results [128, 129]; of note, one of them reported a trend toward improved survival with combination therapy in the subgroup of patients with hospital-acquired pneumonia [128]. Clinical evidence related to the potential benefit of combining ceftazidime–avibactam with colistin is limited to case-reports or small case-series, precluding any conclusion to be drawn [95, 130].
A meta-analysis of observational studies demonstrated a significant reduction in all-cause mortality when combining ceftolozane–tazobactam with other antimicrobials in patients with GNB infections—mostly DTR P. aeruginosa infections—yet without benefit in terms of clinical cure and microbiological eradication [131]. A subsequent multicentre study focused on DTR P. aeruginosa infections in critically ill patients did not confirm this survival benefit [117].
A multi-center retrospective study including 37 patients with severe KPC-producing K. pneumoniae infection reported a higher mortality rate with meropenem–vaborbactam combined with another antimicrobial (mostly colistin or fosfomycin) when compared to meropenem–vaborbactam alone; however, patients receiving combination therapy were older, had more comorbidities and presented with higher severity indexes, thereby inducing obvious bias in the interpretation of this result [102].
In a post hoc analysis of the CREDIBLE-CR trial, the proportions of patients with clinical cure and microbiological eradication at ToC visit did not differ between patients receiving cefiderocol as single-drug regimen or in combination; however, only 14 patients received combination therapy [89]. A single-center retrospective study including 16 patients with DTR A. baumannii infection showed similar results [132].
To our knowledge, no published data exist to appraise the potential benefit of combining imipenem–relebactam with other antimicrobials for DTR-GNB infections, especially those involving P. aeruginosa.
Overall, it remains unclear whether cefiderocol and novel BL/BLI combinations should be associated with antimicrobial agents from other classes to improve patient-centered outcomes in severe DTR-GNB infections, with most of available clinical data coming from retrospective cohort studies. Pending further evidence, combination therapies could be considered in certain situations at high risk for clinical or microbiological failure such as unachievable source control, high bacterial inoculum, or infections due to extensively drug-resistant strains with elevated MICs, as suggested in certain studies evaluating older antimicrobials in DTR-GNB infections [133, 134].
Clinical pharmacokinetics and optimization of dosing schemes
New drugs, old PK/PD concepts
The most efficient pharmacokinetic/pharmacodynamic (PK/PD) index to predict bacterial cell killing with β-lactams is the percentage of the dosing interval during which the concentration of unbound drug exceeds the MIC of the strain (%fT > MIC). A reasonable amount of evidence corroborates that fT ≥ MIC equal to 100% (i.e., minimal inter-dose concentration [Cmin]/MIC ≥ 1) and even fT ≥ 5xMIC equal to 100% (i.e., Cmin/MIC ≥ 5) should be targeted in patients receiving β-lactams for severe infections [135,136,137,138,139,140], higher Cmin/MIC ratio being linked with enhanced bacterial killing and reduced emergence of resistant mutants [135, 141,142,143]. Higher blood levels also correlate with improved tissue penetration and bioavailability of the drug at the infection site. As supported by Monte Carlo simulations [144, 145], extending the duration of β-lactam infusion increases drug exposure and allows higher Cmin targets to be reached, which could translate into improved patient outcome during severe infections [146, 147]. Available data suggest that these concepts apply for new β-lactams and plead for the routine use of 3-h infusion scheme for cefiderocol and meropenem–vaborbactam, and 4- to 6-h infusion scheme for ceftolozane–tazobactam and ceftazidime–avibactam (Fig. 1) [128, 144, 148,149,150,151]. The stability of the drug in syringes at room temperature must be considered when using extended or continuous infusion. Recent studies reported a stability of 4 to 8 h for meropenem (in dextrose 5% and normal saline, respectively), 12 h for vaborbactam, and 24 h for ceftazidime–avibactam, ceftolozane–tazobactam, cefiderocol and aztreonam (either in dextrose 5% or normal saline) [152, 153].
Administration scheme and dosing adjustments of new β-lactam/β-lactamase inhibitor combinations and cefiderocol in critically ill patients. See the text and Table 4 for references. CFL: cefiderocol; CFL: cefiderocol; C-TZ: ceftolozane–tazobactam; CAZ-AVI: ceftazidime–avibactam; MER-VAB: meropenem–vaborbactam; IMI-REL: imipenem–relebactam; CrCl: creatinine clearance; MIC: minimal inhibitory concentration; AKI: acute kidney injury; TDM: therapeutic drug monitoring; IHD: intermittent haemodialysis; CRRT: continuous renal replacement therapy; LD: loading dose
Dosing adjustment in particular situations
New BL/BLI combinations and cefiderocol share similar characteristics with older β-lactams, including high therapeutic indexes, heterogeneous inoculum effect, hydrophilicity, small molecular weights, almost exclusive renal clearance, low protein-binding (except for cefiderocol) implying effective elimination by renal replacement therapy (RRT), and variable tissue diffusion (Table 4) [53, 154]. Dosing adjustment may be required in specific clinical situations to ensure sufficient antibiotic concentration at the infectious site while avoiding toxic levels to be attained [155, 156].
First, augmented renal clearance (ARC), consensually defined as a creatinine clearance ≥ 130 mL/min/1.73m2, may reduce Cmin and overall drug exposure, thereby lowering the probability of PK/PD target attainment, especially for bacterial isolates with high MIC values. For instance, through continuous infusion of ceftolozane–tazobactam has been shown to ease PK/PD target attainment in most cases, 4-h extended infusion may be more effective for MIC values ≥ 4 mg/L combined with ARC [144]. Higher-dose regimen appear also needed in this situation (Fig. 1) [149, 151, 157]. Of note, cefiderocol is the only new β-lactam for which high-dose schemes were used in patients with ARC in pivotal randomized studies—further data are needed for new BL/BLI combinations in this population.
Next, while renal dysfunction exposes to β-lactam over-dosing, therapeutic failures have also been reported in this context, raising the question of inadequate PK/PD target attainment [158]. For novel agents as for older β-lactams, recommendations for dose adjustment in case of renal dysfunction are mostly based on data from patients with chronic kidney disease. Because of increased volume of distribution in critically ill patients, possible resolution of acute renal dysfunction within the first following days [155, 159], high therapeutic index and a limited risk of neurotoxicity with short exposure to high doses, a loading dose is recommended regardless of ClCr and dose adjustment should be applied only after the first 24 to 48 h of therapy [150, 154, 160, 161]. Evidence for dosing adjustment of cefiderocol and new BI/BLI combination in critically ill patients receiving RRT is currently scarce; however, data related to older β-lactams suggest that dosing scheme should be adapted to the overall effluent flow rate during continuous RRT while systematic reinjection at the end of the session may ensure the achievement of PK/PD objectives during intermittent hemodialysis [162,163,164,165].
Of note, hepatic dysfunction does not induce any clinically relevant variation in β-lactam PK; therefore, no dosing adjustment is required in patients with liver failure.
Data are also lacking to appraise the pharmacokinetic impact of obesity for the new drugs addressed here. Generally, the hydrophilic feature of β-lactams explains the weak variation of their volume of distribution in case of overweight [166, 167]. Whether using adjusted body weight may be beneficial in obese patients remains to be confirmed [166]. Higher dosing could be discussed in cases of morbid obesity and high MIC values [168].
Case-reports and small case-series suggest that extracorporeal membrane oxygenation (ECMO) exerts no major effect on the pharmacokinetics of ceftolozane–tazobactam and cefiderocol, with standard dosing enabling the attainment of usual targets [169,170,171,172]. No clinical information is available for other new β-lactams in patients under ECMO.
Through this approach does not appear justified in all critically ill patients [173, 174], therapeutic drug monitoring combined with MIC measurement (to avoid undue dose escalation) could be proposed in those at marked risk for PK/PD impairments (e.g., causative pathogen with high MIC value, ARC, RRT, or low tissue penetration rate). Close collaboration between microbiologist, pharmacist, infectious disease specialist and intensivist is warranted in these situations.
Safety issues
Non-ecological adverse events
No apparent over-risk of drug-related adverse events was noticed with cefiderocol or new BL/BLI combinations in RCTs comparing these agents with meropenem, imipenem plus colistin, or BAT [81, 83, 86,87,88,89]. Importantly, the hazard of acute kidney injury was higher with BAT in nearly all studies using this regimen as comparator, a finding mostly attributable to colistin-induced nephrotoxicity [87,88,89, 124]. Encephalopathy may conceivably occur with these drugs as with older β-lactams though it remains to be explored [175, 176]. A recent large-scale pharmacovigilance analysis suggested an over-reporting of agranulocytosis/pancytopenia and acute pancreatitis with ceftolozane–tazobactam and ceftazidime–avibactam, respectively—these observations require confirmation in clinical cohorts [175].
Impact on the intestinal microbiota
Evidence related to the impact of ceftazidime–avibactam on the gut microbiota is limited to a single study including 12 healthy volunteers receiving standard dosing (2 gr/0.5 gr q8h) for 7 days [177]. This work, based on conventional cultures and not on modern metagenomics approaches, showed a transient decrease in Enterobacterales counts, an increase in the count of Enterococcus spp (without return to baseline 14 days after treatment completion in most of volunteers), a sustained drop in the counts of cultivable resident anaerobes and, strikingly, the acquisition of a toxinogenic strain of Clostridioides difficile in 5 subjects [177]. This apparent link between ceftazidime–avibactam exposure and C. difficile acquisition was not confirmed in clinical studies—indeed, in a multicentre cohort including 203 patients receiving ceftazidime–avibactam, only 3 cases (1.5%) of C. difficile infection were documented [123]. To date, no data exist regarding the impact of ceftolozane–tazobactam, imipenem–relebactam, meropenem–vaborbactam or cefiderocol on the gut microbiota. Clinical studies addressing this issue appear extremely complex to set up since almost all patients requiring these drugs present with multiple risk factors for intestinal dysbiosis, including critical illness and prior exposure to other broad-spectrum antimicrobials [178].
Emergence of resistance under therapy
Treatment-emergent resistance to ceftazidime–avibactam in KPC-producing Enterobacterales mostly results from mutations of the blaKPC-2 or blaKPC-3 genes and may be involved in up to 30% of clinical failure or relapse following exposure to this drug [179,180,181,182,183,184]. Acquired resistance to meropenem–vaborbactam and imipenem–relebactam in CPE appears mostly driven by impermeability ensuing from mutation-induced porin loss—this phenomenon appears rare in patients treated with meropenem–vaborbactam (< 5%) while its incidence has not been precisely described in those receiving imipenem–relebactam [105, 112, 179]. In P. aeruginosa, the emergence of resistance to ceftolozane–tazobactam rests on mutation-induced over-expression of the chromosomal blaAmpC gene: this mechanism might be involved in up to 50% of patients with microbiological failure at end of therapy, especially in case of intermittent infusion (when compared to extended infusion) and defective source control [185]. However, in a post hoc analysis of the ASPECT-NP RCT including 59 patients receiving ceftolozane–tazobactam for nosocomial pneumonia due to P. aeruginosa, only 3 (5%) acquired a ceftolozane–tazobactam-resistant isolate under therapy, all with a new strain (no resistant mutant selection) [186]. Treatment-emergent resistance to imipenem–relebactam in patients infected with CR P. aeruginosa has been recently linked with mutations in the MexAB-OprM and/or MexEF-OprN efflux operons [187]—the clinical frequency of this phenomenon is unknown. Lastly, in the CREDIBLE-CR trial, a fourfold or higher increase in baseline cefiderocol MIC values of causative pathogens was observed in 15% of microbiologically evaluable patients receiving this agent—this increase led to values exceeding the EUCAST susceptibility threshold in one third of cases [89].
Empirical use of cefiderocol and new BL/BLI combinations in critically ill patients
Pending dedicated studies on this issue, several key aspects of antimicrobial stewardship should be taken in account when considering the potential utilization of cefiderocol and new BL/BLI combinations for empirical therapy in patients with suspected DTR-GNB infection. First, the choice of empirical antimicrobials must be a “winning bet” in case of severe infection. Indeed, while delayed appropriate therapy is strongly associated with impaired outcomes in patients with septic shock [188, 189], unnecessary exposure to broad-spectrum antimicrobials may lead to deleterious ecological side-effects (namely, alteration of the host microbiota, acquisition of multidrug-resistant bacteria, and Clostridioides difficile infection) and toxic adverse events [190, 191]. Conversely, evidence exists that a restrictive strategy for empirical initiation of broad-spectrum antimicrobials in hemodynamically stable patients with suspected ICU-acquired infection has no negative impact on hospital mortality [192]. Second, the emergence of bacterial resistance under therapy has been described for virtually all antimicrobial agents, including cefiderocol and novel BL/BLI combinations [89, 112, 179, 193, 194]. Hence, a liberal utilization of these new drugs might compromise their activity on CR-GNB. Third, not all ICU patients are at-risk for infection due to DTR-GNB. Identifying such patients is a challenge that can be approached using known risk factors such as recent exposure to carbapenems and other broad-spectrum agents, invasive healthcare procedures, and, most of all, local epidemiology—that is, endemicity or on-going outbreaks, especially in case of defective infection prevention measures. The colonization status is also pivotal since carriage is a prerequisite for subsequent infection; however, through negative sequential surveillance cultures have a high negative predictive value, less than 50% of critically ill individuals colonized with carbapenem-resistant GNB will experience a healthcare-associated infection due to these pathogens during their ICU stay [195,196,197]. In addition, full antimicrobial susceptibility test results—or, at least, information on the determinants of carbapenem resistance—should be available for clinicians to assist the choice of the most appropriate drug since these agents are not identical with respect to their spectrum of activity and mechanisms of action (Table 1). Multiplex PCR assays enabling species and carbapenemase identification directly from clinical samples in short turn-around time could be useful, but their input warrants further investigation [198]. Of note, these tools are ineffective to detect carbapenem resistance resulting from chromosomal mutations—e.g., in P. aeruginosa [199].
Published evidence on the empirical use of new β-lactams in critically ill patients is currently lacking. These agents might be administered empirically in patients at high-risk for DTR-GNB (that is, known carriage or local endemicity with high colonization pressure) and presenting with life-threatening healthcare-associated infection (e.g., septic shock). Every probabilistic prescription should be reevaluated early to avoid unnecessary exposure to these drugs, with prompt de-escalation to a narrower-spectrum regimen whenever possible.
Should ceftolozane–tazobactam and ceftazidime–avibactam be prescribed as carbapenem-sparing agents in patients infected with ESBL- or AmpC-produding Enterobacterales?
Published RCT have demonstrated the non-inferiority of ceftolozane–tazobactam versus meropenem in terms of clinical cure in patients with complicated intra-abdominal infections (in combination with metronidazole) or nosocomial pneumonia [82, 83]. In this latest trial, ceftolozane–tazobactam was non-inferior to meropenem in patients with pneumonia due to ESBLE or ceftazidime-resistant P. aeruginosa, for clinical cure as for Day-28 all-cause mortality [83]. Moreover, a multi-center study including 153 patients with severe ESBLE infections reported an 84%-overall success rate with ceftolozane–tazobactam [200]. Yet, important considerations argue against the use of ceftolozane–tazobactam as a carbapenem-sparing option in patients with ESBLE infections, including the willingness to preserve its efficacy on DTR P. aeruginosa [193], the hazard of co-selection of ceftazidime–avibactam resistance in P. aeruginosa isolates with treatment-emergent resistance to ceftolozane–tazobactam [201], and the lack of data regarding a potential benefit of ceftolozane–tazobactam versus carbapenems regarding antimicrobial-induced intestinal dysbiosis. Likewise, the results of several RCT [81, 202,203,204,205,206,207] and a meta-analysis [208] support the non-inferiority of ceftazidime–avibactam versus carbapenems on mortality and/or clinical cure endpoints in complicated urinary tract infections, complicated intra-abdominal infections (in combination with metronidazole) and nosocomial pneumonia, even when focusing on ESBL- or AmpC-producing Enterobacterales [209]. Nevertheless, similar arguments than for ceftolozane–tazobactam argue against the liberal use of ceftazidime–avibactam in these common indications, notably the risk of reduced activity on KPC-producing Enterobacterales resulting from mutant selection [182, 210] or the lack of real-world data demonstrating a more limited impact on commensal microbiotas when compared to carbapenems. As others [1], we believe that the use of these BL/BLI combinations should be restricted to clinical situations in whom no first-line safe options are available—that is, infections due to DTR P. aeruginosa plus, for ceftazidime–avibactam only, those due to KPC- or OXA-48-producing Enterobacterales.
Summary of evidence and research agenda
New BL/BLI combinations and cefiderocol represent long-awaited options for improving the management of DTR-GNB infections. These drugs have demonstrated relevant clinical success rates and a reduced renal risk in most of situations for whom polymyxin- and/or aminoglycoside-based regimen were historically used as last-resort strategies—that is, ceftazidime–avibactam for infections due to KPC- or OXA-48-like-producing Enterobacterales, meropenem–vaborbactam for KPC-producing Enterobacterales, ceftazidime–avibactam/aztreonam combination or cefiderocol for MBL-producing Enterobacterales, and ceftolozane–tazobactam, ceftazidime–avibactam and imipenem–relebactam for non-MBL-producing DTR P. aeruginosa. To preserve their efficacy, these drugs should not be used to treat infections due to multidrug-resistant but carbapenem-susceptible GNB (e.g., ESBL-producing Enterobacterales).
Notwithstanding these promising results, limited evidence exists on the use of new β-lactams in critically ill patients with DTR-GNB infection. Several important knowledge gaps warrant urgent investigation in this population, including PK/PD information in particular situations (e.g., pneumonia or other deep-seated infections, RRT and ARC), the benefit of combination therapy for the most severe presentations or DTR-GNB with high MIC values for these new agents, the input of TDM, a precise appraisal of the hazard of treatment-emergent resistance and possible preventive measures, safety analyses (especially for high-dose regimen), the potential usefulness of multiplex PCR assay and other rapid diagnostic tools to rationalize their empirical utilization in ICUs facing endemicity or on-going outbreaks, and optimal treatment durations. Comparative clinical, ecological and medico-economic data are equally needed for situations in whom two or more of these agents exhibit in vitro activity against the causative pathogen. Further studies addressing the aforementioned issues will help better defining the positioning and appropriate administration scheme of these new β-lactams in critically ill patients.
Availability of data and materials
Not applicable.
Abbreviations
- ARC:
-
Augmented renal clearance
- BAT:
-
Best available therapy
- BL/BLI:
-
β-Lactam/β-lactamase inhibitor combination
- CI:
-
Confidence interval
- Cmin :
-
Minimal inter-dose concentration
- CPE:
-
Carbapenemase-producing Enterobacterales
- DTR:
-
Difficult-to-treat resistance
- eCDC:
-
European Centre for Disease Control and Prevention
- ESBL:
-
Extended-spectrum β-lactamase
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- GES:
-
Guyana Extended-spectrum β-lactamase
- GNB:
-
Gram-negative bacteria
- ICU:
-
Intensive care unit
- IMP:
-
Imipenemase
- KPC:
-
Klebsiella pneumoniae Carbapenemase
- MBL:
-
Metallo-β-lactamase
- MIC:
-
Minimal inhibitory concentration
- NDM:
-
New-Delhi metallo-β-lactamase
- OXA:
-
Oxacillinase
- PCR:
-
Polymerase chain reaction
- PD:
-
Pharmacodynamic
- PK:
-
Pharmacokinetic
- RCT:
-
Randomized controlled trial
- RRT:
-
Renal replacement therapy
- TDM:
-
Therapeutic drug monitoring
- ToC:
-
Test-of-cure
- VIM:
-
Verona integron-encoded metallo-β-lactamase
References
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase-producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2021;72(7):e169–83.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of AmpC β-lactamase-producing Enterobacterales, carbapenem-resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia infections. Clin Infect Dis. 2022;74(12):2089–114.
Paul M, Carrara E, Retamar P, Tängdén T, Bitterman R, Bonomo RA, et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin Microbiol Infect. 2022;28(4):521–47.
Rosenthal VD, Bat-Erdene I, Gupta D, Belkebir S, Rajhans P, Zand F, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2012–2017: Device-associated module. Am J Infect Control. 2020;48(4):423–32.
Hu F, Guo Y, Yang Y, Zheng Y, Wu S, Jiang X, et al. Resistance reported from China antimicrobial surveillance network (CHINET) in 2018. Eur J Clin Microbiol Infect Dis. 2019;38(12):2275–81.
Karlowsky JA, Lob SH, Kazmierczak KM, Young K, Motyl MR, Sahm DF. In-vitro activity of imipenem/relebactam and key β-lactam agents against Gram-negative bacilli isolated from lower respiratory tract infection samples of intensive care unit patients - SMART Surveillance United States 2015–2017. Int J Antimicrob Agents. 2020;55(1): 105841.
Centers for Disease Control and Prevention (U.S.). Antibiotic resistance threats in the United States, 2019 [Internet]. Centers for Disease Control and Prevention (U.S.); 2019. https://stacks.cdc.gov/view/cdc/82532. Accessed 26 Mar 2023.
Antimicrobial resistance in the EU/EEA (EARS-Net) - Annual epidemiological report for 2021. European Centre for Disease Prevention and Control. Available at www.ecdc.europa.eu. Accessed 15 Jan 2023.
Lemos EV, de la Hoz FP, Einarson TR, McGhan WF, Quevedo E, Castañeda C, et al. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect. 2014;20(5):416–23.
Kohler PP, Volling C, Green K, Uleryk EM, Shah PS, McGeer A. Carbapenem resistance, initial antibiotic therapy, and mortality in Klebsiella pneumoniae bacteremia: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2017;38(11):1319–28.
Martin A, Fahrbach K, Zhao Q, Lodise T. Association between carbapenem resistance and mortality among adult, hospitalized patients with serious infections due to Enterobacteriaceae: results of a systematic literature review and meta-analysis. Open Forum Infect Dis. 2018;5(7): ofy150.
Righi E, Peri AM, Harris PNA, Wailan AM, Liborio M, Lane SW, et al. Global prevalence of carbapenem resistance in neutropenic patients and association with mortality and carbapenem use: systematic review and meta-analysis. J Antimicrob Chemother. 2017;72(3):668–77.
Liu Q, Li X, Li W, Du X, He JQ, Tao C, et al. Influence of carbapenem resistance on mortality of patients with Pseudomonas aeruginosa infection: a meta-analysis. Sci Rep. 2015;25(5):11715.
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–55.
Barbier F, Lisboa T, Nseir S. Understanding why resistant bacteria are associated with higher mortality in ICU patients. Intensive Care Med. 2016;42(12):2066–9.
Palacios-Baena ZR, Giannella M, Manissero D, Rodríguez-Baño J, Viale P, Lopes S, et al. Risk factors for carbapenem-resistant Gram-negative bacterial infections: a systematic review. Clin Microbiol Infect. 2021;27(2):228–35.
Woerther PL, Lepeule R, Burdet C, Decousser JW, Ruppé É, Barbier F. Carbapenems and alternative β-lactams for the treatment of infections due to extended-spectrum β-lactamase-producing Enterobacteriaceae: what impact on intestinal colonisation resistance? Int J Antimicrob Agents. 2018;52(6):762–70.
Ruppé É, Woerther PL, Barbier F. Mechanisms of antimicrobial resistance in Gram-negative bacilli. Ann Intensive Care. 2015;5(1):61.
Nordmann P, Poirel L. Epidemiology and diagnostics of carbapenem resistance in Gram-negative bacteria. Clin Infect Dis. 2019;69(Suppl 7):S521–8.
Hu F, Yuan L, Yang Y, Xu Y, Huang Y, Hu Y, et al. A multicenter investigation of 2,773 cases of bloodstream infections based on China antimicrobial surveillance network (CHINET). Front Cell Infect Microbiol. 2022;12:1075185.
Weiner-Lastinger LM, Abner S, Edwards JR, Kallen AJ, Karlsson M, Magill SS, et al. Antimicrobial-resistant pathogens associated with adult healthcare-associated infections: summary of data reported to the National Healthcare Safety Network, 2015–2017. Infect Control Hosp Epidemiol. 2020;41(1):1–18.
Sader HS, Streit JM, Carvalhaes CG, Huband MD, Shortridge D, Mendes RE, et al. Frequency of occurrence and antimicrobial susceptibility of bacteria isolated from respiratory samples of patients hospitalized with pneumonia in Western Europe, Eastern Europe and the USA: results from the SENTRY Antimicrobial Surveillance Program (2016-19). JAC Antimicrob Resist. 2021;3(3): dlab117.
Tabah A, Buetti N, Staiquly Q, Ruckly S, Akova M, Aslan AT, et al. Epidemiology and outcomes of hospital-acquired bloodstream infections in intensive care unit patients: the EUROBACT-2 international cohort study. Intensive Care Med. 2023;49(2):178–90.
Bonomo RA, Burd EM, Conly J, Limbago BM, Poirel L, Segre JA, et al. Carbapenemase-producing organisms: a global scourge. Clin Infect Dis. 2018;66(8):1290–7.
European Centre for Disease Prevention and Control. Carbapenem-resistant Enterobacteriaceae : second update, 26 September 2019. www.ecdc.europa.eu. Accessed 15 Jan 2023.
Jousset A, Emeraud C, Bonnin RA, Naas T, Dortet L. Caractéristiques et évolution des souches d’entérobactéries productrices de carbapénémases (EPC) isolées en France, 2012–2020. Bull Epidémiol Hebd. 18–19:351–8.
Grohs P, Vilfaillot A, Zahar JR, Barbut F, Frange P, Casetta A, et al. Faecal carriage of multidrug-resistant bacteria and associated risk factors: results from a point prevalence study. J Antimicrob Chemother. 2022;77(10):2667–78.
Torrens G, van der Schalk TE, Cortes-Lara S, Timbermont L, Del Barrio-Tofiño E, Xavier BB, et al. Susceptibility profiles and resistance genomics of Pseudomonas aeruginosa isolates from European ICUs participating in the ASPIRE-ICU trial. J Antimicrob Chemother. 2022;77(7):1862–72.
Pelegrin AC, Saharman YR, Griffon A, Palmieri M, Mirande C, Karuniawati A, et al. High-risk international clones of carbapenem-nonsusceptible Pseudomonas aeruginosa endemic to Indonesian intensive care units: impact of a multifaceted infection control intervention analyzed at the genomic level. MBio. 2019;10(6):e02384–e2419.
Ibn Saied W, Merceron S, Schwebel C, Le Monnier A, Oziel J, Garrouste-Orgeas M, et al. Ventilator-associated pneumonia due to Stenotrophomonas maltophilia: risk factors and outcome. J Infect. 2020;80(3):279–85.
de Jonge BLM, Karlowsky JA, Kazmierczak KM, Biedenbach DJ, Sahm DF, Nichols WW. In vitro susceptibility to ceftazidime-avibactam of carbapenem-nonsusceptible Enterobacteriaceae isolates collected during the INFORM global surveillance study (2012 to 2014). Antimicrob Agents Chemother. 2016;60(5):3163–9.
Tamma PD, Bergman Y, Jacobs EB, Lee JH, Lewis S, Cosgrove SE, et al. Comparing the activity of novel antibiotic agents against carbapenem-resistant Enterobacterales clinical isolates. Infect Control Hosp Epidemiol. 2022;13:1–6.
Kazmierczak KM, de Jonge BLM, Stone GG, Sahm DF. In vitro activity of ceftazidime/avibactam against isolates of Enterobacteriaceae collected in European countries: INFORM global surveillance 2012–15. J Antimicrob Chemother. 2018;73(10):2782–8.
Kazmierczak KM, Biedenbach DJ, Hackel M, Rabine S, de Jonge BLM, Bouchillon SK, et al. Global dissemination of blaKPC into bacterial species beyond Klebsiella pneumoniae and in vitro susceptibility to ceftazidime-avibactam and aztreonam-avibactam. Antimicrob Agents Chemother. 2016;60(8):4490–500.
Castanheira M, Doyle TB, Collingsworth TD, Sader HS, Mendes RE. Increasing frequency of OXA-48-producing Enterobacterales worldwide and activity of ceftazidime/avibactam, meropenem/vaborbactam and comparators against these isolates. J Antimicrob Chemother. 2021;76(12):3125–34.
Gaibani P, Re MC, Campoli C, Viale PL, Ambretti S. Bloodstream infection caused by KPC-producing Klebsiella pneumoniae resistant to ceftazidime/avibactam: epidemiology and genomic characterization. Clin Microbiol Infect. 2020;26(4):516.e1–516.e4.
Coppi M, Di Pilato V, Monaco F, Giani T, Conaldi PG, Rossolini GM. Ceftazidime-avibactam resistance associated with increased blaKPC-3 gene copy number mediated by pKpQIL plasmid derivatives in sequence type 258 Klebsiella pneumoniae. Antimicrob Agents Chemother. 2020;64(4):e01816–e1819.
Haidar G, Clancy CJ, Chen L, Samanta P, Shields RK, Kreiswirth BN, et al. Identifying spectra of activity and therapeutic niches for ceftazidime-avibactam and imipenem-relebactam against carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2017;61(9):e00642–e717.
Mueller L, Masseron A, Prod’Hom G, Galperine T, Greub G, Poirel L, et al. Phenotypic, biochemical and genetic analysis of KPC-41, a KPC-3 variant conferring resistance to ceftazidime-avibactam and exhibiting reduced carbapenemase activity. Antimicrob Agents Chemother. 2019;63(12): e01111.
Mauri C, Maraolo AE, Di Bella S, Luzzaro F, Principe L. The revival of aztreonam in combination with avibactam against metallo-β-lactamase-producing Gram-negatives: a systematic review of in vitro studies and clinical cases. Antibiot Basel Switz. 2021;10(8):1012.
Davido B, Fellous L, Lawrence C, Maxime V, Rottman M, Dinh A. Ceftazidime-avibactam and aztreonam, an interesting strategy to overcome β-lactam resistance conferred by metallo-β-lactamases in Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017;61(9):e01008–e1017.
Biagi M, Wu T, Lee M, Patel S, Butler D, Wenzler E. Searching for the optimal treatment for metallo- and serine-β-lactamase producing Enterobacteriaceae: aztreonam in combination with ceftazidime-avibactam or meropenem-vaborbactam. Antimicrob Agents Chemother. 2019;63(12): e01426.
Tselepis L, Langley GW, Aboklaish AF, Widlake E, Jackson DE, Walsh TR, et al. In vitro efficacy of imipenem-relebactam and cefepime-AAI101 against a global collection of ESBL-positive and carbapenemase-producing Enterobacteriaceae. Int J Antimicrob Agents. 2020;56(1): 105925.
Shortridge D, Carvalhaes C, Deshpande L, Castanheira M. Activity of meropenem/vaborbactam and comparators against Gram-negative isolates from Eastern and Western European patients hospitalized with pneumonia including ventilator-associated pneumonia (2014–19). J Antimicrob Chemother. 2021;76(10):2600–5.
Pfaller MA, Huband MD, Mendes RE, Flamm RK, Castanheira M. In vitro activity of meropenem/vaborbactam and characterisation of carbapenem resistance mechanisms among carbapenem-resistant Enterobacteriaceae from the 2015 meropenem/vaborbactam surveillance programme. Int J Antimicrob Agents. 2018;52(2):144–50.
Gomez-Simmonds A, Stump S, Giddins MJ, Annavajhala MK, Uhlemann AC. Clonal background, resistance gene profile, and porin gene mutations modulate in vitro susceptibility to imipenem-relebactam in diverse Enterobacteriaceae. Antimicrob Agents Chemother. 2018;62(8):e00573–e618.
Balabanian G, Rose M, Manning N, Landman D, Quale J. Effect of porins and blaKPC expression on activity of imipenem with relebactam in Klebsiella pneumoniae: can antibiotic combinations overcome resistance? Microb Drug Resist. 2018;24(7):877–81.
Wilson WR, Kline EG, Jones CE, Morder KT, Mettus RT, Doi Y, et al. Effects of KPC variant and porin genotype on the in vitro activity of meropenem-vaborbactam against carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2019;63(3):e02048–e2118.
Tsivkovski R, Lomovskaya O. Potency of vaborbactam is less affected than that of avibactam in strains producing KPC-2 mutations that confer resistance to ceftazidime-avibactam. Antimicrob Agents Chemother. 2020;64(4):e01936–e2019.
Longshaw C, Manissero D, Tsuji M, Echols R, Yamano Y. In vitro activity of the siderophore cephalosporin, cefiderocol, against molecularly characterized, carbapenem-non-susceptible Gram-negative bacteria from Europe. JAC Antimicrob Resist. 2020;2(3): dlaa060.
Mushtaq S, Sadouki Z, Vickers A, Livermore DM, Woodford N. In vitro activity of cefiderocol, a siderophore cephalosporin, against multidrug-resistant Gram-negative bacteria. Antimicrob Agents Chemother. 2020;64(12):e01582–e1620.
Lenhard JR, Bulman ZP. Inoculum effect of β-lactam antibiotics. J Antimicrob Chemother. 2019;74(10):2825–43.
Danjean M, Hobson CA, Gits-Muselli M, Courroux C, Monjault A, Bonacorsi S, et al. Evaluation of the inoculum effect of new antibiotics against carbapenem-resistant enterobacterales. Clin Microbiol Infect. 2022;28(11):1503.e1-1503.e3.
Castanheira M, Duncan LR, Mendes RE, Sader HS, Shortridge D. Activity of ceftolozane-tazobactam against Pseudomonas aeruginosa and Enterobacteriaceae isolates collected from respiratory tract specimens of hospitalized patients in the United States during 2013 to 2015. Antimicrob Agents Chemother. 2018;62(3):e02125–e2217.
van Duin D, Bonomo RA. Ceftazidime/avibactam and ceftolozane/tazobactam: second-generation β-lactam/β-lactamase inhibitor combinations. Clin Infect Dis. 2016;63(2):234–41.
Livermore DM, Mushtaq S, Meunier D, Hopkins KL, Hill R, Adkin R, et al. Activity of ceftolozane/tazobactam against surveillance and ‘problem’ Enterobacteriaceae, Pseudomonas aeruginosa and non-fermenters from the British Isles. J Antimicrob Chemother. 2017;72(8):2278–89.
Grupper M, Sutherland C, Nicolau DP. Multicenter evaluation of ceftazidime-avibactam and ceftolozane-tazobactam inhibitory activity against meropenem-nonsusceptible Pseudomonas aeruginosa from blood, respiratory tract, and wounds. Antimicrob Agents Chemother. 2017;61(10):e00875–e917.
Gill CM, Aktaþ E, Alfouzan W, Bourassa L, Brink A, Burnham CAD, et al. The ERACE-PA global surveillance program: ceftolozane/tazobactam and ceftazidime/avibactam in vitro activity against a global collection of carbapenem-resistant Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis. 2021;40(12):2533–41.
Del Barrio-Tofiño E, Zamorano L, Cortes-Lara S, López-Causapé C, Sánchez-Diener I, Cabot G, et al. Spanish nationwide survey on Pseudomonas aeruginosa antimicrobial resistance mechanisms and epidemiology. J Antimicrob Chemother. 2019;74(7):1825–35.
Pfaller MA, Bassetti M, Duncan LR, Castanheira M. Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing urinary tract and intraabdominal infections in Europe: report from an antimicrobial surveillance programme (2012–15). J Antimicrob Chemother. 2017;72(5):1386–95.
Pfaller MA, Shortridge D, Sader HS, Castanheira M, Flamm RK. Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing healthcare-associated infections in the Asia-Pacific region (minus China, Australia and New Zealand): report from an Antimicrobial Surveillance Programme (2013–2015). Int J Antimicrob Agents. 2018;51(2):181–9.
Fournier D, Carrière R, Bour M, Grisot E, Triponney P, Muller C, et al. Mechanisms of resistance to ceftolozane/tazobactam in Pseudomonas aeruginosa: results of the GERPA multicenter study. Antimicrob Agents Chemother. 2021;65(2):e01117–e1120.
Sader HS, Castanheira M, Shortridge D, Mendes RE, Flamm RK. Antimicrobial activity of ceftazidime-avibactam tested against multidrug-resistant Enterobacteriaceae and Pseudomonas aeruginosa isolates from U.S. medical centers, 2013 to 2016. Antimicrob Agents Chemother. 2017;61(11):e01045–e1117.
Hernández-García M, García-Castillo M, Melo-Cristino J, Pinto MF, Gonçalves E, Alves V, et al. In vitro activity of imipenem/relebactam against Pseudomonas aeruginosa isolates recovered from ICU patients in Spain and Portugal (SUPERIOR and STEP studies). J Antimicrob Chemother. 2022;77(11):3163–72.
Horner C, Mushtaq S, Livermore DM, BSAC Resistance Surveillance Standing Committee. Potentiation of imipenem by relebactam for Pseudomonas aeruginosa from bacteraemia and respiratory infections. J Antimicrob Chemother. 2019;74(7):1940–4.
Hackel MA, Tsuji M, Yamano Y, Echols R, Karlowsky JA, Sahm DF. In vitro activity of the siderophore cephalosporin, cefiderocol, against a recent collection of clinically relevant Gram-negative bacilli from North America and Europe, including carbapenem-nonsusceptible isolates (SIDERO-WT-2014 Study). Antimicrob Agents Chemother. 2017;61(9):e00093–e117.
Ito A, Kohira N, Bouchillon SK, West J, Rittenhouse S, Sader HS, et al. In vitro antimicrobial activity of S-649266, a catechol-substituted siderophore cephalosporin, when tested against non-fermenting Gram-negative bacteria. J Antimicrob Chemother. 2016;71(3):670–7.
Jacobs MR, Abdelhamed AM, Good CE, Rhoads DD, Hujer KM, Hujer AM, et al. ARGONAUT-I: activity of cefiderocol (S-649266), a siderophore cephalosporin, against Gram-negative bacteria, including carbapenem-resistant nonfermenters and Enterobacteriaceae with defined extended-spectrum β-lactamases and carbapenemases. Antimicrob Agents Chemother. 2019;63(1):e01801–e1818.
Candel FJ, Santerre Henriksen A, Longshaw C, Yamano Y, Oliver A. In vitro activity of the novel siderophore cephalosporin, cefiderocol, in Gram-negative pathogens in Europe by site of infection. Clin Microbiol Infect. 2022;28(3):447.e1–447.e6.
Sader HS, Mendes RE, Arends SJR, Carvalhaes CG, Shortridge D, Castanheira M. Comparative activity of newer β-lactam/β-lactamase inhibitor combinations against Pseudomonas aeruginosa isolates from US medical centres (2020–2021). Int J Antimicrob Agents. 2023;61(4): 106744.
Bonnin RA, Emeraud C, Jousset AB, Naas T, Dortet L. Comparison of disk diffusion, MIC test strip and broth microdilution methods for cefiderocol susceptibility testing on carbapenem-resistant enterobacterales. Clin Microbiol Infect. 2022;28(8):1156.e1–1156.e5.
Devoos L, Biguenet A, Rousselot J, Bour M, Plésiat P, Fournier D, et al. Performance of discs, sensititre EUMDROXF microplates and MTS gradient strips for the determination of the susceptibility of multidrug-resistant Pseudomonas aeruginosa to cefiderocol. Clin Microbiol Infect. 2023;29(5):652.e1–652.e8.
European Committee on Antimicrobial Susceptibility Testing. Clinical breakpoints (available at www.eucast.org/clinical_breakpoints. Accessed 23 May 2023.
Emeraud C, Escaut L, Boucly A, Fortineau N, Bonnin RA, Naas T, et al. Aztreonam plus clavulanate, tazobactam, or avibactam for treatment of infections caused by metallo-β-lactamase-producing Gram-negative bacteria. Antimicrob Agents Chemother. 2019;63(5):e00010–19.
Crémet L, Joffraud L, Eschapasse E, Bihouée T, Tissot A, Gibaud S, et al. In vitro comparison of aztreonam/amoxicillin-clavulanate versus aztreonam/ceftazidime-avibactam on ceftazidime-avibactam resistant Stenotrophomonas maltophilia. Microb Drug Resist. 2022;28(8):877–81.
Castanheira M, Doyle TB, Mendes RE, Sader HS. Comparative activities of ceftazidime-avibactam and ceftolozane-tazobactam against Enterobacteriaceae isolates producing extended-spectrum β-lactamases from U.S. hospitals. Antimicrob Agents Chemother. 2019;63(7):e00160–e219.
Bianco G, Boattini M, Comini S, Iannaccone M, Casale R, Allizond V, et al. Activity of ceftolozane-tazobactam, ceftazidime-avibactam, meropenem-vaborbactam, cefiderocol and comparators against Gram-negative organisms causing bloodstream infections in Northern Italy (2019–2021): emergence of complex resistance phenotypes. J Chemother. 2022;34(5):302–10.
Snydman DR, McDermott LA, Jacobus NV. Activity of ceftolozane-tazobactam against a broad spectrum of recent clinical anaerobic isolates. Antimicrob Agents Chemother. 2014;58(2):1218–23.
Armstrong ES, Farrell DJ, Palchak M, Steenbergen JN. In vitro activity of ceftolozane-tazobactam against anaerobic organisms identified during the ASPECT-cIAI study. Antimicrob Agents Chemother. 2016;60(1):666–8.
Stone GG, Newell P, Bradford PA. In vitro activity of ceftazidime-avibactam against isolates from patients in a phase 3 clinical trial for treatment of complicated intra-abdominal infections. Antimicrob Agents Chemother. 2018;62(7):e02584–e2617.
Torres A, Zhong N, Pachl J, Timsit JF, Kollef M, Chen Z, et al. Ceftazidime-avibactam versus meropenem in nosocomial pneumonia, including ventilator-associated pneumonia (REPROVE): a randomised, double-blind, phase 3 non-inferiority trial. Lancet Infect Dis. 2018;18(3):285–95.
Solomkin J, Hershberger E, Miller B, Popejoy M, Friedland I, Steenbergen J, et al. Ceftolozane/tazobactam plus metronidazole for complicated intra-abdominal infections in an era of multidrug resistance: results from a randomized, double-blind, phase 3 trial (ASPECT-cIAI). Clin Infect Dis. 2015;60(10):1462–71.
Kollef MH, Nováček M, Kivistik Ü, Réa-Neto Á, Shime N, Martin-Loeches I, et al. Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2019;19(12):1299–311.
Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). Lancet. 2015;385(9981):1949–56.
Kaye KS, Bhowmick T, Metallidis S, Bleasdale SC, Sagan OS, Stus V, et al. Effect of meropenem-vaborbactam vs piperacillin-tazobactam on clinical cure or improvement and microbial eradication in complicated urinary tract infection: the TANGO I randomized clinical trial. JAMA. 2018;319(8):788–99.
Portsmouth S, van Veenhuyzen D, Echols R, Machida M, Ferreira JCA, Ariyasu M, et al. Cefiderocol versus imipenem-cilastatin for the treatment of complicated urinary tract infections caused by Gram-negative uropathogens: a phase 2, randomised, double-blind, non-inferiority trial. Lancet Infect Dis. 2018;18(12):1319–28.
Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, Mathers AJ, Bassetti M, Vazquez J, et al. Effect and safety of meropenem-vaborbactam versus best-available therapy in patients with carbapenem-resistant Enterobacteriaceae infections: the TANGO II randomized clinical trial. Infect Dis Ther. 2018;7(4):439–55.
Motsch J, Murta de Oliveira C, Stus V, Köksal I, Lyulko O, Boucher HW, et al. RESTORE-IMI 1: a multicenter, randomized, double-blind trial comparing efficacy and safety of imipenem/relebactam vs colistin plus imipenem in patients with imipenem-nonsusceptible bacterial infections. Clin Infect Dis. 2020;70(9):1799–808.
Bassetti M, Echols R, Matsunaga Y, Ariyasu M, Doi Y, Ferrer R, et al. Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect Dis. 2021;21(2):226–40.
Choby JE, Ozturk T, Satola SW, Jacob JT, Weiss DS. Does cefiderocol heteroresistance explain the discrepancy between the APEKS-NP and CREDIBLE-CR clinical trial results? Lancet Microbe. 2021;2(12):e648–9.
Naseer S, Weinstein EA, Rubin DB, Suvarna K, Wei X, Higgins K, et al. US Food and Drug Administration (FDA): benefit-risk considerations for Cefiderocol (Fetroja®). Clin Infect Dis. 2021;72(12):e1103–11.
Wilson GM, Fitzpatrick M, Walding K, Gonzalez B, Schweizer ML, Suda KJ, et al. Meta-analysis of clinical outcomes using ceftazidime/avibactam, ceftolozane/tazobactam, and meropenem/vaborbactam for the treatment of multidrug-resistant Gram-negative infections. Open Forum Infect Dis. 2021;8(2): ofaa651.
Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, et al. Ceftazidime-avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother. 2017;61(8):e00883–e917.
Tumbarello M, Trecarichi EM, Corona A, De Rosa FG, Bassetti M, Mussini C, et al. Efficacy of ceftazidime-avibactam salvage therapy in patients with infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Clin Infect Dis. 2019;68(3):355–64.
Wang W, Wang R, Zhang Y, Zeng L, Kong H, Bai X, et al. Ceftazidime-avibactam as salvage therapy in pediatric liver transplantation patients with infections caused by carbapenem-resistant Enterobacterales. Infect Drug Resist. 2022;15:3323–32.
Castón JJ, Gallo M, García M, Cano A, Escribano A, Machuca I, et al. Ceftazidime-avibactam in the treatment of infections caused by KPC-producing Klebsiella pneumoniae: factors associated with clinical efficacy in a single-center cohort. Int J Antimicrob Agents. 2020;56(3): 106075.
Karaiskos I, Daikos GL, Gkoufa A, Adamis G, Stefos A, Symbardi S, et al. Ceftazidime/avibactam in the era of carbapenemase-producing Klebsiella pneumoniae: experience from a national registry study. J Antimicrob Chemother. 2021;76(3):775–83.
Sousa A, Pérez-Rodríguez MT, Soto A, Rodríguez L, Pérez-Landeiro A, Martínez-Lamas L, et al. Effectiveness of ceftazidime/avibactam as salvage therapy for treatment of infections due to OXA-48 carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73(11):3170–5.
Alraddadi BM, Saeedi M, Qutub M, Alshukairi A, Hassanien A, Wali G. Efficacy of ceftazidime-avibactam in the treatment of infections due to Carbapenem-resistant Enterobacteriaceae. BMC Infect Dis. 2019;19(1):772.
Castón JJ, Cano A, Pérez-Camacho I, Aguado JM, Carratalá J, Ramasco F, et al. Impact of ceftazidime/avibactam versus best available therapy on mortality from infections caused by carbapenemase-producing Enterobacterales (CAVICOR study). J Antimicrob Chemother. 2022;77(5):1452–60.
Balandín B, Ballesteros D, Pintado V, Soriano-Cuesta C, Cid-Tovar I, Sancho-González M, et al. Multicentre study of ceftazidime/avibactam for Gram-negative bacteria infections in critically ill patients. Int J Antimicrob Agents. 2022;59(3): 106536.
Tumbarello M, Raffaelli F, Cascio A, Falcone M, Signorini L, Mussini C, et al. Compassionate use of meropenem/vaborbactam for infections caused by KPC-producing Klebsiella pneumoniae: a multicentre study. JAC Antimicrob Resist. 2022;4(1): dlac022.
Alosaimy S, Lagnf AM, Morrisette T, Scipione MR, Zhao JJ, Jorgensen SCJ, et al. Real-world, multicenter experience with meropenem-vaborbactam for Gram-negative bacterial infections including carbapenem-resistant Enterobacterales and Pseudomonas aeruginosa. Open Forum Infect Dis. 2021;8(8): ofab371.
van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F, et al. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant Enterobacteriaceae. Clin Infect Dis. 2018;66(2):163–71.
Shields RK, McCreary EK, Marini RV, Kline EG, Jones CE, Hao B, et al. Early experience with meropenem-vaborbactam for treatment of carbapenem-resistant Enterobacteriaceae infections. Clin Infect Dis. 2020;71(3):667–71.
Timsit JF, Paul M, Shields RK, Echols R, Baba T, Yamano Y, et al. Cefiderocol for the treatment of infections due to metallo-B-lactamase-producing pathogens in the CREDIBLE-CR and APEKS-NP phase 3 randomized studies. Clin Infect Dis. 2022;75(6):1081–4.
Longshaw C, Roger E, Santerre Henriksen A, Baba T, Nguyen S, Yamano Y. Evidence for efficacy of cefiderocol against OXA-48-containing isolates from the APEKS-NP and CREDIBLE-CR trials. Antimicrob Agents Chemother. 2022;66(10): e0110022.
Kaye KS, Naas T, Pogue JM, Rossolini GM. Cefiderocol, a siderophore cephalosporin, as a treatment option for infections caused by carbapenem-resistant Enterobacterales. Infect Dis Ther. 2023;12(3):777–806.
Shaw E, Rombauts A, Tubau F, Padullés A, Càmara J, Lozano T, et al. Clinical outcomes after combination treatment with ceftazidime/avibactam and aztreonam for NDM-1/OXA-48/CTX-M-15-producing Klebsiella pneumoniae infection. J Antimicrob Chemother. 2018;73(4):1104–6.
Falcone M, Daikos GL, Tiseo G, Bassoulis D, Giordano C, Galfo V, et al. Efficacy of ceftazidime-avibactam plus aztreonam in patients with bloodstream infections caused by metallo-β-lactamase-producing Enterobacterales. Clin Infect Dis. 2021;72(11):1871–8.
Sempere A, Viñado B, Los-Arcos I, Campany D, Larrosa N, Fernández-Hidalgo N, et al. Ceftazidime-avibactam plus aztreonam for the treatment of infections by VIM-type-producing Gram-negative bacteria. Antimicrob Agents Chemother. 2022;66(10): e0075122.
Ackley R, Roshdy D, Meredith J, Minor S, Anderson WE, Capraro GA, et al. Meropenem-vaborbactam versus ceftazidime-avibactam for treatment of carbapenem-resistant Enterobacteriaceae infections. Antimicrob Agents Chemother. 2020;64(5):e02313–e2319.
Gallagher JC, Satlin MJ, Elabor A, Saraiya N, McCreary EK, Molnar E, et al. Ceftolozane-Tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: a multicenter study. Open Forum Infect Dis. 2018;5(11): ofy280.
Castan B, Akrich B, Levy-Bachelot L, Amode A, Berthelot A, Mackosso C, et al. Real-world evaluation of ceftolozane/tazobactam therapy and clinical outcomes in France. Infect Dis Now. 2021;51(6):532–9.
Pogue JM, Kaye KS, Veve MP, Patel TS, Gerlach AT, Davis SL, et al. Ceftolozane/tazobactam vs polymyxin or aminoglycoside-based regimens for the treatment of drug-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2020;71(2):304–10.
Hart DE, Gallagher JC, Puzniak LA, Hirsch EB, C/T Alliance to deliver Real-world Evidence (CARE). A multicenter evaluation of ceftolozane/tazobactam treatment outcomes in immunocompromised patients with multidrug-resistant Pseudomonas aeruginosa infections. Open Forum Infect Dis. 2021;8(3): ofab089.
Balandin B, Ballesteros D, Ruiz de Luna R, López-Vergara L, Pintado V, Sancho-González M, et al. Multicenter study of ceftolozane/tazobactam for treatment of Pseudomonas aeruginosa infections in critically ill patients. Int J Antimicrob Agents. 2021;57(3): 106270.
Corbella L, Boán J, San-Juan R, Fernández-Ruiz M, Carretero O, Lora D, et al. Effectiveness of ceftazidime-avibactam for the treatment of infections due to Pseudomonas aeruginosa. Int J Antimicrob Agents. 2022;59(2): 106517.
Chen J, Liang Q, Chen X, Wu J, Wu Y, Teng G, et al. Ceftazidime/avibactam versus Polymyxin B in the challenge of carbapenem-resistant Pseudomonas aeruginosa infection. Infect Drug Resist. 2022;15:655–67.
Rodríguez-Núñez O, Ripa M, Morata L, de la Calle C, Cardozo C, Fehér C, et al. Evaluation of ceftazidime/avibactam for serious infections due to multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa. J Glob Antimicrob Resist. 2018;15:136–9.
Santevecchi BA, Smith TT, MacVane SH. Clinical experience with ceftazidime/avibactam for treatment of antibiotic-resistant organisms other than Klebsiella pneumoniae. Int J Antimicrob Agents. 2018;51(4):629–35.
Cultrera R, Libanore M, Barozzi A, d’Anchera E, Romanini L, Fabbian F, et al. Ceftolozane/tazobactam and ceftazidime/avibactam for multidrug-resistant Gram-negative infections in immunocompetent patients: a single-center retrospective study. Antibiot Basel Switz. 2020;9(10):640.
Jorgensen SCJ, Trinh TD, Zasowski EJ, Lagnf AM, Bhatia S, Melvin SM, et al. Real-world experience with ceftazidime-avibactam for multidrug-resistant Gram-negative bacterial infections. Open Forum Infect Dis. 2019;6(12): ofz522.
Falcone M, Tiseo G, Leonildi A, Della Sala L, Vecchione A, Barnini S, et al. Cefiderocol- compared to colistin-based regimens for the treatment of severe infections caused by carbapenem-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2022;66(5): e0214221.
Timsit JF, Bassetti M, Cremer O, Daikos G, de Waele J, Kallil A, et al. Rationalizing antimicrobial therapy in the ICU: a narrative review. Intensive Care Med. 2019;45(2):172–89.
Onorato L, Di Caprio G, Signoriello S, Coppola N. Efficacy of ceftazidime/avibactam in monotherapy or combination therapy against carbapenem-resistant Gram-negative bacteria: a meta-analysis. Int J Antimicrob Agents. 2019;54(6):735–40.
Fiore M, Alfieri A, Di Franco S, Pace MC, Simeon V, Ingoglia G, et al. Ceftazidime-avibactam combination therapy compared to ceftazidime-avibactam monotherapy for the treatment of severe infections due to carbapenem-resistant pathogens: a systematic review and network meta-analysis. Antibiot Basel Switz. 2020;9(7):388.
Tumbarello M, Raffaelli F, Giannella M, Mantengoli E, Mularoni A, Venditti M, et al. Ceftazidime-avibactam use for Klebsiella pneumoniae carbapenemase-producing K. pneumoniae infections: a retrospective observational multicenter study. Clin Infect Dis. 2021;73(9):1664–76.
Oliva A, Volpicelli L, Di Bari S, Curtolo A, Borrazzo C, Cogliati Dezza F, et al. Effect of ceftazidime/avibactam plus fosfomycin combination on 30-day mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae: results from a multicentre retrospective study. JAC Antimicrob Resist. 2022;4(6): dlac121.
Xipell M, Bodro M, Marco F, Losno RA, Cardozo C, Soriano A. Clinical experience with ceftazidime/avibactam in patients with severe infections, including meningitis and lung abscesses, caused by extensively drug-resistant Pseudomonas aeruginosa. Int J Antimicrob Agents. 2017;49(2):266–8.
Fiore M, Corrente A, Pace MC, Alfieri A, Simeon V, Ippolito M, et al. Ceftolozane-tazobactam combination therapy compared to ceftolozane-tazobactam monotherapy for the treatment of severe infections: a systematic review and meta-analysis. Antibiot Basel Switz. 2021;10(1):79.
Corcione S, De Benedetto I, Pinna SM, Vita D, Lupia T, Montrucchio G, et al. Cefiderocol use in Gram negative infections with limited therapeutic options: Is combination therapy the key? J Infect Public Health. 2022;15(9):975–9.
Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, Hsueh PR, Viale P, Paño-Pardo JR, et al. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis. 2017;17(7):726–34.
Durante-Mangoni E, Andini R, Zampino R. Management of carbapenem-resistant Enterobacteriaceae infections. Clin Microbiol Infect. 2019;25(8):943–50.
Al-Shaer MH, Rubido E, Cherabuddi K, Venugopalan V, Klinker K, Peloquin C. Early therapeutic monitoring of β-lactams and associated therapy outcomes in critically ill patients. J Antimicrob Chemother. 2020;75(12):3644–51.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, et al. DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58(8):1072–83.
Abdul-Aziz MH, Brady K, Cotta MO, Roberts JA. Therapeutic drug monitoring of antibiotics: defining the therapeutic range. Ther Drug Monit. 2022;44(1):19–31.
Li C, Du X, Kuti JL, Nicolau DP. Clinical pharmacodynamics of meropenem in patients with lower respiratory tract infections. Antimicrob Agents Chemother. 2007;51(5):1725–30.
Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL. Pharmacodynamics of cefepime in patients with Gram-negative infections. J Antimicrob Chemother. 2002;50(3):425–8.
Aitken SL, Altshuler J, Guervil DJ, Hirsch EB, Ostrosky-Zeichner LL, Ericsson CD, et al. Cefepime free minimum concentration to minimum inhibitory concentration (fCmin/MIC) ratio predicts clinical failure in patients with Gram-negative bacterial pneumonia. Int J Antimicrob Agents. 2015;45(5):541–4.
Craig WA, Ebert SC. Killing and regrowth of bacteria in vitro: a review. Scand J Infect Dis Suppl. 1990;74:63–70.
Sumi CD, Heffernan AJ, Lipman J, Roberts JA, Sime FB. What antibiotic exposures are required to suppress the emergence of resistance for Gram-negative bacteria? A systematic review. Clin Pharmacokinet. 2019;58(11):1407–43.
Tam VH, Schilling AN, Neshat S, Poole K, Melnick DA, Coyle EA. Optimization of meropenem minimum concentration/MIC ratio to suppress in vitro resistance of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49(12):4920–7.
Pilmis B, Petitjean G, Lesprit P, Lafaurie M, El Helali N, Le Monnier A, et al. Continuous infusion of ceftolozane/tazobactam is associated with a higher probability of target attainment in patients infected with Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis. 2019;38(8):1457–61.
Roberts JA, Kirkpatrick CMJ, Roberts MS, Dalley AJ, Lipman J. First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents. 2010;35(2):156–63.
Shiu J, Wang E, Tejani AM, Wasdell M. Continuous versus intermittent infusions of antibiotics for the treatment of severe acute infections. Cochrane Database Syst Rev. 2013;2013(3): CD008481.
Falagas ME, Tansarli GS, Ikawa K, Vardakas KZ. Clinical outcomes with extended or continuous versus short-term intravenous infusion of carbapenems and piperacillin/tazobactam: a systematic review and meta-analysis. Clin Infect Dis. 2013;56(2):272–82.
Natesan S, Pai MP, Lodise TP. Determination of alternative ceftolozane/tazobactam dosing regimens for patients with infections due to Pseudomonas aeruginosa with MIC values between 4 and 32 mg/L. J Antimicrob Chemother. 2017;72(10):2813–6.
Han R, Sun D, Li S, Chen J, Teng M, Yang B, et al. Pharmacokinetic/pharmacodynamic adequacy of novel β-lactam/β-lactamase inhibitors against Gram-negative bacterial in critically ill patients. Antibiot Basel Switz. 2021;10(8):993.
Gatti M, Giannella M, Rinaldi M, Gaibani P, Viale P, Pea F. Pharmacokinetic/pharmacodynamic analysis of continuous-infusion fosfomycin in combination with extended-infusion cefiderocol or continuous-infusion ceftazidime-avibactam in a case series of difficult-to-treat resistant Pseudomonas aeruginosa bloodstream infections and/or hospital-acquired pneumonia. Antibiot Basel Switz. 2022;11(12):1739.
Katsube T, Wajima T, Ishibashi T, Arjona Ferreira JC, Echols R. Pharmacokinetic/pharmacodynamic modeling and simulation of cefiderocol, a parenteral siderophore cephalosporin, for dose adjustment based on renal function. Antimicrob Agents Chemother. 2017;61(1):e01381–e1416.
Loeuille G, D’Huart E, Vigneron J, Nisse YE, Beiler B, Polo C, et al. Stability studies of 16 antibiotics for continuous infusion in intensive care units and for performing outpatient parenteral antimicrobial therapy. Antibiot Basel Switz. 2022;11(4):458.
Chen IH, Martin EK, Nicolau DP, Kuti JL. Assessment of meropenem and vaborbactam room temperature and refrigerated stability in polyvinyl chloride bags and elastomeric devices. Clin Ther. 2020;42(4):606–13.
Gorham J, Taccone FS, Hites M. Drug regimens of novel antibiotics in critically ill patients with varying renal functions: a rapid review. Antibiot Basel Switz. 2022;11(5):546.
Crass RL, Rodvold KA, Mueller BA, Pai MP. Renal dosing of antibiotics: are we jumping the gun? Clin Infect Dis. 2019;68(9):1596–602.
Barreto EF, Webb AJ, Pais GM, Rule AD, Jannetto PJ, Scheetz MH. Setting the beta-lactam therapeutic range for critically ill patients: is there a floor or even a ceiling? Crit Care Explor. 2021;3(6): e0446.
Lodise TP, Smith NM, O’Donnell N, Eakin AE, Holden PN, Boissonneault KR, et al. Determining the optimal dosing of a novel combination regimen of ceftazidime/avibactam with aztreonam against NDM-1-producing Enterobacteriaceae using a hollow-fibre infection model. J Antimicrob Chemother. 2020;75(9):2622–32.
de Vroom SL, van Daalen FV, Zieck SE, Mathôt RAA, van Hest RM, Geerlings SE. Does dose reduction of renally cleared antibiotics in patients with impaired renal function lead to adequate drug exposure? A systematic review. Clin Microbiol Infect. 2021;27(3):352–63.
Gaudry S, Hajage D, Schortgen F, Martin-Lefevre L, Pons B, Boulet E, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016;375(2):122–33.
Delattre IK, Hites M, Laterre PF, Dugernier T, Spapen H, Wallemacq PE, et al. What is the optimal loading dose of broad-spectrum β-lactam antibiotics in septic patients? Results from pharmacokinetic simulation modelling. Int J Antimicrob Agents. 2020;56(4): 106113.
Gatti M, Pea F. Antimicrobial dose reduction in continuous renal replacement therapy: myth or real need? A practical approach for guiding dose optimization of novel antibiotics. Clin Pharmacokinet. 2021;60(10):1271–89.
Scheetz MH, Scarsi KK, Ghossein C, Hurt KM, Zembower TR, Postelnick MJ. Adjustment of antimicrobial dosages for continuous venovenous hemofiltration based on patient-specific information. Clin Infect Dis. 2006;42(3):436–7.
Aguilar G, Ferriols R, Martínez-Castro S, Ezquer C, Pastor E, Carbonell JA, et al. Optimizing ceftolozane-tazobactam dosage in critically ill patients during continuous venovenous hemodiafiltration. Crit Care. 2019;23(1):145.
Wenzler E, Butler D, Tan X, Katsube T, Wajima T. Pharmacokinetics, pharmacodynamics, and dose optimization of cefiderocol during continuous renal replacement therapy. Clin Pharmacokinet. 2022;61(4):539–52.
Sime FB, Pandey S, Karamujic N, Parker S, Alexander E, Loutit J, et al. Ex vivo characterization of effects of renal replacement therapy modalities and settings on pharmacokinetics of meropenem and vaborbactam. Antimicrob Agents Chemother. 2018;62(10):e01306–e1318.
Meng L, Mui E, Holubar MK, Deresinski SC. Comprehensive guidance for antibiotic dosing in obese adults. Pharmacotherapy. 2017;37(11):1415–31.
Hites M, Taccone FS, Wolff F, Cotton F, Beumier M, De Backer D, et al. Case-control study of drug monitoring of β-lactams in obese critically ill patients. Antimicrob Agents Chemother. 2013;57(2):708–15.
Alobaid AS, Hites M, Lipman J, Taccone FS, Roberts JA. Effect of obesity on the pharmacokinetics of antimicrobials in critically ill patients: a structured review. Int J Antimicrob Agents. 2016;47(4):259–68.
Arena F, Marchetti L, Henrici De Angelis L, Maglioni E, Contorni M, Cassetta MI, et al. Ceftolozane-tazobactam pharmacokinetics during extracorporeal membrane oxygenation in a lung transplant recipient. Antimicrob Agents Chemother. 2019;63(3):e02131–e2218.
Argudo E, Riera J, Luque S, Los-Arcos I, López-Meseguer M, Sandiumenge A, et al. Effects of the extracorporeal membrane oxygenation circuit on plasma levels of ceftolozane. Perfusion. 2020;35(3):267–70.
König C, Both A, Rohde H, Kluge S, Frey OR, Röhr AC, et al. Cefiderocol in critically ill patients with multi-drug resistant pathogens: real-life data on pharmacokinetics and microbiological surveillance. Antibiot Basel Switz. 2021;10(6):649.
Gatti M, Bartoletti M, Cojutti PG, Gaibani P, Conti M, Giannella M, et al. A descriptive case series of pharmacokinetic/pharmacodynamic target attainment and microbiological outcome in critically ill patients with documented severe extensively drug-resistant Acinetobacter baumannii bloodstream infection and/or ventilator-associated pneumonia treated with cefiderocol. J Glob Antimicrob Resist. 2021;27:294–8.
Hagel S, Bach F, Brenner T, Bracht H, Brinkmann A, Annecke T, et al. Effect of therapeutic drug monitoring-based dose optimization of piperacillin/tazobactam on sepsis-related organ dysfunction in patients with sepsis: a randomized controlled trial. Intensive Care Med. 2022;48(3):311–21.
Ewoldt TMJ, Abdulla A, Rietdijk WJR, Muller AE, de Winter BCM, Hunfeld NGM, et al. Model-informed precision dosing of beta-lactam antibiotics and ciprofloxacin in critically ill patients: a multicentre randomised clinical trial. Intensive Care Med. 2022;48(12):1760–71.
Gatti M, Raschi E, De Ponti F. Serious adverse events with novel beta-lactam/beta-lactamase inhibitor combinations: a large-scale pharmacovigilance analysis. Eur J Clin Microbiol Infect Dis. 2021;40(6):1169–76.
Roger C, Louart B. Beta-lactams toxicity in the intensive care init: an underestimated collateral damage? Microorganisms. 2021;9(7):1505.
Rashid MU, Rosenborg S, Panagiotidis G, Löfdal KS, Weintraub A, Nord CE. Ecological effect of ceftazidime/avibactam on the normal human intestinal microbiota. Int J Antimicrob Agents. 2015;46(1):60–5.
Ruppé É, Lisboa T, Barbier F. The gut microbiota of critically ill patients: first steps in an unexplored world. Intensive Care Med. 2018;44(9):1561–4.
Papp-Wallace KM, Mack AR, Taracila MA, Bonomo RA. Resistance to novel β-lactam-β-lactamase inhibitor combinations: the ‘price of progress.’ Infect Dis Clin North Am. 2020;34(4):773–819.
Humphries RM, Yang S, Hemarajata P, Ward KW, Hindler JA, Miller SA, et al. First report of ceftazidime-avibactam resistance in a KPC-3-expressing Klebsiella pneumoniae isolate. Antimicrob Agents Chemother. 2015;59(10):6605–7.
Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, et al. Emergence of ceftazidime-avibactam resistance due to plasmid-borne blaKPC-3 mutations during treatment of carbapenem-resistant Klebsiella pneumoniae infections. Antimicrob Agents Chemother. 2017;61(3):e02097-e2116.
Giddins MJ, Macesic N, Annavajhala MK, Stump S, Khan S, McConville TH, et al. Successive emergence of ceftazidime-avibactam resistance through distinct genomic adaptations in blaKPC-2-harboring Klebsiella pneumoniae sequence type 307 isolates. Antimicrob Agents Chemother. 2018;62(3):e02101-e2117.
Göttig S, Frank D, Mungo E, Nolte A, Hogardt M, Besier S, et al. Emergence of ceftazidime/avibactam resistance in KPC-3-producing Klebsiella pneumoniae in vivo. J Antimicrob Chemother. 2019;74(11):3211–6.
Zhang P, Shi Q, Hu H, Hong B, Wu X, Du X, et al. Emergence of ceftazidime/avibactam resistance in carbapenem-resistant Klebsiella pneumoniae in China. Clin Microbiol Infect. 2020;26(1):124.e1–124.e4.
Tamma PD, Beisken S, Bergman Y, Posch AE, Avdic E, Sharara SL, et al. Modifiable risk factors for the emergence of ceftolozane-tazobactam resistance. Clin Infect Dis. 2021;73(11):e4599–606.
Johnson MG, Bruno C, Castanheira M, Yu B, Huntington JA, Carmelitano P, et al. Evaluating the emergence of nonsusceptibility among Pseudomonas aeruginosa respiratory isolates from a phase-3 clinical trial for treatment of nosocomial pneumonia (ASPECT-NP). Int J Antimicrob Agents. 2021;57(3): 106278.
Shields RK, Stellfox ME, Kline EG, Samanta P, Van Tyne D. Evolution of imipenem-relebactam resistance following treatment of multidrug-resistant Pseudomonas aeruginosa pneumonia. Clin Infect Dis. 2022;75(4):710–4.
Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ, Bhattacharya J, et al. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med. 2017;196(7):856–63.
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–44.
Arulkumaran N, Routledge M, Schlebusch S, Lipman J, Conway MA. Antimicrobial-associated harm in critical care: a narrative review. Intensive Care Med. 2020;46(2):225–35.
Rhee C, Kadri SS, Dekker JP, Danner RL, Chen HC, Fram D, et al. Prevalence of antibiotic-resistant pathogens in culture-proven sepsis and outcomes associated with inadequate and broad-spectrum empiric antibiotic use. JAMA Netw Open. 2020;3(4): e202899.
Hranjec T, Rosenberger LH, Swenson B, Metzger R, Flohr TR, Politano AD, et al. Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis. 2012;12(10):774–80.
Haidar G, Philips NJ, Shields RK, Snyder D, Cheng S, Potoski BA, et al. Ceftolozane-tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: clinical effectiveness and evolution of resistance. Clin Infect Dis. 2017;65(1):110–20.
McCreary EK, Heil EL, Tamma PD. New perspectives on antimicrobial agents: cefiderocol. Antimicrob Agents Chemother. 2021;65(8): e0217120.
Dickstein Y, Edelman R, Dror T, Hussein K, Bar-Lavie Y, Paul M. Carbapenem-resistant Enterobacteriaceae colonization and infection in critically ill patients: a retrospective matched cohort comparison with non-carriers. J Hosp Infect. 2016;94(1):54–9.
Qin X, Wu S, Hao M, Zhu J, Ding B, Yang Y, et al. The colonization of carbapenem-resistant Klebsiella pneumoniae: epidemiology, resistance mechanisms, and risk factors in patients admitted to intensive care units in China. J Infect Dis. 2020;221(Suppl 2):S206–14.
Qiao F, Huang W, Gao S, Cai L, Zhu S, Wei L, et al. Risk factor for intestinal carriage of carbapenem-resistant Acinetobacter baumannii and the impact on subsequent infection among patients in an intensive care unit: an observational study. BMJ Open. 2020;10(9): e035893.
Satlin MJ, Chen L, Gomez-Simmonds A, Marino J, Weston G, Bhowmick T, et al. Impact of a rapid molecular test for Klebsiella pneumoniae carbapenemase and ceftazidime-avibactam use on outcomes after bacteremia caused by carbapenem-resistant Enterobacterales. Clin Infect Dis. 2022;75(12):2066–75.
Evans SR, Tran TTT, Hujer AM, Hill CB, Hujer KM, Mediavilla JR, et al. Rapid molecular diagnostics to inform empiric use of ceftazidime/avibactam and ceftolozane/tazobactam against Pseudomonas aeruginosa: PRIMERS IV. Clin Infect Dis. 2019;68(11):1823–30.
Bassetti M, Vena A, Giacobbe DR, Falcone M, Tiseo G, Giannella M, et al. Ceftolozane/tazobactam for treatment of severe ESBL-producing Enterobacterales infections: a multicenter nationwide clinical experience (CEFTABUSE II Study). Open Forum Infect Dis. 2020;7(5): ofaa139.
Rubio AM, Kline EG, Jones CE, Chen L, Kreiswirth BN, Nguyen MH, et al. In vitro susceptibility of multidrug-resistant Pseudomonas aeruginosa following treatment-emergent resistance to ceftolozane-tazobactam. Antimicrob Agents Chemother. 2021;65(6):e00084–e121.
Carmeli Y, Armstrong J, Laud PJ, Newell P, Stone G, Wardman A, et al. Ceftazidime-avibactam or best available therapy in patients with ceftazidime-resistant Enterobacteriaceae and Pseudomonas aeruginosa complicated urinary tract infections or complicated intra-abdominal infections (REPRISE): a randomised, pathogen-directed, phase 3 study. Lancet Infect Dis. 2016;16(6):661–73.
Lucasti C, Popescu I, Ramesh MK, Lipka J, Sable C. Comparative study of the efficacy and safety of ceftazidime/avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infections in hospitalized adults: results of a randomized, double-blind, Phase II trial. J Antimicrob Chemother. 2013;68(5):1183–92.
Mazuski JE, Gasink LB, Armstrong J, Broadhurst H, Stone GG, Rank D, et al. Efficacy and safety of ceftazidime-avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infection: results from a randomized, controlled, double-blind, phase 3 program. Clin Infect Dis. 2016;62(11):1380–9.
Qin X, Tran BG, Kim MJ, Wang L, Nguyen DA, Chen Q, et al. A randomised, double-blind, phase 3 study comparing the efficacy and safety of ceftazidime/avibactam plus metronidazole versus meropenem for complicated intra-abdominal infections in hospitalised adults in Asia. Int J Antimicrob Agents. 2017;49(5):579–88.
Vazquez JA, González Patzán LD, Stricklin D, Duttaroy DD, Kreidly Z, Lipka J, et al. Efficacy and safety of ceftazidime-avibactam versus imipenem-cilastatin in the treatment of complicated urinary tract infections, including acute pyelonephritis, in hospitalized adults: results of a prospective, investigator-blinded, randomized study. Curr Med Res Opin. 2012;28(12):1921–31.
Wagenlehner FM, Sobel JD, Newell P, Armstrong J, Huang X, Stone GG, et al. Ceftazidime-avibactam versus doripenem for the treatment of complicated urinary tract infections, including acute pyelonephritis: RECAPTURE, a phase 3 randomized trial. Clin Infect Dis. 2016;63(6):754–62.
Sternbach N, Leibovici Weissman Y, Avni T, Yahav D. Efficacy and safety of ceftazidime/avibactam: a systematic review and meta-analysis. J Antimicrob Chemother. 2018;73(8):2021–9.
Isler B, Ezure Y, Romero JLGF, Harris P, Stewart AG, Paterson DL. Is ceftazidime/avibactam an option for serious infections due to extended-spectrum-β-lactamase- and AmpC-producing enterobacterales?: a systematic review and meta-analysis. Antimicrob Agents Chemother. 2020;65(1):e01052–e1120.
Gaibani P, Campoli C, Lewis RE, Volpe SL, Scaltriti E, Giannella M, et al. In vivo evolution of resistant subpopulations of KPC-producing Klebsiella pneumoniae during ceftazidime/avibactam treatment. J Antimicrob Chemother. 2018;73(6):1525–9.
SPIADI Network. National surveillance of device-associated infection, France, 2021. www.spiadi.fr. Accessed 1 Mar 2023.
Dimelow R, Wright JG, MacPherson M, Newell P, Das S. Population pharmacokinetic modelling of ceftazidime and avibactam in the plasma and epithelial lining fluid of healthy volunteers. Drugs RD. 2018;18(3):221–30.
Stein GE, Smith CL, Scharmen A, Kidd JM, Cooper C, Kuti J, et al. Pharmacokinetic and pharmacodynamic analysis of ceftazidime/avibactam in critically ill patients. Surg Infect. 2019;20(1):55–61.
Nicolau DP, Siew L, Armstrong J, Li J, Edeki T, Learoyd M, et al. Phase 1 study assessing the steady-state concentration of ceftazidime and avibactam in plasma and epithelial lining fluid following two dosing regimens. J Antimicrob Chemother. 2015;70(10):2862–9.
Boselli E, Breilh D, Rimmelé T, Poupelin JC, Saux MC, Chassard D, et al. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30(5):989–91.
Cousson J, Floch T, Guillard T, Vernet V, Raclot P, Wolak-Thierry A, et al. Lung concentrations of ceftazidime administered by continuous versus intermittent infusion in patients with ventilator-associated pneumonia. Antimicrob Agents Chemother. 2015;59(4):1905–9.
Dheyriat L, Bourguignon L, Perpoint T, Ferry T, Goutelle S. Pharmacokinetic/pharmacodynamic simulations of cost-effective dosage regimens of ceftolozane-tazobactam and ceftazidime-avibactam in patients with renal impairment. Antimicrob Agents Chemother. 2022;66(3): e0210421.
Nichols WW, Newell P, Critchley IA, Riccobene T, Das S. Avibactam pharmacokinetic/pharmacodynamic targets. Antimicrob Agents Chemother. 2018;62(6):e02446-e2517.
Yasmin M, Hanrahan J, Marshall S, Lodise TP, Chen L, Perez F, et al. Using therapeutic drug monitoring to treat KPC-producing Klebsiella pneumoniae central nervous system infection with ceftazidime/avibactam. Open Forum Infect Dis. 2020;7(9): ofaa349.
Sime FB, Lassig-Smith M, Starr T, Stuart J, Pandey S, Parker SL, et al. A population pharmacokinetic model-guided evaluation of ceftolozane-tazobactam dosing in critically ill patients undergoing continuous venovenous hemodiafiltration. Antimicrob Agents Chemother. 2019;64(1):e01655–e1719.
Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic-derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2016;56(1):56–66.
Zhanel GG, Chung P, Adam H, Zelenitsky S, Denisuik A, Schweizer F, et al. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination with activity against multidrug-resistant gram-negative bacilli. Drugs. 2014;74(1):31–51.
Caro L, Nicolau DP, De Waele JJ, Kuti JL, Larson KB, Gadzicki E, et al. Lung penetration, bronchopulmonary pharmacokinetic/pharmacodynamic profile and safety of 3 g of ceftolozane/tazobactam administered to ventilated, critically ill patients with pneumonia. J Antimicrob Chemother. 2020;75(6):1546–53.
Kakara M, Larson K, Feng HP, Shiomi M, Yoshitsugu H, Rizk ML. Population pharmacokinetics of tazobactam/ceftolozane in Japanese patients with complicated urinary tract infection and complicated intra-abdominal infection. J Infect Chemother. 2019;25(3):182–91.
Sime FB, Lassig-Smith M, Starr T, Stuart J, Pandey S, Parker SL, et al. Cerebrospinal fluid penetration of ceftolozane-tazobactam in critically Iill patients with an indwelling external ventricular drain. Antimicrob Agents Chemother. 2020;65(1):e01698–e1720.
Bhagunde P, Patel P, Lala M, Watson K, Copalu W, Xu M, et al. Population pharmacokinetic analysis for imipenem-relebactam in healthy volunteers and patients with bacterial infections. CPT Pharmacomet Syst Pharmacol. 2019;8(10):748–58.
Rhee EG, Rizk ML, Calder N, Nefliu M, Warrington SJ, Schwartz MS, et al. Pharmacokinetics, safety, and tolerability of single and multiple doses of relebactam, a β-lactamase inhibitor, in combination with imipenem and cilastatin in healthy participants. Antimicrob Agents Chemother. 2018;62(9):e00280-e318.
Jang SM, Yessayan L, Dean M, Costello G, Katwaru R, Mueller BA. Imipenem/relebactam ex vivo clearance during continuous renal replacement therapy. Antibiot Basel Switz. 2021;10(10):1184.
Wu J, Racine F, Wismer MK, Young K, Carr DM, Xiao JC, et al. Exploring the pharmacokinetic/pharmacodynamic relationship of relebactam (MK-7655) in combination with imipenem in a hollow-fiber infection model. Antimicrob Agents Chemother. 2018;62(5):e02323–e2417.
Couffignal C, Pajot O, Laouénan C, Burdet C, Foucrier A, Wolff M, et al. Population pharmacokinetics of imipenem in critically ill patients with suspected ventilator-associated pneumonia and evaluation of dosage regimens. Br J Clin Pharmacol. 2014;78(5):1022–34.
Rubino CM, Bhavnani SM, Loutit JS, Lohse B, Dudley MN, Griffith DC. Single-dose pharmacokinetics and safety of meropenem-vaborbactam in subjects with chronic renal impairment. Antimicrob Agents Chemother. 2018;62(3):e02103–e2117.
Wenzler E, Gotfried MH, Loutit JS, Durso S, Griffith DC, Dudley MN, et al. Meropenem-RPX7009 concentrations in plasma, epithelial lining fluid, and alveolar macrophages of healthy adult subjects. Antimicrob Agents Chemother. 2015;59(12):7232–9.
Wenzler E, Scoble PJ. An appraisal of the pharmacokinetic and pharmacodynamic properties of meropenem-vaborbactam. Infect Dis Ther. 2020;9(4):769–84.
Kufel WD, Eranki AP, Paolino KM, Call A, Miller CD, Mogle BT. In vivo pharmacokinetic analysis of meropenem/vaborbactam during continuous venovenous haemodialysis. J Antimicrob Chemother. 2019;74(7):2117–8.
Kuti JL, Nicolau DP. Derivation of meropenem dosage in patients receiving continuous veno-venous hemofiltration based on pharmacodynamic target attainment. Chemotherapy. 2005;51(4):211–6.
Zhuang L, Yu Y, Wei X, Florian J, Jang SH, Reynolds KS, et al. Evaluation of hemodialysis effect on pharmacokinetics of meropenem/vaborbactam in end-stage renal disease patients using modeling and simulation. J Clin Pharmacol. 2020;60(8):1011–21.
Griffith DC, Sabet M, Tarazi Z, Lomovskaya O, Dudley MN. Pharmacokinetics/pharmacodynamics of vaborbactam, a novel beta-lactamase inhibitor, in combination with meropenem. Antimicrob Agents Chemother. 2019;63(1):e01659–e1718.
Dagan R, Velghe L, Rodda JL, Klugman KP. Penetration of meropenem into the cerebrospinal fluid of patients with inflamed meninges. J Antimicrob Chemother. 1994;34(1):175–9.
Goncalves-Pereira J, Silva NE, Mateus A, Pinho C, Povoa P. Assessment of pharmacokinetic changes of meropenem during therapy in septic critically ill patients. BMC Pharmacol Toxicol. 2014;14(15):21.
Kothekar AT, Divatia JV, Myatra SN, Patil A, Nookala Krishnamurthy M, Maheshwarappa HM, et al. Clinical pharmacokinetics of 3-h extended infusion of meropenem in adult patients with severe sepsis and septic shock: implications for empirical therapy against Gram-negative bacteria. Ann Intensive Care. 2020;10(1):4.
Ramsey C, MacGowan AP. A review of the pharmacokinetics and pharmacodynamics of aztreonam. J Antimicrob Chemother. 2016;71(10):2704–12.
Singh R, Kim A, Tanudra MA, Harris JJ, McLaughlin RE, Patey S, et al. Pharmacokinetics/pharmacodynamics of a β-lactam and β-lactamase inhibitor combination: a novel approach for aztreonam/avibactam. J Antimicrob Chemother. 2015;70(9):2618–26.
Modai J, Vittecoq D, Decazes JM, Wolff M, Meulemans A. Penetration of aztreonam into cerebrospinal fluid of patients with bacterial meningitis. Antimicrob Agents Chemother. 1986;29(2):281–3.
Kawaguchi N, Katsube T, Echols R, Wajima T. Population pharmacokinetic analysis of cefiderocol, a parenteral siderophore cephalosporin, in healthy subjects, subjects with various degrees of renal function, and patients with complicated urinary tract infection or acute uncomplicated pyelonephritis. Antimicrob Agents Chemother. 2018;62(2):e01391–e1417.
Katsube T, Echols R, Arjona Ferreira JC, Krenz HK, Berg JK, Galloway C. Cefiderocol, a siderophore cephalosporin for Gram-negative bacterial infections: pharmacokinetics and safety in subjects with renal impairment. J Clin Pharmacol. 2017;57(5):584–91.
Saisho Y, Katsube T, White S, Fukase H, Shimada J. Pharmacokinetics, safety, and tolerability of cefiderocol, a novel siderophore cephalosporin for Gram-negative bacteria, in healthy subjects. Antimicrob Agents Chemother. 2018;62(3):e02163–e2217.
Katsube T, Saisho Y, Shimada J, Furuie H. Intrapulmonary pharmacokinetics of cefiderocol, a novel siderophore cephalosporin, in healthy adult subjects. J Antimicrob Chemother. 2019;74(7):1971–4.
Bilal M, El Tabei L, Büsker S, Krauss C, Fuhr U, Taubert M. Clinical pharmacokinetics and pharmacodynamics of cefiderocol. Clin Pharmacokinet. 2021;60(12):1495–508.
Nakamura R, Ito-Horiyama T, Takemura M, Toba S, Matsumoto S, Ikehara T, et al. In vivo pharmacodynamic study of cefiderocol, a novel parenteral siderophore cephalosporin, in murine thigh and lung infection models. Antimicrob Agents Chemother. 2019;63(9):e02031-e2118.
Luque-Paz D, Bennis Y, Jaubert P, Dubée V, Wolff M, Mortaza S. Cerebrospinal fluid concentrations of cefiderocol during the treatment of extensively drug-resistant Pseudomonas aeruginosa ventriculitis. J Antimicrob Chemother. 2022;77(6):1787–9.
Kufel WD, Abouelhassan Y, Steele JM, Guttierez RL, Perwez T, Bourdages G, et al. Plasma and cerebrospinal fluid concentrations of cefiderocol during successful treatment of carbapenem-resistant Acinetobacter baumannii meningitis. J Antimicrob Chemother. 2022;77(10):2737–41.
Marcelo C, de Gea GA, Martinez Palazuelos M, Veganzones J, Grandioso D, Diaz-Pllan B. Clinical cure of a difficult-to-treat resistant Pseudomonas aeruginosa ventriculitis using cefiderocol: a case-report and literature review. Open Forum Infect Dis. 2022;9(8):391.
Katsube T, Nicolau DP, Rodvold KA, Wunderink R, Echols R, Matsunaga Y, et al. Intrapulmonary pharmacokinetic profile of cefiderocol in mechanically ventilated patients with pneumonia. J Antimicrob Chemother. 2021;76(11):2902–5.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the literature search and the writing of the manuscript—all approved the final, submitted version of the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
FB declares having received lecture and consulting fees from MSD, lecture fees for BioMérieux and conference invitation from Pfizer. SH declares having received a conference invitation from Shionogi and lecture fees from Pfizer. OP declares having received consulting fees and conference invitation from MSD, and conference invitation from Correvio. JP declares having received lecture fees from Gilead. JRZ declares having received lecture fees from MSD, Pfizer, Shinogi and BioMérieux, and conference invitations from MSD and Pfizer. All other authors declare having no potential conflict of interest related to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Criteria for literature search.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barbier, F., Hraiech, S., Kernéis, S. et al. Rationale and evidence for the use of new beta-lactam/beta-lactamase inhibitor combinations and cefiderocol in critically ill patients. Ann. Intensive Care 13, 65 (2023). https://doi.org/10.1186/s13613-023-01153-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01153-6