Abstract
Background
The need for continuous renal replacement therapy (CRRT) in critically ill patients with serious infections is associated with clinical failure, emergence of resistance, and excess mortality. These poor outcomes are attributable in large part to subtherapeutic antimicrobial exposure and failure to achieve target pharmacokinetic/pharmacodynamic (PK/PD) thresholds during CRRT. Cefiderocol is a novel siderophore cephalosporin with broad in vitro activity against resistant pathogens and is often used to treat critically ill patients, including those receiving CRRT, despite the lack of data to guide dosing in this population.
Objective
The aim of this study was to evaluate the PK and PD of cefiderocol during in vitro and in vivo CRRT and provide optimal dosing recommendations.
Methods
The PK and dialytic clearance of cefiderocol was evaluated via an established in vitro CRRT model across various modes, filter types, and effluent flow rates. These data were combined with in vivo PK data from nine patients receiving cefiderocol while receiving CRRT from phase III clinical trials. Optimal dosing regimens and their respective probability of target attainment (PTA) were assessed via an established population PK model with Bayesian estimation and 1000-subject Monte Carlo simulations at each effluent flow rate.
Results
The overall mean sieving/saturation coefficient during in vitro CRRT was 0.90 across all modes, filter types, effluent flow rates, and points of replacement fluid dilution tested. Adsorption was negligible at 10.9%. Three-way analysis of variance (ANOVA) and multiple linear regression analyses demonstrated that effluent flow rate is the primary driver of clearance during CRRT and can be used to calculate optimal cefiderocol doses required to match the systemic exposure observed in patients with normal renal function. Bayesian estimation of these effluent flow rate-based optimal doses in nine patients receiving CRRT from the phase III clinical trials of cefiderocol revealed comparable mean (± standard deviation) area under the concentration-time curve values as patients with normal renal function (1709 ± 539 mg·h/L vs. 1494 ± 58.4 mg·h/L; p = 0.26). Monte Carlo simulations confirmed these doses achieved >90% PTA against minimum inhibitory concentrations ≤4 mg/L at effluent flow rates from 0.5 to 5 L/h.
Conclusion
The optimal dosing regimens developed from this work have been incorporated into the prescribing information for cefiderocol, making it the first and only antimicrobial with labeled dosing for CRRT. Future clinical studies are warranted to confirm the efficacy and safety of these regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
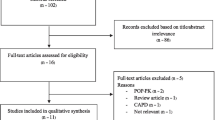
This is the first study to evaluate the pharmacokinetics (PK) of cefiderocol during continuous renal replacement therapy (CRRT) and to provide optimal dosing recommendations for these patients through integration of in vitro modeling, clinical PK, and in silico probability of target attainment (PTA) analyses. The results of this work have been incorporated into the revised prescribing information for cefiderocol, making it the first and only antimicrobial agent with US FDA labeled dosing for CRRT. |
Thorough statistical analysis of in vitro CRRT data supported optimal dosing regimens of cefiderocol based only on effluent flow rate and simplified into four dosage levels. When applied to nine patients undergoing CRRT during phase III trials, these optimal effluent flow rate-based doses resulted in free plasma concentrations ≥8 mg/L in all patients during the dosing interval. |
Monte Carlo simulation at each effluent flow rate demonstrated that the proposed optimal dosing regimens achieved >90% PTA at minimum inhibitory concentration (MIC) values ≤4 mg/L across effluent flow rates from 0.5 to 5 L/h. Therefore, the optimal CRRT dosing regimens developed herein should provide adequate cefiderocol exposure against cefiderocol susceptible, meropenem non-susceptible Enterobacterales, Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia. |
1 Introduction
Serious infections due to difficult-to-treat (DTR) Gram-negative pathogens are responsible for significant morbidity, mortality, and excess healthcare costs [1,2,3,4]. Risk factors for infection due to these pathogens, specifically those that are carbapenem-resistant (CR), are well described and almost always include intensive care unit (ICU) admission, sepsis, renal dysfunction, and/or renal replacement therapy (RRT) [5,6,7]. In addition to acquisition risk, these same factors are also frequently associated with poor clinical outcomes. Recent studies of extended-spectrum β-lactamase (ESBL)-producing and CR Enterobacterales demonstrate that approximately 20% of patients require RRT at baseline and that the need for RRT is independently associated with clinical failure, development of resistance, and mortality [8,9,10,11,12]. Although mortality in this population is likely multifactorial in etiology, pharmacokinetic (PK) alterations in patients receiving continuous RRT (CRRT) have been shown to lead to suboptimal antimicrobial exposures and worse clinical outcomes, especially for highly renally eliminated agents with time-dependent pharmacodynamic (PD) properties such as the β-lactams [13]. Unfortunately, robust PK data in patients receiving CRRT are scarce and often include few critically ill patients on many different modes of CRRT with heterogeneous flow rates, filter types, dosing, and sampling schemes, making it difficult to draw meaningful conclusions [14,15,16,17,18]. As such, in vitro CRRT models are useful for generating precise assessments of sieving/saturation coefficients (SC/SA) across different modes, flow rates, filter types, and points of dilution while eliminating the variability introduced by the patient. These models can be used to guide dosing in the absence of, or when combined with, in vivo data, and have been shown to approximate in vivo total body clearance (CLT) [19], allowing for data derived from in vitro investigations to be utilized in estimating clinical dosing regimens [20].
Cefiderocol is a novel catechol-substituted siderophore cephalosporin antibiotic with potent in vitro activity against clinically relevant DTR Gram-negative bacteria, including CR strains and those producing Ambler class A–D β-lactamases, porin channel alterations, and efflux pump overproduction [21]. Given this broad spectrum of activity, cefiderocol is often used for the treatment of critically ill patients with complex infections due to DTR pathogens, including those receiving CRRT [22]. This is evidenced by the 74 cases treated via the compassionate use program [23], and supported by the Infectious Diseases Society of America Antimicrobial Resistant Treatment Guidance for Gram-Negative Bacterial Infections as an alternative treatment agent [24]. Unfortunately, there are currently no PK data to inform dosing of cefiderocol during CRRT despite that its physiochemical properties (752.2 Da, 40–60% protein binding, apparent volume of distribution [Vd] 18 ± 3.4 L, 98.6% renal excretion) suggest it is likely to be readily dialyzable [25]. As such, the objective of this study was to evaluate the PK of cefiderocol during in vitro and in vivo CRRT in patients treated with cefiderocol while receiving CRRT during the phase III clinical program to provide guidance on optimal dosing in this population.
2 Materials and Methods
2.1 In Vitro CRRT
In vitro CRRT was simulated using a Prismaflex 7.2 control unit (Baxter Healthcare Corporation, Deerfield, IL, USA) in continuous veno-venous hemofiltration (CVVH) and continuous veno-venous hemodialysis (CVVHD) modes using fresh 1.4 m2 polyarylethersulfone (PAES; Prismaflex HF1400) and 1.5 m2 acrylonitrile (AN69; Prismaflex M150) hemofilter sets for each experiment. One liter of heparinized (20 units/mL; West-Ward Pharmaceutical Corp., Eatontown, NJ, USA) bovine plasma containing a potassium oxalate/sodium-fluoride stabilizer (Lampire Biological Labs, Pipersville, PA, USA) was heated to 37 °C in a water bath and stirred continuously. The measured albumin content of the potassium oxalate/sodium-fluoride bovine plasma was 3.74 g/dL (Biologic Resources Laboratory, University of Illinois at Chicago, Chicago, IL, USA), within range of previous in vivo studies of patients undergoing CRRT [26]. The Prismaflex circuit was initially primed with 186 mL (HF1400) or 189 mL (M150) of 0.9% sodium chloride per the manufacturer’s operating instructions [27, 28]. Prior to the start of each experiment, plasma was then allowed to circulate throughout the system for at least 10 min to permit adequate exposure of the hemofilter to proteins. The plasma flow rate was fixed at 200 mL/min for all experiments, while CVVH replacement fluid (PrismaSOL® BGK 2/0; Baxter Healthcare Corporation) and CVVHD dialysate (PrismaSATE® BGK 2/0; Baxter Healthcare Corporation) rates of 2 and 4 L/h were tested with each filter type. During CVVH at 2 L/h, replacement fluid was added at 100% pre-filter, 100% post-filter, and at 50% pre-/50% post-filter. During CVVH at 4 L/h, replacement fluid was added at 50% pre-/50% post-filter. All experiments were performed in at least duplicate in each mode, at each rate, and with each filter for a total of 24 experiments (excluding adsorption experiments).
Cefiderocol (Fetroja®, S-649266, GSK2696266 sodium drug product, Shionogi & Co., Ltd, Osaka, Japan) was reconstituted from vials with sterile water for injection per manufacturer’s instructions. Once reconstituted, cefiderocol was added as a bolus to the central plasma reservoir at a concentration approximately equal to the mean peak serum concentration (Cmax) observed in adults after a 2 g dose infused over 3 h (approximately 90 mg/L) [29] and allowed to equilibrate for at least 1 min prior to sampling. Bovine plasma was also supplemented with urea (Sigma-Aldrich, St Louis, MO, USA) at a concentration of 75 mg/dL and allowed to equilibrate to serve as a control solute.
After equilibration, serial pre-filter plasma samples were collected in K2 EDTA vacutainer tubes (Becton Dickinson, Franklin Lakes, NJ, USA) immediately (0 min) and at 10, 20, 30, 60, and 90 min, with simultaneous post-filter plasma and effluent samples also collected at 10 and 30 min. Plasma and effluent samples were frozen at −80 °C within 30 min of collection until analysis. To ensure sample stability, prior to freezing, plasma and effluent samples were diluted 1:1 with a 0.2 mol/L ammonium acetate buffer (pH 5 ± 0.2) made in-house.
2.2 Adsorption
To evaluate potential adsorption of cefiderocol to the hemofilters, the initial CRRT model was modified to create a closed-circuit system. Effluent was rerouted to the central plasma reservoir and 0.9% normal saline was exogenously pumped into the effluent bag via a Masterflex® Peristaltic pump (Cole-Parmer, Vernon Hills, IL, USA) at the same rate to prevent the Prismaflex system from aborting due to the patient blood loss/gain alarm. Serial plasma samples were drawn from the central reservoir at 0, 10, 20, 30, 45, 60, 90, 105, 120, 150, and 180 min and frozen at −80 °C within 30 min of collection until analysis. A total of six adsorption experiments were performed incorporating various CRRT modes, filters, and flow rates.
2.3 Protein Binding
To assess cefiderocol protein binding in bovine plasma, pre-filter samples taken at 0, 10, 30, and/or 60 min after drug equilibration from four in vitro CRRT experiments along with four contrived samples were immediately centrifuged in a fixed-angle rotor at 1800 × g, 37 °C, 15 min using a Centrifree® Ultrafiltration Device (Merck Millipore Ltd, Tullagreen, Carrigtwohill, County Cork, Ireland). An equal volume of 0.2 mol/L ammonium acetate buffer (pH 5 ± 0.2) was added into an aliquot of the filtrate and the mixture was frozen at −80 °C within 30 min until analysis.
2.4 In Vivo Continuous Renal Replacement Therapy (CRRT)
Nine of the 12 patients from the phase III nosocomial pneumonia (APEKS-NP; n = 3) and CR Gram-negative infection (CREDIBLE-CR; n = 6) studies undergoing CRRT during cefiderocol administration were included in this analysis. Three patients were excluded due to a lack of information on the CRRT effluent flow rate that was necessary to determine the optimal dosing regimen. Full study details have been published previously [30, 31]. The administered dose of cefiderocol was 1 g every 12 h as a 3-h infusion for patients undergoing CVVH and 1.5 g every 12 h as a 3-h infusion for patients undergoing CVVHD or continuous veno-venous hemodiafiltration (CVVHDF). As no data were available at the time of study design, the cefiderocol dosing regimens used for patients receiving CRRT were developed based on the clearance of cefepime during CRRT, given its structural similarity to cefiderocol (accounting for differences in protein binding) and the clearance of cefiderocol during intermittent hemodialysis [32, 33]. Blood samples for PK analysis were obtained pre-filter at a site contralateral to the cefiderocol infusion at steady-state on day 3 prior to the infusion (0 h) and at 1, 3, and 4 h after the start of infusion.
2.5 Bioanalytical Procedures
Concentrations of cefiderocol and urea in bovine plasma and dialysis solutions were measured via validated liquid chromatography-tandem mass spectrometry (Keystone Bioanalytical, North Wales, PA, USA) [34]. The calibration range of the cefiderocol assay was linear from 0.2 to 200 mg/L (r ≥ 0.999). The precision and accuracy acceptance criteria for the quality control samples and calibration standards were ≤15% CV and ±15% relative error determined at each concentration level. The mean percentage recovery of cefiderocol from bovine plasma was 95.7% and all precision and acceptance criteria were met, while the mean percentage recovery of cefiderocol from dialysis solutions was 96.2% and all precision and acceptance criteria were met.
Concentrations of cefiderocol in human plasma were quantified via validated liquid chromatography-tandem mass spectrometry as previously described [35].
2.6 Pharmacokinetic Analysis
2.6.1 In Vitro CRRT
PK parameters for cefiderocol were estimated from observed pre-filter plasma concentrations via non-compartmental analysis in Phoenix WinNonlin version 8.2 (Certara USA Inc., Princeton, NJ, USA). Reported parameters included Cmax, half-life (t½), Vd, clearance (designated CLCRRT), area under the concentration-time curve (AUC) from time zero to infinity (AUC∞) and AUC from time zero to the last measurable concentration (AUClast) as determined via the linear up/log down method. As in vitro experiments were run for 1.5 h, AUClast was multiplied by 16 to demonstrate proportional AUC from time zero to 24 h (AUC24) values. The SC and SA of cefiderocol and urea were calculated as follows [36]:
-
sieving coefficient (SC) = (2 * Cuf) / (Cpre + Cpost)
-
saturation coefficient (SA) = (2 * Cdialysate) / (Cpre + Cpost)
where Cuf is the concentration in the ultrafiltrate, Cpre is the concentration from the pre-filter sampling port, Cdialysate is the concentration in the dialysate, and Cpost is the concentration from the post-filter sampling port [36,37,38].
Adsorption was calculated as the difference between the total amount of cefiderocol added to the system and the total amount recovered in the dialysate and plasma after 180 min using the following equation at each sampling time point:
-
Adsorption (%) = Ʃ1 − [(dose of cefiderocol added at time zero) / (concentration of cefiderocol * measured volume in central reservoir)] [39].
2.7 Dose Optimization
Optimal dosing was calculated to provide a mean AUC value equivalent to that achieved by the 139 cUTI/AP patients administered 2 g every 8 h during the phase III APEKS-cUTI trial (1184 mg·h/L) [40] via the equation AUC = Total Daily Dose/CLT. Clearance by CRRT in vitro (CLCRRT) was substituted for renal CL (CLR) and added to non-renal CL (CLNR) to estimate CLT. CLNR was imputed as the average CLNR from subjects included in the phase I renal impairment study (1.298 L/h), excluding the value from end-stage renal disease subjects receiving dialysis [41], and was assumed to be constant. Calculations were performed for CRRT effluent flow rates from 0.5 to 5 L/h, in 0.5 L/h increments, to generate total daily dose estimations, which were converted to optimal dosing regimens by rounding to the nearest 500 mg and diving into two to three daily doses to align with the labeled dosing of cefiderocol (including the recommended 3-h infusion) [42].
These optimal dosing regimens were then used to calculate the post hoc Cmax, AUC, and plasma trough concentration (Ctrough) for each of the nine CRRT patients. An established population PK model with Bayesian estimation was applied to their individual plasma cefiderocol concentration data to predict CLT [35]. Dosing regimens were then assessed for their probability of target attainment (PTA) based on a %fT>MIC target of ≥75% against minimum inhibitory concentration (MIC) values of 0.25–16 mg/L in log2 dilutions using 1000-subject Monte Carlo simulations at each effluent flow rate. The target 75% fT>MIC was selected from animal infection models, as analysis of phase III data failed to identify a clear PK/PD clinical outcome relationship [35, 43]. For PTA analyses, CLT was again obtained by adding in vitro CLCRRT and CLNR (CLNR was simulated according to uniform distribution from 1.1 to 1.5 L/h [41]) given the minimal variability in CLT observed in vivo secondary to the narrow range of doses and effluent flow rates employed. Steady-state PK were assumed and interindividual variability was set to that of the established population PK model. As body weight and albumin were significant covariates in the population PK model, they were assumed to be log-normally distributed, with a covariance of 30% each and set to the original population mean values of 72.6 kg and 2.8 g/dL, respectively. Free concentrations were estimated using an unbound fraction of 0.422 [44]. Monte Carlo simulations were performed using NONMEM version 7.3 (ICON Development Solutions, Ellicott City, MD, USA) and R version 3.5.1 (The R Foundation for Statistical Computing, Vienna, Austria), as previously described [35].
2.8 Statistical Analysis
Data are presented as mean (± standard deviation [SD]) or with 95% confidence intervals (CIs), or as geometric mean and (CV%) unless otherwise specified. Continuous data were compared via Student’s t-test or Mann–Whitney U test as appropriate. For in vitro data, one- and two-way analysis of variance (ANOVA) models with Tukey’s post hoc test were built to evaluate significant differences in mean CLCRRT according to CVVH point of dilution within and between each filter type. Three-way ANOVA models were then fit using CLCRRT as the outcome to evaluate the interaction between CRRT mode, filter type, and effluent flow rate. ANOVA-generated means of CLCRRT were then used to estimate optimal total daily doses of cefiderocol during CRRT. Finally, multiple linear regression via backwards stepwise analysis was used to correlate effluent flow rate with mean CLCRRT while adjusting for covariates (CRRT mode, filter type, point of dilution, and effluent flow rate) and predict optimal dosing regimens across effluent flow rates from 0.5 to 5 L/h. Model performance was assessed via the adjusted R2 value, and collinearity was assessed via tolerance and variance inflation factors. A p-value ≤ 0.05 was considered statistically significant in the final model. All statistical analyses were performed using SPSS® version 26 (IBM Corporation, Armonk, NY, USA).
3 Results
3.1 In Vitro CRRT
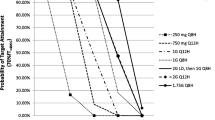
Mean (±SD) pre-filter PK parameters of cefiderocol in bovine plasma during CRRT, as estimated via non-compartmental analyses, are summarized in Table 1, and respective concentration-time profiles are shown in Fig. 1. The mean (±SD) Cmax value observed across the 24 experiments was 92.8 ± 7.24 mg/L, which was ≤3% different from the target value of 90 mg/L. Notably, CLCRRT did not consistently scale exactly proportionally with effluent flow rate and increased 1.4- to 1.8-fold as effluent flow rate increased from 2 to 4 L/h. Overall, the PK were comparable between CRRT modes at the same flow rate. The mean (±SD) AUC24 during CVVH and CVVHD, respectively, at 2 L/h was 914.3 ± 97.3 mg·h/L and 906.7 ± 76.1 mg·h/L (p = 0.89) and at 4 L/h was 597.7 ± 53.8 mg·h/L and 626.5 ± 96.7 mg·h/L (p = 0.62).
Pre-filter plasma concentration-time profiles of cefiderocol during in vitro CVVH and CVVHD at each rate and point of dilution with the HF1400 filter (left) and M150 filter (right). Mean values are displayed with error bars representing standard deviations. CVVH continuous veno-venous hemofiltration, CVVHD continuous veno-venous hemodialysis
Table 2 displays mean (±SD) SC and SA values for cefiderocol stratified by CRRT mode, filter type, effluent flow rate, and point of replacement fluid dilution. The mean cefiderocol SC during CVVH with the M150 filter was 0.855, and 0.984 with the HF1400 (p = 0.019), while mean SA during CVVHD was 0.781 with M150 and 0.940 with HF1400 (p = 0.009). The average SC across CVVH was 0.919, and SA across CVVHD was 0.860 (p = 0.204). The overall mean SC/SA for cefiderocol was 0.90 across all CRRT modes, filter types, effluent flow rates, and points of replacement fluid dilution tested. Mean (±SD) urea SC and SA values across all experiments were 1.06 ± 0.14 and 1.20 ± 0.07, respectively, and were comparable with previously established parameters obtained in analogous experimental conditions [45].
There were no significant differences in CLCRRT during CVVH across any of the three points of dilution (100% pre-filter, 100% post-filter, or 50%/50% pre-/post-filter) regardless of the effluent flow rate tested or filter type used. Ignoring point of dilution, the three-way ANOVA for the effect of CRRT mode, filter type, and effluent flow rate on CLCRRT demonstrated no significant two-way interactions between CRRT mode and filter (p = 0.059), filter and effluent flow rate (p = 0.182), or CRRT mode and effluent flow rate (p = 0.340). The three-way interaction between CRRT mode, filter, and effluent flow rate was also non-significant (p = 0.051), with an adjusted R2 of 0.872. The estimated marginal means and 95% CI for CLCRRT generated from these ANOVAs as a function of CRRT mode, filter type, and effluent flow rate are displayed in electronic supplementary Table 1. Despite consistently higher mean SC and SA values observed for the HF1400 filter compared with the M150 filter, the only significant difference in marginal mean CLCRRT values was observed between CVVHD at 4 L/h with the HF1400 filter (3.355 L/h) and the M150 filter (2.503 L/h) [p = 0.034].
3.2 Adsorption
The overall mean (±SD) percentage adsorption was 10.93 ± 6.28% across CRRT modes, filter types, effluent flow rates, points of dilution, and time. Adsorption peaked at 10–20 min for both filter types. although the percentage adsorbed to the HF1400 filter was significantly higher than to the M150 filter (14.87 ± 0.13% vs. 8.96 ± 4.97%, p = 0.004).
3.3 Protein Binding
Overall, mean (±SD) percentage protein binding in bovine plasma across 16 samples was 36.1 ± 0.04%. No differences were observed between the experimental and contrived samples or between CRRT modes, filter types, or effluent flow rates (data not shown). Protein binding also did not appear to be concentration-dependent as mean percentage bound was approximately constant over time at 0 min (33.9%), 10 min (36.6%), 30 min (36.2%), and 60 min (42.4%).
3.4 In Vivo CRRT
Available characteristics and CRRT settings for each of the nine patients undergoing CRRT from the phase III nosocomial pneumonia (n = 3) and CR Gram-negative infection (n = 6) studies are shown in Table 3. Importantly, the CRRT modalities employed in vivo matched well with our in vitro CRRT model and were representative of the machines, filter types, and settings most commonly utilized in clinical practice worldwide [46, 47]. All but two patients received CRRT via the Prismaflex system with an AN69 filter. The most commonly employed CRRT mode was CVVHDF in seven (78%) patients, with replacement fluid added either 100% pre-filter (n = 2) or 100% post-filter (n = 3) most often. All patients with available data reported a blood flow rate of between 100 and 200 mL/min and a median (interquartile range) effluent flow rate of 1.25 L/h (1.15–2.2 L/h), with 78% of effluent flow rates set between 1 and 3 L/h. Individual observed plasma concentration-time profiles from each of the nine CRRT patients are displayed in Fig. 2.
3.5 Dose Optimization
All four applicable covariates (CRRT mode, filter type, effluent flow rate, and point of dilution) were entered into the multiple linear regression model. Effluent flow rate was the only significant covariate retained in the final model, demonstrating an increase of 0.655 L/h (95% CI 0.508–0.803; p < 0.001) in CLCRRT for every 1 L/h increase in effluent flow rate with excellent correlation (adjusted R2 = 0.856). The regression equation CLCRRT = 0.497 L/h + (effluent flow rate * 0.655) was then used to make predictions for CLCRRT and suggest optimal dosing regimens for cefiderocol during CRRT across effluent flow rates from 0.5 to 5 L/h (Table 4). Four optimal dosing regimens (each infused over 3 h) were proposed over the 10 effluent flow rates simulated, which allowed for simplification into the following recommendations:
-
1.5 g every 12 h for effluent flow rate ≤2 L/h
-
2 g every 12 h for effluent flow rate 2.1–3 L/h
-
1.5 g every 8 h for effluent flow rate 3.1–4 L/h
-
2 g every 8 h for effluent flow rate ≥4.1 L/h
Estimated post hoc plasma cefiderocol PK parameters derived from the population PK model using these optimal effluent flow rate-based dosing regimens for each of the nine CRRT patients individually and in aggregate are shown in Table 5. Electronic supplementary Fig. 1 illustrates the satisfactory individual observed versus predicted fits (R2 = 0.795) for the nine CRRT patients. Additionally, individual predicted plasma concentration-time profiles from the nine CRRT patients receiving optimal effluent flow rate-based dosing regimens are overlayed on the 95% prediction interval of plasma concentrations from patients not undergoing CRRT receiving cefiderocol 2 g every 8 h in phase III studies in Fig. 3. Optimal dosing regimens based on effluent flow rate were equivalent to the dose actually received in the phase III studies for five patients and were higher than the actual dose received in the remaining four patients. The estimated geometric mean (±SD) Cmax and AUC, respectively, for the nine CRRT patients receiving optimal dosing regimens versus those patients from phase III trials with normal renal function receiving 2 g every 8 h were similar at 108 ± 35.7 mg/L versus 101 ± 51.6 mg/L (p = 0.68) and 1709 ± 539 mg·h/L versus 1494 ± 58.4 mg·h/L (p = 0.26). Assuming protein binding of 58%, the predicted geometric mean (range) fCtrough for patients undergoing CRRT receiving optimal dosing regimens was 17.9 mg/L (12.2–39.3 mg/L), with four patients <16 mg/L and no patients <8 mg/L (Table 5). At 75% of the dosing interval (6 or 9 h post-dose), all nine patients had a free plasma concentration ≥8 mg/L (Fig. 3). Similar geometric mean (range) fCtrough values of 12.7 mg/L (0.856–89.5 mg/L) and 16.3 mg/L (2.91–84.8 mg/L) were estimated from the nosocomial pneumonia and CR Gram-negative pathogen studies, respectively.
Individual predicted plasma concentration-time profiles for the nine patients receiving CRRT at optimal effluent flow rate-based dosing regimens (red lines) and the 95% prediction interval of plasma concentrations for patients not undergoing CRRT receiving cefiderocol 2 g every 8 h in phase III trials (gray shaded area). CRRT continuous renal replacement therapy
Figure 4 illustrates the PTA for cefiderocol by effluent flow rate and associated optimal dosing regimen according to MIC, with the actual percentage PTA shown in electronic supplementary Table 2. Across 1000 simulated patients undergoing CRRT at various effluent flow rates, the proposed optimal dosing regimens of cefiderocol conferred >94% PTA against MIC values ≤4 mg/L at all flow rates. Against an MIC of 8 mg/L, PTA was >75% at all 10 effluent flow rates and >80% for all but two flow rates. All PTAs dropped below 60% at an MIC of 16 mg/L.
4 Discussion
Non-clinical and clinical PK/PD models play a critical role in designing human dosage regimens and are essential tools for dose optimization in special patient populations, such as those undergoing CRRT [20, 48]. Critically ill patients with CR infections on concomitant CRRT are at risk for worse outcomes due in large part to suboptimal antimicrobial exposure secondary to inadequate dosing stemming from a lack of reliable PK/PD data [49]. This is the first study to evaluate the PK of cefiderocol during CRRT and to provide optimal dosing recommendations for these patients through integration of in vitro modeling, clinical PK, and in silico PTA analyses. It is also the largest and most comprehensive CRRT study of the modern anti-CR agents to date [39, 50,51,52,53,54]. The results of this work have been incorporated into the revised prescribing information for cefiderocol, making it the first and only antimicrobial agent with US FDA labeled dosing for CRRT [25, 55]. Encouragingly, these optimized CRRT dosing regimens have already begun to demonstrate the ability to achieve target PK/PD thresholds and lead to clinical and microbiological cure against MDR pathogens as predicted herein [56].
Importantly, thorough statistical evaluation provided confidence that the proposed dosing strategies could be simplified to be based only on effluent flow rate while ignoring CRRT mode, filter type, and point of dilution, and thereby easing translation into clinical practice. The predominant influence of effluent flow rate observed in the current study is supported by previous large-scale studies demonstrating clear and consistent associations between CRRT effluent flow rate and clearance of β-lactams such as piperacillin and meropenem [57]. When applied to patients undergoing CRRT during phase III trials, these optimized dosing regimens resulted in comparable exposure to patients with normal renal function receiving the labeled dose of cefiderocol. Furthermore, these optimal effluent flow rate-based dosing regimens were predicted to achieve >90% PTA against MIC values ≤4 mg/L. Given that the MIC90 against meropenem non-susceptible Enterobacterales, Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia is ≤4 mg/L [58], the proposed effluent flow rate-based doses recommended herein should provide adequate cefiderocol exposure against all of these pathogens and cover all organisms considered susceptible based on Clinical and Laboratory Standards Institute (CLSI), FDA, and European Committee on Antimicrobial Susceptibility Testing (EUCAST) interpretive criteria. Finally, as the predicted geometric mean total Ctrough for patients receiving CRRT was 42.4 mg/L, the proposed optimal dosing regimens may also be sufficient to prevent the emergence of resistance to cefiderocol at MICs ≤4 mg/L [59].
In addition to providing clinicians with the first set of dosing recommendations for cefiderocol during CRRT, our study has several other notable strengths. Primarily, our methodology for assessing CLCRRT employed a rich sampling scheme and non-compartmental PK analyses, which significantly improved our ability to accurately estimate drug removal during in vitro CRRT. The majority of previous studies attempt to estimate CLCRRT by multiplying SC or SA derived from a single time point by the flow rate [60,61,62,63]. These methods falsely assume SC and SA are static over time and that CLCRRT is directly proportional to flow rate across the continuum of CRRT settings. Moreover, the methods used for calculating SC, SA, and CLCRRT have varied dramatically throughout the literature, even among the same authors/groups across different studies [36, 64,65,66,67,68,69,70], especially with regard to the influence of point of dilution during CVVH. Therefore, our optimal dosing regimens were generated exclusively via non-compartmental analyses given its increased precision and lack of influence by CRRT mode, filter type, or point of dilution. Notably, our optimized dosing recommendations resulted in the same or higher, but never lower, total daily doses of cefiderocol compared with the dosing regimens used in the phase III trials. This finding highlights the shortcomings of extrapolating data from other agents (even if physiochemically similar), the inability to use CL during intermittent hemodialysis to accurately predict CRRT clearance, and the importance of avoiding unnecessary and detrimental dose reductions in these vulnerable patients [55].
We also directly assessed the effect of protein binding and adsorption on the clearance of cefiderocol during CRRT. Although protein binding is known to be one of the most important factors affecting drug removal during CRRT [49], exceedingly few agents have available data regarding binding to bovine plasma as these animals are not typically utilized in the drug development process [71]. The mean protein binding of 36.1% observed in this study (despite a measured bovine albumin concentration of 3.7 g/dL) was slightly lower than the range previously reported in humans (40–60%) [72]. In the population PK model utilized for this study, a negative correlation between albumin concentration and volume of distribution (V1) was observed, although Cmax, AUC, and CLT were similar regardless of albumin concentration, suggesting hypoalbuminemia may not have a significant effect on cefiderocol exposure. Even if the slightly higher free fraction of cefiderocol in bovine plasma resulted in higher CLCRRT values, and therefore higher than necessary dosing recommendations, the estimated Cmax and AUC of cefiderocol in patients undergoing CRRT receiving optimized effluent flow rate-based dosing regimens were similar to those of patients with normal renal function from the phase III studies and well below the exposure level that has been previously well tolerated after supratherapeutic doses of 3 and 4 g [29].
Although we observed negligible degrees of filter adsorption comparable with those reported for other similar β-lactam agents [39, 73,74,75], which aided in our ability to recommend dosing regimens based strictly on CRRT effluent flow rate, adsorption was significantly higher with the HF1400 filter compared with the M150 filter. This is consistent with our previous investigations [76] and is likely due to known differences in filter composition [77,78,79]. While the interaction between CRRT mode and filter was not statistically significant (p = 0.051), ANOVA-generated marginal mean CLCRRT was significantly higher during CVVHD at 4 L/h with the HF1400 filter versus the M150 filter, suggesting higher doses may need to be considered in this specific situation. As only one CRRT patient had an effluent flow rate >3.5 L/h (fCtrough = 18.8 mg/L), this requires confirmation in future investigations.
Despite these strengths, our study is not without limitations. First, although as many different CRRT modes, filter types, dilution points, and flow rates as possible were included, the results may not be representative of all modalities of CRRT. Second, we assumed non-renal drug clearance to be stable when providing dosing recommendations. Although there are some data to suggest acute kidney injury (AKI) may affect CLNR [80], there are currently no practical methods or useful biomarkers to assess changes in CLNR. We also assumed residual renal function to be negligible as is common in critically ill patients with AKI receiving CRRT [81]. Although this could possibly have underestimated clearance and impacted dosing recommendations, the optimal effluent flow rate-based doses of cefiderocol established in vitro demonstrated adequate in vivo exposure comparable with that observed in patients with normal renal function therefore this is unlikely. Third, the use of a new hemofilter and circuit for each experiment may have limited our ability to fully assess the effect of filter life on adsorption and CLCRRT as well as the impact of repeated cefiderocol dosing. Due to the complicated logistics of in vitro adsorption experiments, caution should be taken when interpreting these data [82]. Fourth, as the PK of cefiderocol have already been extensively described, our 1.5-h sampling scheme in this study was designed solely to evaluate the CLCRRT of cefiderocol during in vitro CRRT, and therefore the half-lives reported should be interpreted with care. Finally, post-filter and effluent samples were not collected in vivo and some patient information was unavailable, including the type of filter used and any interruptions in CRRT therapy that may have impacted the PK results.
5 Conclusion
The thorough exploration of cefiderocol PK during in vitro and in vivo CRRT in this study resulted in optimal dosing recommendations based only on effluent flow rates that provide >90% PTA against pathogens with an MIC ≤4 mg/L. These effluent flow rate-based dosing recommendations have been incorporated into the labeled dosing for cefiderocol and offer a simple dosing algorithm for adoption in the clinical arena. Further confirmation of the efficacy of these doses in clinical studies is warranted.
Change history
06 June 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40262-022-01146-x
References
Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019. Available at: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf Accessed 20 Feb 2020.
Kadri SS, Adjemian J, Lai YL, Spaulding AB, Ricotta E, Prevots DR, et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 us hospitals: retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018;67(12):1803–14.
Kadri SS, Lai YLE, Ricotta EE, Strich JR, Babiker A, Rhee C, et al. External validation of difficult-to-treat resistance prevalence and mortality risk in gram-negative bloodstream infection using electronic health record data from 140 US hospitals. Open Forum Infect Dis. 2019;6(4):110.
Huh K, Chung DR, Ha YE, Ko JH, Kim SH, Kim MJ, et al. Impact of difficult-to-treat resistance in gram-negative bacteremia on mortality: retrospective analysis of nationwide surveillance data. Clin Infect Dis. 2020;71(9):e487–96.
Richter SE, Miller L, Needleman J, Uslan DZ, Bell D, Watson K, et al. Risk factors for development of carbapenem resistance among gram-negative rods. Open Forum Infect Dis. 2019;6(3):027.
Lat I, Daley MJ, Shewale A, Pangrazzi MH, Hammond D, Olsen KM, et al. A multicenter, prospective, observational study to determine predictive factors for multidrug-resistant pneumonia in critically ill adults: the DEFINE study. Pharmacotherapy. 2019;39(3):253–60.
van Loon K, Voor Holt AF, Vos MC. A systematic review and meta-analyses of the clinical epidemiology of carbapenem-resistant enterobacteriaceae. Antimicrob Agents Chemother. 2018;62(1):e01730-e1817.
Alexander EL, Loutit J, Tumbarello M, Wunderink R, Felton T, Daikos G, et al. Carbapenem-resistant enterobacteriaceae infections: results from a retrospective series and implications for the design of prospective clinical trials. Open Forum Infect Dis. 2017;4(2):63.
Shields RK, Nguyen MH, Chen L, Press EG, Kreiswirth BN, Clancy CJ. Pneumonia and renal replacement therapy are risk factors for ceftazidime-avibactam treatment failures and resistance among patients with carbapenem-resistant enterobacteriaceae infections. Antimicrob Agents Chemother. 2018;62(5):e02497-e2517.
Shields RK, McCreary EK, Marini RV, Kline EG, Jones CE, Hao B, et al. Early experience with meropenem-vaborbactam for treatment of carbapenem-resistant enterobacteriaceae infections. Clin Infect Dis. 2019;71(3):667–71.
Eilertson B, Cober E, Richter SS, Perez F, Salata RA, Kalayjian RC, et al. Carbapenem-resistant enterobacteriaceae infections in patients on renal replacement therapy. Open Forum Infect Dis. 2017;4(4):216.
Bassetti M, Vena A, Giacobbe DR, Falcone M, Tiseo G, Giannella M, et al. Ceftolozane/tazobactam for treatment of severe esbl-producing enterobacterales infections: A multicenter nationwide clinical experience (CEFTABUSE II Study). Open Forum Infect Dis. 2020;7(5):139.
Jamal JA, Mueller BA, Choi GY, Lipman J, Roberts JA. How can we ensure effective antibiotic dosing in critically ill patients receiving different types of renal replacement therapy? Diagn Microbiol Infect Dis. 2015;82(1):92–103.
Beumier M, Roberts JA, Kabtouri H, Hites M, Cotton F, Wolff F, et al. A new regimen for continuous infusion of vancomycin during continuous renal replacement therapy. J Antimicrob Chemother. 2013;68(12):2859–65.
Roberts JA, Udy AA, Bulitta JB, Stuart J, Jarrett P, Starr T, et al. Doripenem population pharmacokinetics and dosing requirements for critically ill patients receiving continuous venovenous haemodiafiltration. J Antimicrob Chemother. 2014;69(9):2508–16.
Roberts DM, Liu X, Roberts JA, Nair P, Cole L, Roberts MS, et al. A multicenter study on the effect of continuous hemodiafiltration intensity on antibiotic pharmacokinetics. Crit Care. 2015;19:84.
Jamal JA, Udy AA, Wallis SC, Ranganathan D, McWhinney BC, Ungerer JP, et al. Can we use an ex vivo continuous hemofiltration model to describe the adsorption and elimination of meropenem and piperacillin? Int J Artif Organs. 2015;38(8):419–24.
Roger C, Wallis SC, Muller L, Saissi G, Lipman J, Bruggemann RJ, et al. Caspofungin population pharmacokinetics in critically ill patients undergoing continuous veno-venous haemofiltration or haemodiafiltration. Clin Pharmacokinet. 2017;56(9):1057–68.
Churchwell MD. Use of an in vitro model of renal replacement therapy systems to estimate extracorporeal drug removal. J Clin Pharmacol. 2012;52(1 Suppl):35s–44s.
Bulitta JB, Hope WW, Eakin AE, Guina T, Tam VH, Louie A, et al. Generating robust and informative nonclinical in vitro and in vivo bacterial infection model efficacy data to support translation to humans. Antimicrob Agents Chemother. 2019;63(5):e02307-e2318.
Abdul-Mutakabbir JC, Alosaimy S, Morrisette T, Kebriaei R, Rybak MJ. Cefiderocol: a novel siderophore cephalosporin against multidrug-resistant gram-negative pathogens. Pharmacotherapy. 2020;40(12):1228–47.
McCreary EK, Heil EL, Tamma PD. New perspectives on antimicrobial agents: cefiderocol. Antimicrob Agents Chemother. 2021;65(8):e0217120.
Antimicrobial Drugs Advisory Committee. Cefiderocol Briefing Document NDA # 209445. Advisory Committee Meeting. 16 Oct 2019.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious diseases society of america antimicrobial resistant treatment guidance: gram-negative bacterial infections. Clin Infect Dis. 2020;2:2.
Gatti M, Pea F. Pharmacokinetic/pharmacodynamic target attainment in critically ill renal patients on antimicrobial usage: focus on novel beta-lactams and beta lactams/beta-lactamase inhibitors. Expert Rev Clin Pharmacol. 2021;14(5):583–99.
Wu X, Clancy CJ, Rivosecchi RM, Zhao W, Shields RK, Marini RV, et al. Pharmacokinetics of intravenous isavuconazole in solid-organ transplant recipients. Antimicrob Agents Chemother. 2018;62(12):e01643-e1718.
PRISMAFLEX System M60/M100/M150 Hemofilter Sets. 2016 [cited 12 Jun 2020]. Available at: https://econnect.baxter.com/assets/downloads/products_expertise/renal_therapies/PRISMAFLEX_System_M60_M100_M150.pdf
PRISMAFLEX System HF1000/HF1400 Hemofilter Sets. 2016 [cited 12 Jun 2020]. Available at: https://econnect.baxter.com/assets/downloads/products_expertise/renal_therapies/Prismaflex_HF_Spec_Sheet.pdf
Sanabria C, Migoya E, Mason JW, Stanworth SH, Katsube T, Machida M, et al. Effect of cefiderocol, a siderophore cephalosporin, on QT/QTc interval in healthy adult subjects. Clin Ther. 2019;41(9):1724–36.
Wunderink RG, Matsunaga Y, Ariyasu M, Clevenbergh P, Echols R, Kaye KS, et al. Cefiderocol versus high-dose, extended-infusion meropenem for the treatment of Gram-negative nosocomial pneumonia (APEKS-NP): a randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2021;21(2):213–25.
Bassetti M, Echols R, Matsunaga Y, Ariyasu M, Doi Y, Ferrer R, et al. Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect Dis. 2021;21(2):226–40.
Katsube T, Wajima T, Ishibashi T, Arjona Ferreira JC, Echols R. Dose adjustment of S-649266, a siderophore cephalosporin, for patients requiring haemodialysis [poster 1311]. Presented at the 26th European Congress of Clinical Microbiology and Infectious Diseases, 9–12 April 2016: Amsterdam.
Malone RS, Fish DN, Abraham E, Teitelbaum I. Pharmacokinetics of cefepime during continuous renal replacement therapy in critically ill patients. Antimicrob Agents Chemother. 2001;45(11):3148–55.
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research and Center for Veterinary Medicine. Bioanalytical Method Validation: Guidance for Industry. 2013. Avialable at https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf. Accessed 20 Feb 2020. .
Kawaguchi N, Katsube T, Echols R, Wajima T. Population pharmacokinetic and pharmacokinetic/pharmacodynamic analyses of cefiderocol, a parenteral siderophore cephalosporin, in patients with pneumonia, bloodstream infection/sepsis, or complicated urinary tract infection. Antimicrob Agents Chemother. 2021;65(3):e01437-e1520.
Golper TA, Wedel SK, Kaplan AA, Saad AM, Donta ST, Paganini EP. Drug removal during continuous arteriovenous hemofiltration: theory and clinical observations. Int J Artif Organs. 1985;8(6):307–12.
Churchwell MD, Pasko DA, Mueller BA. Daptomycin clearance during modeled continuous renal replacement therapy. Blood Purif. 2006;24(5–6):548–54.
Schetz M. Drug dosing in continuous renal replacement therapy: general rules. Curr Opin Crit Care. 2007;13(6):645–51.
Sime FB, Pandey S, Karamujic N, Parker S, Alexander E, Loutit J, et al. Ex vivo characterization of effects of renal replacement therapy modalities and settings on pharmacokinetics of meropenem and vaborbactam. Antimicrob Agents Chemother. 2018;62(10):e01306-e1318.
Kawaguchi N, Katsube T, Echols R, Wajima T. Population pharmacokinetic analysis of cefiderocol, a parenteral siderophore cephalosporin, in healthy subjects, subjects with various degrees of renal function, and patients with complicated urinary tract infection or acute uncomplicated pyelonephritis. Antimicrob Agents Chemother. 2018;62(2):e01391-e1417.
Katsube T, Echols R, Arjona Ferreira JC, Krenz HK, Berg JK, Galloway C. Cefiderocol, a siderophore cephalosporin for gram-negative bacterial infections: pharmacokinetics and safety in subjects with renal impairment. J Clin Pharmacol. 2017;57(5):584–91.
FETROJA (cefiderocol) [package insert]. Florham Park, NJ; Shionogi & Co., Ltd. Revised September 2020. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/209445Orig1s000Lbl.pdf. Accessed 5 May 2021.
Nakamura R, Ito-Horiyama T, Takemura M, Toba S, Matsumoto S, Ikehara T, et al. In vivo pharmacodynamic study of cefiderocol, a novel parenteral siderophore cephalosporin, in murine thigh and lung infection models. Antimicrob Agents Chemother. 2019;63(9):e02031-e2118.
Matsumoto S, Singley CM, Hoover J, Nakamura R, Echols R, Rittenhouse S, et al. Efficacy of cefiderocol against carbapenem-resistant gram-negative bacilli in immunocompetent-rat respiratory tract infection models recreating human plasma pharmacokinetics. Antimicrob Agents Chemother. 2017;61(9):e00700-e717.
Troyanov S, Cardinal J, Geadah D, Parent D, Courteau S, Caron S, et al. Solute clearances during continuous venovenous haemofiltration at various ultrafiltration flow rates using Multiflow-100 and HF1000 filters. Nephrol Dial Transplant. 2003;18(5):961–6.
Ricci Z, Ronco C, D’Amico G, De Felice R, Rossi S, Bolgan I, et al. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transplant. 2006;21(3):690–6.
Vaidya M. Continuous Renal Replacement Therapy Industry Worth 1.1 Billion USD by 2020. 3 Jul 2016. Available at: https://issuu.com/makarand.vaidya/docs/continuous_renal_replacement_therap_a10d34dc1adeb9. Accessed 17 Jul 2021.
Trivedi A, Lee RE, Meibohm B. Applications of pharmacometrics in the clinical development and pharmacotherapy of anti-infectives. Expert Rev Clin Pharmacol. 2013;6(2):159–70.
Hoff BM, Maker JH, Dager WE, Heintz BH. Antibiotic dosing for critically ill adult patients receiving intermittent hemodialysis, prolonged intermittent renal replacement therapy, and continuous renal replacement therapy: an update. Ann Pharmacother. 2020;54(1):43–55.
Wenzler E, Bunnell KL, Bleasdale SC, Benken S, Danziger LH, Rodvold KA. Pharmacokinetics and dialytic clearance of ceftazidime-avibactam in a critically ill patient on continuous venovenous hemofiltration. Antimicrob Agents Chemother. 2017;61(7):e00464-e517.
Bunnell KL, Wenzler E, Danziger LH, Rodvold KA. Clearance of ceftazidime-avibactam in an in vitro continuous venovenous hemodialysis model. Open Forum Infect Dis. 2017;4(Suppl 1):S294–5.
Sime FB, Lassig-Smith M, Starr T, Stuart J, Pandey S, Parker SL, et al. A population pharmacokinetic model-guided evaluation of ceftolozane-tazobactam dosing in critically ill patients undergoing continuous venovenous hemodiafiltration. Antimicrob Agents Chemother. 2019;64(1):e01655-e1719.
Kufel WD, Eranki AP, Paolino KM, Call A, Miller CD, Mogle BT. In vivo pharmacokinetic analysis of meropenem/vaborbactam during continuous venovenous haemodialysis. J Antimicrob Chemother. 2019;74(7):2117–8.
Jang SM, Yessayan L, Dean M, et al. Relebactam and imipenem clearance during ex vivo continuous renal replacement therapy [poster P1959]. Presented at the 29th ECCMID; 13-16 April 2019: Amsterdam.
Gatti M, Pea F. Antimicrobial dose reduction in continuous renal replacement therapy: myth or real need? A practical approach for guiding dose optimization of novel antibiotics. Clin Pharmacokinet. 2021;60(10):1271–89.
Fratoni AJ, Kuti JL, Nicolau DP. Optimized cefiderocol exposures in a successfully treated critically ill patient with polymicrobial stenotrophomonas maltophilia bacteremia and pneumonia receiving continuous venovenous hemodiafiltration. Int J Antimicrob Agents. 2021;58(3):106395.
Jamal JA, Udy AA, Lipman J, Roberts JA. The impact of variation in renal replacement therapy settings on piperacillin, meropenem, and vancomycin drug clearance in the critically ill: an analysis of published literature and dosing regimens*. Crit Care Med. 2014;42(7):1640–50.
Yamano Y. In vitro activity of cefiderocol against a broad range of clinically important gram-negative bacteria. Clin Infect Dis. 2019;69(Suppl 7):S544–51.
Sumi CD, Heffernan AJ, Lipman J, Roberts JA, Sime FB. What antibiotic exposures are required to suppress the emergence of resistance for gram-negative bacteria? A systematic review. Clin Pharmacokinet. 2019;58(11):1407–43.
Chaijamorn W, Shaw AR, Lewis SJ, Mueller BA. Ex vivo ceftolozane/tazobactam clearance during continuous renal replacement therapy. Blood Purif. 2017;44(1):16–23.
Lewis SJ, Switaj LA, Mueller BA. Tedizolid adsorption and transmembrane clearance during in vitro continuous renal replacement therapy. Blood Purif. 2015;40(1):66–71.
Kesner JM, Yardman-Frank JM, Mercier RC, Wong CS, Walker SE, Argyres DP, et al. Trimethoprim and sulfamethoxazole transmembrane clearance during modeled continuous renal replacement therapy. Blood Purif. 2014;38(3–4):195–202.
Jang SM, Hough G, Mueller BA. Ex vivo rezafungin adsorption and clearance during continuous renal replacement therapy. Blood Purif. 2018;46(3):214–9.
Akers KS, Rowan MP, Niece KL, Stewart IJ, Mende K, Cota JM, et al. Colistin pharmacokinetics in burn patients during continuous venovenous hemofiltration. Antimicrob Agents Chemother. 2015;59(1):46–52.
Uchino S, Cole L, Morimatsu H, Goldsmith D, Bellomo R. Clearance of vancomycin during high-volume haemofiltration: impact of pre-dilution. Intensive Care Med. 2002;28(11):1664–7.
Janssen PK, Foudraine NA, Burgers DM, Neef K, le Noble JL. Population pharmacokinetics of cefuroxime in critically ill patients receiving continuous venovenous hemofiltration with regional citrate anticoagulation and a phosphate-containing replacement fluid. Ther Drug Monit. 2016;38(6):699–705.
Tegeder I, Bremer F, Oelkers R, Schobel H, Schüttler J, Brune K, et al. Pharmacokinetics of imipenem-cilastatin in critically ill patients undergoing continuous venovenous hemofiltration. Antimicrob Agents Chemother. 1997;41(12):2640–5.
Boucher BA, Hudson JQ, Hill DM, Swanson JM, Wood GC, Laizure SC, et al. Pharmacokinetics of imipenem/cilastatin burn intensive care unit patients undergoing high-dose continuous venovenous hemofiltration. Pharmacotherapy. 2016;36(12):1229–37.
Kiser TH, Fish DN, Aquilante CL, Rower JE, Wempe MF, MacLaren R, et al. Evaluation of sulfobutylether-β-cyclodextrin (SBECD) accumulation and voriconazole pharmacokinetics in critically ill patients undergoing continuous renal replacement therapy. Crit Care. 2015;19(1):32.
Li AM, Gomersall CD, Choi G, Tian Q, Joynt GM, Lipman J. A systematic review of antibiotic dosing regimens for septic patients receiving continuous renal replacement therapy: do current studies supply sufficient data? J Antimicrob Chemother. 2009;64(5):929–37.
Charlson ME, Peterson JC, Krieger KH, Hartman GS, Hollenberg JP, Briggs WM, et al. Improvement of outcomes after coronary artery bypass II: a randomized trial comparing intraoperative high versus customized mean arterial pressure. J Card Surg. 2007;22(6):465–72.
Center for Drug Evaluation and Research. Application Number: 209445Orig1s00. Multi-Disciplinary Review and Evaluation NDA 209445: FETROJA (cefiderocol for Injection).
Maynor LM, Carl DE, Matzke GR, Gehr TW, Farthing C, Farthing D, et al. An in vivo-in vitro study of cefepime and cefazolin dialytic clearance during high-flux hemodialysis. Pharmacotherapy. 2008;28(8):977–83.
Allaouchiche B, Breilh D, Jaumain H, Gaillard B, Renard S, Saux MC. Pharmacokinetics of cefepime during continuous venovenous hemodiafiltration. Antimicrob Agents Chemother. 1997;41(11):2424–7.
Isla A, Gascon AR, Maynar J, Arzuaga A, Toral D, Pedraz JL. Cefepime and continuous renal replacement therapy (CRRT): in vitro permeability of two CRRT membranes and pharmacokinetics in four critically ill patients. Clin Ther. 2005;27(5):599–608.
Andrews L, Benken S, Tan X, Wenzler E. Pharmacokinetics and dialytic clearance of apixaban during in vitro continuous renal replacement therapy. BMC Nephrol. 2021;22(1):45.
Tian Q, Gomersall CD, Ip M, Tan PE, Joynt GM, Choi GYS. Adsorption of amikacin, a significant mechanism of elimination by hemofiltration. Antimicrob Agents Chemother. 2008;52(3):1009–13.
Choi G, Gomersall CD, Lipman J, Wong A, Joynt GM, Leung P, et al. The effect of adsorption, filter material and point of dilution on antibiotic elimination by haemofiltration an in vitro study of levofloxacin. Int J Antimicrob Agents. 2004;24(5):468–72.
Honore PM, Spapen HD. What a clinician should know about a renal replacement membrane? J Transl Int Med. 2018;6(2):62–5.
Vilay AM, Churchwell MD, Mueller BA. Clinical review: drug metabolism and nonrenal clearance in acute kidney injury. Crit Care. 2008;12(6):235.
Choi G, Gomersall CD, Tian Q, Joynt GM, Freebairn R, Lipman J. Principles of antibacterial dosing in continuous renal replacement therapy. Crit Care Med. 2009;37(7):2268–82.
Wenzler E, Biagi M, Tan X, Butler DA. Reply to baud and houze: “should in vitro and in vivo studies on antimicrobial agents during continuous renal replacement therapy comply with general principles of pharmacokinetics?” Antimicrob Agents Chemother. 2020;64(6):e00401-e420.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported in part by an investigator-initiated research grant from Shionogi & Co., Ltd, awarded to EW. Other than the named authors, the study sponsor had no role in the study design, data collection/analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interest/Competing Interests
Eric Wenzler serves on the speaker’s bureau for Melinta Therapeutics, Astellas Pharma, and Allergan Plc., and on the advisory board for GenMark Diagnostics and Shionogi & Co., Ltd. Takayuki Katsube is currently an employee of Shionogi & Co., Ltd, and Toshihiro Wajima was an employee of Shionogi & Co., Ltd at the time of this work. David Butler and Xing Tan certify no potential conflicts of interest.
Ethics Approval
The study design of phase III trials followed US regulatory considerations that were valid in 2016 and were approved by the EMA Committee for Medicinal Products for Human Use (CHMP). Study protocols were approved by relevant national authorities and Institutional Review Boards or independent Ethics Committees. No additional ethical approvals were required for the current study.
Consent to Participate
Written informed consent was obtained from all participants during phase III trials. Informed consent was not necessary for the current work.
Consent for Publication
Not applicable.
Availability of Data and Material
Protocols for the phase III clinical studies are available on ClinicalTrials.gov as NCT03032380, NCT02714595, and NCT02321800. Data generated from this study are not publicly available due to confidentiality agreements with the sponsor, although they may be provided upon reasonable requests by healthcare providers, investigators, and researchers to address specific scientific or clinical objectives.
Code Availability
May be made available upon reasonable request.
Author Contributions
EW was responsible for conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, visualization, and writing/reviewing/editing the manuscript. DB contributed to the conceptualization, formal analysis, investigation, and writing/reviewing/editing the manuscript. XT contributed to the formal analysis, investigation, and writing/reviewing/editing the manuscript. TK and TW contributed to the formal analysis, investigation, and reviewing and editing the manuscript. All authors read and approved the final manuscript.
Additional information
The original online version of the article has been revised due to retrospective open access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wenzler, E., Butler, D., Tan, X. et al. Pharmacokinetics, Pharmacodynamics, and Dose Optimization of Cefiderocol during Continuous Renal Replacement Therapy. Clin Pharmacokinet 61, 539–552 (2022). https://doi.org/10.1007/s40262-021-01086-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-021-01086-y