Abstract
The belief that, for the individual patient, the benefit of prompt and continued use of antimicrobials outweighs any potential harm is a significant barrier to improved stewardship of these vital agents. Antimicrobial stewardship may be perceived as utilitarian rationing, seeking to preserve the availability of effective antimicrobials by limiting the development of resistance in a manner which could conflict with the immediate treatment of the patient in need. This view does not account for the growing evidence of antimicrobial-associated harm to individual patients. This review sets out the evidence for antimicrobial-associated harm and how this should be balanced with the need for prompt and appropriate therapy in infection. It describes the mechanisms by which antimicrobials may harm patients including: mitochondrial toxicity; immune cell toxicity; adverse drug reactions; selection of resistant organisms within a given patient; and disruption of the microbiome. Finally, the article indicates how the harms of antimicrobials may be mitigated and identifies areas for research and development in this field.
Similar content being viewed by others
Antimicrobial stewardship is sometimes perceived by frontline clinicians as the utilitarian rationing of a vital healthcare resource; sacrificing the wellbeing of the present individual for a less immediate collective good. This review sets out the evidence that antimicrobials can cause harm for the individual patient and proposes a research and quality improvement agenda to address this pressing but underacknowledged issue. |
Introduction
One of the major barriers to improved antimicrobial stewardship is the widespread belief amongst both medical professionals and the public that, for the individual patient, the benefits of prompt and continued use of antimicrobials outweigh any potential harm. Antimicrobial stewardship is sometimes perceived as the utilitarian rationing of a vital resource, sacrificing the wellbeing of the present individual for a less immediate collective good. For the clinician, their principal duty to the patient in need outweighs this wider and more nebulous benefit. This view is perhaps most pertinent to critically ill patients, who are the highest per-capita consumers of antimicrobials [1] and who are at greatest risk of harm from untreated or undertreated infection [2, 3].
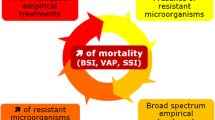
However, there is growing evidence of the harm caused to individual patients by unnecessary or unduly prolonged antimicrobial use [4]. If consideration is given to potential harms in the individual patient, clinicians may be more judicious about antimicrobial prescribing. Several studies conducted within the intensive care unit (ICU) setting have provided compelling evidence that over-zealous use of antimicrobials can translate into adverse patient outcomes, including increased mortality [4,5,6].
This review sets out the evidence for antimicrobial-associated harm, with a specific focus on the critically ill patient. It explores potential mechanisms underlying antimicrobial toxicity, including antimicrobial-induced cellular and mitochondrial toxicity, adverse drug reactions, selection of resistant organisms at individual patient level and disruption of the microbiome. Finally, it discusses approaches to limit antimicrobial-associated harm and highlights research priorities.
The evidence for antimicrobial-associated harm
Initiation of antimicrobial therapy
Early initiation of antimicrobial therapy in bacteraemic septic shock on ICU admission is associated with a mortality benefit [3, 7, 8]. This led to the Surviving Sepsis Campaign guidelines emphasizing the importance of timely, empirical, broad spectrum antimicrobial therapy [9]. However, the effect of the timing of initiation of antimicrobials in patients already in ICU is less clear cut, a large observational multi-centre study possibly suggested that adequacy of antimicrobial coverage may be more critical than time of initiation [10]. In clinical practice, the Surviving Sepsis Campaign guidelines have sometimes resulted in the indiscriminate of empirical broad-spectrum antimicrobials in patients who have uncomplicated infections (an area where the evidence base is far less certain) and in those who have no bacterial infection at all [11]. There is some evidence that suggests that an early empiric approach may cause harm. A quasi-experimental, before and after cohort study [12], performed on patients suspected of having an infection on a single Surgical ICU, compared early antimicrobial administration based solely on clinical grounds to a more conservative strategy, based on waiting for microbiological evidence of infection. There was a significant all-cause mortality benefit among patients treated with the more conservative approach (odds of death ratio 2.5, 95% CI 1.5–4.0), despite a median 10-h prolongation in time to antimicrobial therapy, suggesting inappropriate antimicrobial therapy was associated with significant harm. This approach also appeared to translate into more appropriate antimicrobial choice and a shorter overall course duration.
However, it is important to note several caveats with these data. The data concerning initiation of antimicrobials in ICU comes from observational studies which are subject to inherent biases. For example, in observational studies there may be systematic differences between patients who received earlier and later antimicrobial therapy which were not measured and may influence the effects seen. Equally, Hranjec et al.’s quasi-experimental study [12] occurred in a selected group of patients in a single ICU and may not be generalisable.
Although it is plausible that early initiation of appropriate antimicrobials is beneficial in severe sepsis and septic shock, their over-zealous use in patients without infection is likely to lead to harm [13].
Although beyond the scope of this review, it should be emphasised that prompt source control can be vital in managing sepsis, improving the physiological status of the patient as well as providing samples for microbiological investigation [8, 10, 14].
Duration of antimicrobial therapy
Arguably of greater concern for stewardship efforts in the ICU is the inappropriate continuation of antimicrobials following initiation. The potential harms of this were illustrated in a randomised controlled trial (RCT) of invasive versus non-invasive diagnostic strategies for ventilator-associated pneumonia (VAP). Patients in the invasive group had significantly reduced antimicrobial exposure which was associated with reduced risk-adjusted mortality [15]. Subsequent studies of diagnostic technique did not result in significant reduction in antimicrobial use or mortality [16, 17], implying that it was the reduction in antimicrobials rather than the method of diagnosis that was the key factor. Similarly, in the largest RCT evaluating procalcitonin (PCT) guided cessation of antimicrobials, PCT-guided treatment was associated with lower overall antimicrobial use and mortality [4]. However, the association between shorter duration of antimicrobial use and mortality was not demonstrated by other, smaller, studies [18].
Broad-spectrum antimicrobial combination
Another area where there is evidence that antimicrobials cause harm is in the co-administration of agents. A prospective observational study evaluating the impact of American Thoracic Society/Infectious Diseases Society of America guideline compliance in management of potentially resistant pneumonia demonstrated an excess mortality associated with guideline compliance [5]. The main reasons for non-compliance were non-use of dual treatment for Gram negative pathogens and non-coverage for methicillin-resistant Staphylococcus aureus. This suggests that empirical, concomitant use of several antimicrobials is associated with an excess mortality risk compared to monotherapy [5].
Excessive prolongation
There is a growing body of evidence that antimicrobial course durations are excessive[19]. These have led to calls to abandon the concept of a defined ‘antimicrobial course’ and move to a more individualised approach to antimicrobial duration [20]. An RCT looking at the management of community acquired pneumonia (CAP) showed no significant difference in mortality between median antimicrobial treatment duration of 5 versus 10 days. There was, however, a significant increase in readmission at 30 days in those treated for longer durations; Intriguingly this appears not to have been caused by CAP recurrence, which was similar between the two groups [21].
Several randomised trials have evaluated the duration of antimicrobials in ICU patients. Three studies including patients with VAP [22,23,24] and one with undifferentiated sepsis [25], demonstrated that shorter duration of antimicrobials was not associated with increased mortality risk. It should be noted that, in general, these trials were powered for non-inferiority, which may explain why many of them failed to identify any significant reduction in antimicrobial-associated harm. De-escalation of antimicrobials, being the reduction in spectrum and duration of agents, has been assessed in a number of observational studies in intensive care and one RCT [26], which did not show a survival advantage in de-escalation. However, this literature should give the intensivist confidence that in many cases the duration of antimicrobial courses can be safely shortened and de-escalated, thereby minimising the risk of adverse effects.
Mechanisms of anti-microbial associated harm
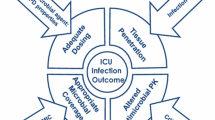
Antimicrobials are able to harm patients by various mechanisms (Fig. 1).
Mechanism: drug toxicity
Antimicrobials are associated with a wide range of well-recognised detrimental side effects including hepatotoxicity, nephrotoxicity, and cytopaenias. The multiple pathophysiological mechanisms underlying these toxicities is not completely understood. The common phylogenetic origin between mitochondria and bacteria [27] suggest that antimicrobials may directly affect human mitochondrial function and may contribute to the mitochondrial dysfunction and associated organ failure in sepsis.
Mechanism: mitochondrial dysfunction and organ dysfunction
Mitochondrial dysfunction is implicated in the pathophysiology of organ dysfunction in sepsis [28], although the mechanisms are poorly understood. At clinically relevant doses, exposure to bactericidal antimicrobials results in mitochondrial dysfunction, reactive oxygen species (ROS) overproduction, reduced ATP, and oxidative damage in mammalian cells ex vivo [29]. Similar changes have been described in patients with sepsis[30, 31]. The diverse mechanisms that underlie antimicrobial-induced mitochondrial damage may provide insight into therapies that aim to mitigate toxicity (Fig. 2).
Antibiotics affect mitochondrial function by multiple mechanisms. Summary of findings from ex-vivo investigation. i Direct inhibition of mitochondrial complex (CI–CIV) activity results in the inability to maintain an electrochemical gradient. ii—iii The loss of mitochondrial membrane potential decreases the ability of the cell to generate ATP. Impaired Complex I and Complex III function result in leak of electrons from the ETC into the matrix, which then allows reaction with oxygen to form the superoxide free radical (O2−). iv Inability of Complex I to form ROS impairs NLRP3 activation; whereas excessive mitochondrial ROS enhances NLRP3 inflammasome activity. In health, superoxide is reduced to hydrogen peroxide (H2O2) by superoxide dismutase (SOD). The hydrogen peroxide is further reduced to water (H2O) by catalase. v If excessive superoxide is produced, the anti-oxidant system is overwhelmed resulting in DNA oxidation and damage. vi Consequently, the ability of the cell to generate new mitochondria (mitochondrial biogenesis) is impaired. vii Additionally, ciprofloxacin is able to inhibit DNA topoisomerase, thereby interfering with mitochondrial DNA replication. viii Beta-lactams fit carriers for mitochondrial substrate uptake, causing reduced succinate uptake. Succinate is converted to fumarate which itself has potent antibacterial effects. C I Complex I, C II Complex II, C III Complex III, C IV Complex IV, C V Complex V/ ATP synthase, Cyt C Cytochrome C, FAD Flavin adenine dinucleotide, FAD Flavin adenine dinucleotide, H2O2 hydrogen peroxide, Q Co-enzyme Q, NAD nicotinamide adenine dinucleotide, SOD superoxide dismutase, Ψ mitochondrial membrane potential
ROS production, antioxidant depletion, and associated oxidative damage in sepsis has been described in several clinical studies [32]. The mitochondrial electron transport chain (ETC) is the major source of ROS production in non-immune cells [33]. A number of antimicrobials including ciprofloxacin and ampicillin inhibit ETC complexes I and III [29]. This disrupts the flow of electrons through the ETC, allowing the leak of electrons into the matrix which react with oxygen to form superoxide [34]. Excessive ROS production can lead to irreversible protein nitration, DNA damage, perpetuation of mitochondrial dysfunction, and cellular dysfunction.
Beta-lactams and cephalosporins fit carriers for mitochondrial substrate uptake, causing reversible inhibition [35] and prolonged exposure to beta-lactams results in irreversible change due to acylation of the transporters [35]. At high doses, several antimicrobials are able to inhibit mitochondrial oxidative phosphorylation [36]. The resulting impairment in substrate availability, ETC complex activity, and decreased ATP production may contribute to organ dysfunction in sepsis [30].
Recovery from sepsis is heralded by increased mitochondrial biogenesis [31]. Mitochondrial topoisomerase II is required for mtDNA replication and transcription; a key feature of mitochondrial biogenesis. This enzyme is susceptible to direct inhibition by antimicrobials including ciprofloxacin, resulting in a loss of mtDNA [37]. Prolonged use of antimicrobials may, therefore, perpetuate organ dysfunction by impairing mitogenesis.
Therapeutic strategies to mitigate antimicrobial-induced cellular dysfunction may be of benefit where prolonged courses of antimicrobials are required. Although mitochondrial-targeted anti-oxidants have demonstrated benefit in experimental sepsis [38], none have been used in clinical trials in septic patients. Clinical trials evaluating non-specific anti-oxidants have failed to demonstrate any clinical benefit [39], reflecting the complexity of the underlying pathology and the difficulty of targeting a mediator as ubiquitous and pluripotent as reactive oxygen species.
Immune function and mitochondria
Many patients with sepsis develop immunoparalysis and are at increased risk of secondary infections [40]. Mitochondria are integral to regulating immune function, and defects in energy metabolism of leukocytes are associated with immunoparalysis in septic patients [41]. Although the adverse effects of antimicrobials on immune cell function have been known for decades [42], their specific impact on immunoparalysis in sepsis and critical illness is unknown. Mitochondria regulate wide-ranging functional responses in innate and adaptive immune cells which may be altered by antimicrobials (Fig. 2).
As an example, electron transport chain adaptations serve as an early immunological-metabolic checkpoint that adjust innate immune responses to bacterial infection [43]. Increased mitochondrial complex II conversion of succinate to fumarate is required for macrophage phagocytic activity. Beta-lactams and cephalosporins fit carriers for mitochondrial substrate uptake [35] and may limit the activity of Complex II. The highly energy-dependent respiratory burst required for bacterial killing by macrophages is impaired by ciprofloxacin through a dose-dependent inhibition of mitochondrial respiratory activity [44].
Whilst excessive ROS may be detrimental, mitochondrial ROS has important signalling roles in immune homeostasis. Cytosolic oxidized mtDNA associates with the NLRP3 inflammasome complex and is required for its activation after the engagement of Toll-like receptors [45]. Inhibition of mitochondrial complex I-induced- ROS impairs NLRP3 inflammasome activity [46], and impaired monocyte NLRP3 activity is associated with mitochondrial dysfunction and increased risk of death in sepsis [47].
The effect of antimicrobials on immune system function are, however, complex, and observations from ex vivo experiments may not always translate to in vivo function. Therefore, whilst the hypothesis that antimicrobials are key drivers of immune cell dysfunction in sepsis and other critical illness syndromes is plausible and supported by mechanistic data, it requires further investigation at a whole organism and patient level.
Mechanism: adverse drug reactions
Commonly encountered manifestations of antimicrobial harm are the various forms of adverse drug reactions that they can provoke. These can be broadly divided into ‘dose dependent’ or predictable reactions, and ‘immunological’ or idiosyncratic reactions. The topic of adverse drug reactions to antimicrobials in intensive care has been reviewed in depth [48], and will be briefly summarised below.
Dose-dependent reactions result from pharmacodynamic interactions between antimicrobials and mammalian cells. Aminoglycosides, glycopeptides, and polymixins have dose-dependent risks of nephrotoxicity, and these agents are amongst those most commonly managed with therapeutic drug monitoring (TDM) as a result [49]. Routine TDM is seldom employed for other antimicrobial classes, although they too can have organ-specific reactions such as beta-lactam and macrolide-induced neurotoxicities [50]. Fluoroquinolones and macrolides lead to cardiac dysrhythmias through interaction with the rapidly activating delayed rectifier potassium channel (IKr) [51]. Fluoroquinolones are also associated with collagen-toxicity which leads to aortic aneurysms and tendinopathy, whilst bone marrow suppression is seen with co-trimoxazole and linezolid. Beyond direct drug toxicity, antimicrobials may alter the plasma levels of other drugs through effects on plasma protein binding or impact on the cytochrome P450 metabolism system. These adverse drug reactions are frequently missed in critically ill patients as they may be misinterpreted as part of the underlying disease process.
Antimicrobials are common triggers of Immune-mediated idiosyncratic reactions such as anaphylaxis [52]. Beyond type I (anaphylactic) reactions, there are a range of other idiosyncratic immune responses that range from mild eosinophilic drug rash to the severe cutaneous adverse reactions (including Toxic Epidermal Necrolysis and Stevens-Johnson syndrome). Within this spectrum there are also a variety of systemic and organ-specific reactions such as serum sickness, hypersensitivity vasculitis, angioedema, acute interstitial nephritis [53]. There is a growing recognition that some of these reactions are not simple immune system-drug interactions, but also involve interactions with viral pathogens. Examples include the rash observed with penicillin treatment in Epstein-Barr Virus infection and the role of Human Herpes Viruses 6/7 in drug rash with eosinophilia and systemic symptoms (DRESS) syndrome [54]. Again, these reactions can, at times, be difficult to distinguish from the underlying disease process.
Conversely, there is an increasing focus on the problem of the documentation of antimicrobial allergy. Rates of reported penicillin allergy far outstrip rates of actual allergy on skin prick testing [55]. This can result in antimicrobial choices with unnecessarily broad spectrum or adverse toxicity profiles, increasing the risk of antimicrobial-induced harm.
Mechanism: antimicrobial resistance
The most widely recognised mechanism of antimicrobial-associated harm is the emergence of antimicrobial resistance (AMR). Whilst the global threat of AMR is now widely acknowledged [56, 57], what has received less attention is the role of antimicrobial therapy in developing subsequent multi-drug resistant (MDR) infections in the patients receiving those antimicrobials.
Infections caused by MDR pathogens are associated with increased mortality and length of stay [58]. They are more likely to be resistant to commonly prescribed empirical antimicrobials and thus introduce delays to appropriate, effective therapy. They also often necessitate treatment with antimicrobials that have inferior bactericidal activity and undesirable pharmacological properties/toxicities, as seen in the comparison between beta-lactam and glycopeptide therapy for S. aureus infection [59]. MDR pathogens are common causes of ICU-acquired infection with one European estimate suggesting that more than two-thirds of cases of ICU-acquired bacteraemia are caused by MDR bacteria [60].
Common MDR bacteria encountered in Intensive Care are linked to the antimicrobials used in critically ill patients. Examples include Gram positive organisms such as methicillin resistant S. aureus (MRSA) and vancomycin resistant enterococci (VRE) the prevalence of which appears to have been relatively stable [61]. Conversely, rates of MDR Gram negative bacteria (e.g. Carbapenem-resistant Pseudomonas aeruginosa, Acinetobacter baumannii and Carbapenem-resistant/extended spectrum beta-lactamase (ESBL) producing Enterobacterales) appear to be rising [62].
Patients in ICU are particularly susceptible to acquiring MDR organisms, either as pathogens or colonisers. One of the causes is the large antimicrobial burden critical care patients are exposed to prior and during their ICU stay. Case–control studies examining risk factors for isolating Carbapenemase-resistant Enterobacterales (CRE) found recent antimicrobial administration, and carbapenems specifically, to be the largest risk factor [63, 64]. Likewise a recent meta-analysis, specifically looking at the risk factors for MDR Gram negative bacteria infection in ICUs, found previous antimicrobial therapy to be key [65].
Respiratory tract infections and VAP [1] account for the majority of hospital-acquired infections. An observational cohort study in suspected VAP and a RCT in microbiologically proven VAP have shown a significant increase in subsequent MDR-related superinfection in patients treated with longer duration of antimicrobial therapy [23, 66]. Crucially neither study showed a mortality benefit with longer antimicrobial use.
It is established that the oropharynx of ventilated patients become colonised with multi-resistant bacteria within a few days of ICU admission [67] and that this is related to antimicrobial use [67]. What is also increasingly being appreciated is that exposure to antimicrobials can lead to colonisation/infection with pathogens resistant to not only the same class, but also different classes of antimicrobials. A study looking at the development of piperacillin-resistant P. aeruginosa VAP showed an association with prior fluoroquinolone treatment [68]. This likely underscores the complex selection pressures driven by antimicrobial therapy on the host microbiome, and how antimicrobial-associated dysbiosis (see below) relates to the selection of MDR organisms. A study performed in two ICUs in the Netherlands, utilizing mathematical modelling, suggested that the predominant route of acquisition of MDR Enterobacterales was endogenous (i.e. from selection pressure applied to the patient’s own gut microbiome), rather than by exogenous cross-contamination (i.e. from other patients, healthcare workers or the environment) [69]. This suggests that infection control/hand hygiene precautions, that have been very effective at reducing rates of MRSA infection [70], may not be as effective in preventing MDR Gram negative infections and that antimicrobial therapy may well be a driver of MDR Gram-negative colonisation in the individual patient.
Mechanism: disruption of the microbiome
When an imbalance of commensal and pathogenic bacteria occurs in a microbiome, known as dysbiosis, the risk increases for local and systemic disease including healthcare-acquired infection (HAI) and associated complications [69, 71]. Not only can alteration of the microbiome and dysbiosis increase risk of infection, it also has the potential to contribute to increase of antimicrobial resistance genes and become a source for MDR organisms such as the ESKAPE organisms [72, 73]. ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, and Enterobacter species) are of worldwide concern as major causes of HAI and can cause life-threatening infections in critical care patients [74]. The impact of dysbiosis extends beyond overgrowth of pathogenic organisms, and a loss of diversity can upset the metabolic symbiosis between the host and its microbiome which may drive inflammation and organ dysfunction directly [75].
Critical illness results in changes to the human microbiome and dysbiosis [72, 76]. A decrease in diversity and commensal organisms, with a concomitant increase in potential pathogens, has been described for the skin, oral, respiratory, and gastrointestinal microbiota of ICU patients [76,77,78]. In mechanically ventilated patients, a decrease in the diversity of the lung microbiome and increase in the abundance of potential pathogens such as staphylococci and Pseudomonas spp. has been reported [77]. Greater lung dysbiosis was demonstrated in patients with VAP compared to ventilated patients without VAP [79]. Despite inter-individual variation in the gut microbiome, marked reductions in bacterial diversity have been described in septic and non-septic critically ill patients [80]. Prolonged ICU admission has also been associated with low gut microbiome diversity and presence of MDR organisms [72]. Whilst the process of critical illness itself contributes to gut microbiome disruption, the frequent use of antimicrobials in ICU can further adversely impact gut microbiome diversity [72, 81]. The high frequency of antimicrobial administration in ICU, makes it challenging to disentangle these processes in human illness [76, 82] although animal models do imply both play a major role [83].
Impact of antimicrobials on the microbiome
Significant loss of gut microbiome diversity has been observed in intensive care patients following the use of broad spectrum antimicrobials such as meropenem [84]. In a study currently being conducted at the ICU of the Royal Brisbane Hospital, Australia, similar findings are observed using shotgun metagenomics. In one particular patient, admitted with burns, classified Candida albicans reads increases to nearly 30% relative abundance following the receipt of antimicrobials including meropenem. Figure 3 illustrates the significant increase of C. albicans in this patient following broad-spectrum antimicrobials (Schlebusch S. pers comm). This finding is consistent with observations by Ravi and colleagues [84]. C. albicans is recognised as a serious concern in critically ill patients and colonization with Candida predisposes for invasive Candida infections in intensive care patients [85].
Analysis of relative abundance changes prior to (sample A) and following broad spectrum antimicrobials (sample B), demonstrating an increase in Ascomycota, all of which identified as C. albicans, using One Codex (https://onecodex.com/) [92]
In 75% of long-stay ICU patients, most of whom received antimicrobials [84], Ravi and colleagues further describe increases in the relative abundance of ESKAPE pathogens such as E. faecium, K.pneumoniae, and E. cloacae, illustrating the selective effect of antimicrobial therapy on resistant microbial populations. In this study 23 of 24 patients received antimicrobials, with meropenem especially being associated with increased abundance of pathogens and loss of putative beneficial species such as Faecalibacterium prauznetzii and Akkermansia muciniphila [84].
Although it is clear that dysbiosis occurs amongst critically ill patients, and that antimicrobials are a major driver of this, it is less clear how this impacts patient outcomes as we do not currently have effective interventions to modify the microbiome. However, there is considerable plausibility from animal models, where antimicrobial-induced dysbiosis worsens spinal cord injury [86], increases the risk of pseudomonal lung infection by affecting mucosal IgA levels [87], and impairs the immune response to Influenza A [88]. In terms of human disease, perhaps the clearest example of a disease arising from dysbiosis is Clostridium difficile-associated diarrhoea (CDAD). Whilst the association between antimicrobial exposure and CDAD is long established, the realisation that this was not simply selection of a resistant organism has come more recently [89]. The role of dysbiosis in CDAD is underlined by the impressive response to faecal microbial transplant [90] and its ability to restore gut microbiota [91].
Reducing harm: the research agenda
What remains to be elucidated is how to mitigate against these harms given the centrality played by antimicrobials in the treatment of infections. Antimicrobial stewardship programmes to reduce the use of antimicrobials in non-bacterial infections and non-infectious conditions reduce harm by reducing exposure [93], whilst efforts to shorten courses avoid unnecessarily broad-spectrum or multiple agents may also be expected to reduce harm. In this area, the domain of healthcare improvement science, we believe that research efforts should focus on determining the optimal components of antimicrobial stewardship programmes and how to drive behaviour change [94].
Secondary infections are common amongst patients in intensive care [40] and efforts to reduce these through prevention programmes can have a significant impact on antimicrobial use [95]. Molecular diagnostic techniques allow more rapid and sensitive testing for infecting organisms [96], whilst host-focussed diagnostics can identify patients with infection as opposed to colonization [94]. However, the impact of these tests on antimicrobial prescribing is not clearly established and should be a focus for future research. The heightened sensitivity of pathogen-focussed tests especially may inappropriately increase the use of antimicrobials. Limiting this inappropriate increase will require distinguishing between invasive infection and benign colonisation and may require the combination of both host and pathogen-focussed tests.
The use of gut microbiome testing for monitoring and guiding antimicrobial choice is promising; however, although direct to consumer testing is available, accredited clinical testing remains elusive [97]. Further research underpinning the clinical validation of gut microbiome testing to progress clinical accreditation of testing is much needed.
A recent meta-analysis of pro-biotics in intensive care patients suggested that administration of these organisms to either the oropharynx or GI tract could reduce development of VAP [98]; however, this approach has not yet found widespread acceptance [99]. Further work in this area would provide vital testing of the mechanistic hypothesis that dysbiosis plays a causative role in adverse outcomes in our patients. However, a note of caution is sounded by reports of both faecal microbiota transplant and probiotic therapy being implicated in bacteraemia [100, 101].
Even with improved stewardship and diagnostics, patients with infections will continue to require antimicrobial therapy, and often resistance patterns will demand the use of broad-spectrum agents with adverse toxicity profiles. We do not know if there are ways of preventing the immuno-suppressive and metabolic side effects of mitochondrial impairment, and similarly beyond avoiding excessive dosing there is limited evidence on how to prevent direct organ toxicity. The development of mito-protective strategies which may counteract the mitochondrial toxicity of antimicrobials are of urgent need. This should be combined with further mechanistic studies on the effects of antimicrobials on immune and solid-organ tissues, which may lead to targeted mito-protective strategies. The successful development of such agents would open up an entirely novel branch of therapeutics.
Ultimately, mitigation of antimicrobial-associated harm is likely to require a multi-faceted approach, combining many or all the approaches discussed above which will need to be both individually proven and then implemented in a bundle of proven interventions.
Summary and conclusions
In conclusion, there is evidence that reducing antimicrobial use in critical care can have a direct impact on individual patients, reducing mortality. The mechanisms by which antimicrobials may worsen outcomes are varied, ranging from direct drug toxicity to dysbiosis, immune cell dysfunction to idiosyncratic drug reactions. Mitigation of these will require a multi-faceted approach. However, the first step in dealing with the problem posed by antimicrobial-associated harm is widespread acknowledgement of this issue. We need to develop an understanding that antimicrobial stewardship is about more than simply attempting to limit the development of microbial resistance and undertake research and quality improvement focusing on understanding and mitigating the serious adverse effects of these vital drugs.
References
Vincent J-L, Rello J, Marshall J et al (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302(21):2323–2329
Kollef MH (2000) Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis 31:S131–S138
Kumar A, Roberts D, Wood KE et al (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 34(6):1589–1596
de Jong E, van Oers JA, Beishuizen A, Infectious PVTL (2016) Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis 16(7):819–827
Kett DH, Cano E, Quartin AA et al (2011) Implementation of guidelines for management of possible multidrug-resistant pneumonia in intensive care: an observational, multicentre cohort study. Lancet Infect Dis 11(3):181–189
Cotten CM, Taylor S, Stoll B et al (2009) Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics 123(1):58–66
Seymour CW, Gesten F, Prescott HC et al (2017) Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 376(23):2235–2244
Bloos F, Rüddel H, Thomas-Rüddel D et al (2017) Effect of a multifaceted educational intervention for anti-infectious measures on sepsis mortality: a cluster randomized trial. Intensive Care Med 43(11):1602–1612
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Bloos F, Thomas-Rüddel D, Rüddel H et al (2014) Impact of compliance with infection management guidelines on outcome in patients with severe sepsis: a prospective observational multi-center study. Crit Care 18(2):R42
Wachter RM, Flanders SA, Fee C, Pronovost PJ (2008) Public reporting of antibiotic timing in patients with pneumonia: lessons from a flawed performance measure. Ann Intern Med 149(1):29–32
Hranjec T, Rosenberger LH, Swenson B et al (2012) Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis 12(10):774–780
Prescott HC, Iwashyna TJ (2019) Improving sepsis treatment by embracing diagnostic uncertainty. Annals ATS 16(4):426–429
De Waele JJ (2010) Early source control in sepsis. Langenbecks Arch Surg 395(5):489–494
Fagon JY, Chastre J, Wolff M et al (2000) Invasive and noninvasive strategies for management of suspected ventilator-associated pneumonia. A randomized trial. Ann Intern Med 132(8):621–630
Canadian Critical Care Trials Group (2006) A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N Engl J Med 355(25):2619–2630
Ruiz M, Torres A, Ewig S et al (2000) Noninvasive versus invasive microbial investigation in ventilator-associated pneumonia: evaluation of outcome. Am J Respir Crit Care Med 162(1):119–125
Bouadma L, Luyt C-E, Tubach F et al (2010) Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 375(9713):463–474
Onakpoya IJ, Walker AS, Tan PS et al (2018) Overview of systematic reviews assessing the evidence for shorter versus longer duration antibiotic treatment for bacterial infections in secondary care. PLoS ONE 13(3):e0194858
Llewelyn MJ, Fitzpatrick JM, Darwin E et al (2017) The antibiotic course has had its day. BMJ 358:j3418
Uranga A, España PP, Bilbao A et al (2016) Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med 176(9):1257–1265
Capellier G, Mockly H, Charpentier C, et al. (2012) Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. Spellberg B, ed. PLoS One 7(8):e41290–12
Chastre J, Wolff M, Fagon J-Y et al (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA 290(19):2588–2598
Kollef MH, Chastre J, Clavel M et al (2012) A randomized trial of 7-day doripenem versus 10-day imipenem-cilastatin for ventilator-associated pneumonia. Crit Care 16(6):R218
Scawn N, Saul D, Pathak D et al (2012) A pilot randomised controlled trial in intensive care patients comparing 7 days’ treatment with empirical antibiotics with 2 days’ treatment for hospital-acquired infection of unknown origin. Health Technol Assess 16(36):1–94
Leone M, Bechis C, Baumstarck K et al (2014) De-escalation versus continuation of empirical antimicrobial treatment in severe sepsis: a multicenter non-blinded randomized noninferiority trial. Intensive Care Med 40(10):1399–1408
Carvalho DS, Andrade RFS, Pinho STR et al (2015) What are the evolutionary origins of mitochondria? A complex network approach. PLoS ONE 10(9):e0134988–e135021
Singer M (2013) The role of mitochondrial dysfunction in sepsis-induced multi-organ failure. Virulence 5(1):66–72
Kalghatgi S, Spina CS, Costello JC et al (2013) Bactericidal antibiotics induce mitochondrial dysfunction and oxidative damage in mammalian cells. Science Trans Med 5(192):192
Brealey D, Brand M, Hargreaves I et al (2002) Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 360(9328):219–223
Carré JE, Orban J-C, Re L et al (2010) Survival in critical illness is associated with early activation of mitochondrial biogenesis. Am J Respir Crit Care Med 182(6):745–751
Galley HF (2011) Oxidative stress and mitochondrial dysfunction in sepsis. Br J Anaesth 107(1):57–64
Turrens JF (2003) Mitochondrial formation of reactive oxygen species. J Physiol 552(2):335–344
Dröse S, Brandt U (2008) The mechanism of mitochondrial superoxide production by the cytochrome bc1 complex. J Biol Chem 283(31):21649–21654
Tune BM, Hsu CY (1990) The renal mitochondrial toxicity of beta-lactam antibiotics: in vitro effects of cephaloglycin and imipenem. J Am Soc Nephrol 1(5):815–821
Duewelhenke N, Krut O, Eysel P (2007) Influence on mitochondria and cytotoxicity of different antibiotics administered in high concentrations on primary human osteoblasts and cell lines. Antimicrob Agents Chemother 51(1):54–63
Lawrence JW, Claire DC, Weissig V, Rowe TC (1996) Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells. Mol Pharmacol 50(5):1178–1188
Mantzarlis K, Tsolaki V, Zakynthinos E (2017) Role of oxidative stress and mitochondrial dysfunction in sepsis and potential therapies. Ox Med Cell Long 2017(7):1–10
Manzanares W, Lemieux M, Elke G, Langlois PL, Bloos F, Heyland DK (2016) High-dose intravenous selenium does not improve clinical outcomes in the critically ill: a systematic review and meta-analysis. Crit Care 20:356
Morris AC, Datta D, Shankar-Hari M et al (2018) Cell-surface signatures of immune dysfunction risk-stratify critically ill patients: INFECT study. Intensive Care Med 44(5):627–635
Cheng S-C, Scicluna BP, Arts RJW et al (2016) Broad defects in the energy metabolism of leukocytes underlie immunoparalysis in sepsis. Nat Immunol 17(4):406–413
Hauser WE, Remington JS (1982) Effect of antibiotics on the immune response. Am J Med 72(5):711–716
Garaude J, Acín-Pérez R, Martínez-Cano S et al (2016) Mitochondrial respiratory-chain adaptations in macrophages contribute to antibacterial host defense. Nat Immunol 17(9):1037–1045
Yang JH, Bhargava P, McCloskey D, Mao N, Palsson BO, Collins JJ (2017) Antibiotic-induced changes to the host metabolic environment inhibit drug efficacy and alter immune function. Cell Host Microbe 22(6):757–765.e3
Zhong Z, Liang S, Sanchez-Lopez E et al (2018) New mitochondrial DNA synthesis enables NLRP3 inflammasome activation. Nature 560(7717):198–203
Kelly B, Tannahill GM, Murphy MP, O'Neill LAJ (2015) Metformin inhibits the production of reactive oxygen species from NADH: ubiquinone oxidoreductase to limit induction of interleukin-1β (IL-1β) and boosts interleukin-10 (IL-10) in lipopolysaccharide (LPS)-activated macrophages. J Biol Chem 290(33):20348–20359
Martínez-García JJ, Martínez-Banaclocha H, Angosto-Bazarra D et al (2019) P2X7 receptor induces mitochondrial failure in monocytes and compromises NLRP3 inflammasome activation during sepsis. Nature Comms 10(1):2711
Granowitz EV, Brown RB (2008) Antibiotic adverse reactions and drug interactions. Crit Care Clin 24(2):421–442
Jager NGL, van Hest RM, Lipman J, Taccone FS, Roberts JA (2016) Therapeutic drug monitoring of anti-infective agents in critically ill patients. Expert Rev Clin Pharm 9(7):961–979
Bhattacharyya S, Darby RR, Raibagkar P, Gonzalez Castro LN, Berkowitz AL (2016) Antibiotic-associated encephalopathy. Neurology 86(10):963–971
Cornett E, Novitch MB, Kaye AD et al (2017) Macrolide and fluoroquinolone mediated cardiac arrhythmias: clinical considerations and comprehensive review. Postgrad Med 129(7):715–724
Harper NJN, Cook TM, Garcez T et al (2018) Anaesthesia, surgery, and life-threatening allergic reactions: epidemiology and clinical features of perioperative anaphylaxis in the 6th National Audit Project (NAP6). Br J Anaes 121(1):159–171
Kanji S, Chant C (2010) Allergic and hypersensitivity reactions in the intensive care unit. Critical Care Med 38:S162–S168
Blumenthal KG, Peter JG, Trubiano JA, Phillips EJ (2019) Antibiotic allergy. Lancet 393(10167):183–198
Blumenthal KG, Ryan EE, Li Y, Lee H, Kuhlen JL, Shenoy ES (2017) The impact of a reported penicillin allergy on surgical site infection risk. Clin Infect Dis 66(3):329–336
Tackling antimicrobial resistance 2019–2024 The UK’s five-year national action plan, HM Government (2019) https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/784894/UK_AMR_5_year_national_action_plan.pdf. Accessed 20 Dec 2019
Global action plan on antimicrobial resistance, WHO (2015) https://www.who.int/antimicrobial-resistance/global-action-plan/en/. Accessed 20 Dec 2019
Neidell MJ, Cohen B, Furuya Y et al (2012) Costs of healthcare- and community-associated infections with antimicrobial-resistant versus antimicrobial-susceptible organisms. Clin Infect Dis 55(6):807–815
Apellaniz G, Valdés M, Perez R et al (1991) Comparison of the effectiveness of various antibiotics in the treatment of methicillin-susceptible Staphylococcus aureus experimental infective endocarditis. J Chemother 3(2):91–97
Tabah A, Koulenti D, Laupland K et al (2012) Characteristics and determinants of outcome of hospital-acquired bloodstream infections in intensive care units: the EUROBACT International Cohort Study. Intensive Care Med 38(12):1930–1945
Global priority list of antibiotic-resistant bacteria to guide research, discovery and development of new antibiotics (2017) https://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf. Accessed 20 Dec 2019
Munoz-Price LS, Poirel L, Bonomo RA et al (2013) Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 13(9):785–796
Marchaim D, Chopra T, Bhargava A et al (2015) recent exposure to antimicrobials and carbapenem-resistant Enterobacteriaceae: the role of antimicrobial stewardship. Infect Control Hosp Epidemiol 33(8):817–830
Armand-Lefèvre L, Angebault C, Barbier F et al (2013) Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother 57(3):1488–1495
Ang H, Sun X (2018) Risk factors for multidrug-resistant Gram-negative bacteria infection in intensive care units: a meta-analysis. Int J Nurs Pract 24(4):e12644–e12713
Raman K, Nailor MD, Nicolau DP, Aslanzadeh J, Nadeau M, Kuti JL (2013) Early antibiotic discontinuation in patients with clinically suspected ventilator-associated pneumonia and negative quantitative bronchoscopy cultures. Crit Care Med 41(7):1656–1663
Ewig S, Torres A, El-Ebiary M, et al. (1999) Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Incidence, risk factors, and association with ventilator-associated pneumonia. Am J Respir Crit Care Med 159(1): 188–198
Trouillet JL, Vuagnat A, Combes A, Kassis N, Chastre J, Gibert C (2002) Pseudomonas aeruginosa ventilator-associated pneumonia: comparison of episodes due to piperacillin-resistant versus piperacillin-susceptible organisms. Clin Infect Dis 34(8):1047–1054
Bootsma M, Bonten M, Nijssen S, Fluit A, Diekmann O (2007) An Algorithm to estimate the importance of bacterial acquisition routes in hospital settings. Am J Epidemiol 166(7):841–851
Derde LPG, Cooper BS, Goossens H et al (2014) Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis. 14(1):31–39
Wischmeyer PE, McDonald D, Knight R (2016) Role of the microbiome, probiotics, and “dysbiosis therapy” in critical illness. Curr Opin Crit Care 22(4):347–353
Zaborin A, Smith D, Garfield K, et al. (2014) Membership and behavior of ultra-low-diversity pathogen communities present in the gut of humans during prolonged critical illness Clemente J, Dominguez Bello MG, eds. mBio 5(5): 01361–14
Baron SA, Diene SM, Rolain JM (2018) Human microbiomes and antibiotic resistance. Human Microbiome J 10:43–52
Santajit S, Indrawattana N (2016) Mechanisms of antimicrobial resistance in ESKAPE pathogens. BioMed Res Int. https://doi.org/10.1155/2016/2475067
Saltzman ET, Palacios T, Thomsen M, Vitetta L (2018) Intestinal microbiome shifts, dysbiosis, inflammation, and non-alcoholic fatty liver disease. Front Microbiol 9:307–311
McDonald D, Ackermann G, Khailova L, et al. (2016) Extreme dysbiosis of the microbiome in critical illness. Green Tringe S, ed. mSphere 1(4):207–6
Alagna L, Bandera A, Patruno A, Muscatello A, Citerio G, Gori A (2019) Microbiota in ICU, not only a gut problem. Intensive Care Med 45(5):733–737
Yeh A, Rogers MB, Firek B, Neal MD, Zuckerbraun BS, Morowitz MJ (2016) Dysbiosis across multiple body sites in critically ill adult surgical patients. Shock 46(6):649–654
Zakharkina T, Martin-Loeches I, Matamoros S et al (2017) The dynamics of the pulmonary microbiome during mechanical ventilation in the intensive care unit and the association with occurrence of pneumonia. Thorax 72(9):803–810
Lankelma JM, Vught LA, Belzer C et al (2016) Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med 43(1):59–68
Pettigrew MM, Gent JF, Kong Y et al (2018) Gastrointestinal microbiota disruption and risk of colonization with carbapenem-resistant Pseudomonas aeruginosa in Intensive Care Unit Patients. Clin Infect Dis 69(4):604–613
Otani S, Chihade DB, Coopersmith CM (2019) Critical illness and the role of the microbiome. Acute Med Surg 6(2):91–94
Dickson RP, Singer BH, Newstead MW et al (2016) Enrichment of the lung microbiome with gut bacteria in sepsis and the acute respiratory distress syndrome. Nat Microbiol 1(10):16113
Ravi A, Halstead FD, Bamford A et al (2019) Loss of microbial diversity and pathogen domination of the gut microbiota in critically ill patients. bioRxiv 9:151–236
Hankovszky P, Társy D, Öveges N, Molnár Z (2015) Invasive Candida infections in the ICU: diagnosis and therapy. J Crit Care Med 1(4):129–139
Kigerl KA, Hall JCE, Wang L, Mo X, Yu Z, Popovich PG (2016) Gut dysbiosis impairs recovery after spinal cord injury. J Exp Med 213(12):2603–2620
Robak OH, Heimesaat MM, Kruglov AA et al (2018) Antibiotic treatment–induced secondary IgA deficiency enhances susceptibility to Pseudomonas aeruginosa pneumonia. J Clin Invest 128(8):3535–3545
Ichinohe T, Pang IK, Kumamoto Y et al (2011) Microbiota regulates immune defense against respiratory tract influenza A virus infection. Proc Natl Acad Sci USA 108(13):5354–5359
Johanesen P, Mackin K, Hutton M et al (2015) Disruption of the gut microbiome: clostridium difficile infection and the threat of antibiotic resistance. Genes 6(4):1347–1360
Cammarota G, Masucci L, Ianiro G, et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther 41(9): 835–843
Staley C, Kelly CR, Brandt LJ, Khoruts A, Sadowsky MJ (2016) Complete microbiota engraftment is not essential for recovery from recurrent Clostridium difficile infection following fecal microbiota transplantation. mBio 7(6):2074–2079
Minot SS, Krumm N, Greenfield NB (2015) One codex: a sensitive and accurate data platform for genomic microbial identification. bioRxiv. https://doi.org/10.1101/027607
Karanika S, Paudel S, Grigoras C, Kalbasi A, Mylonakis E (2016) Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital-based antimicrobial stewardship programs. Antimicrob Agents Chemother 60(8):4840–4852
Hellyer TP, McAuley DF, Walsh TS et al (2019) Biomarker-guided antibiotic stewardship in suspected ventilator-associated pneumonia (VAPrapid2): a randomised controlled trial and process evaluation. Lancet Resp Med. https://doi.org/10.1016/S2213-2600(19)30367-4
Morris AC, Hay AW, Swann DG et al (2011) Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit Care Med 39(10):2218–2224
Gadsby NJ, Russell CD, McHugh MP et al (2016) Comprehensive molecular testing for respiratory pathogens in community-acquired pneumonia. Clin Infect Dis 62(7):817–823
Chiu CY, Miller SA (2019) Clinical metagenomics. Nature Rev Genet 20(6):341–355
Weng H, Li J-G, Mao Z et al (2017) Probiotics for preventing ventilator-associated pneumonia in mechanically ventilated patients: a meta-analysis with trial sequential analysis. Front Pharmacol 8:S17–S36
Wheeler KE, Cook DJ, Mehta S et al (2016) Use of probiotics to prevent ventilator-associated pneumonia: a survey of pharmacists' attitudes. J Crit Care 31(1):221–226
De Filipp Z, Bloom PP, Torres Soto M et al (2019) Drug-resistant E coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med 381(21):2043–2050
Yelin I, Flett KB, Merakou C et al (2019) Genomic and epidemiological evidence of bacterial transmission from probiotic capsule to blood in ICU patients. Nat Med 25:1728–1732
Acknowledgement
We are grateful to Rudma Tek Pty Ltd and Phillip M Ball for their assistance with the illustrations for this article.
Funding
ACM is supported by a Clinical Research Career Development Fellowship from the Wellcome Trust (WT 2055214/Z/16/Z).
Author information
Authors and Affiliations
Contributions
NA reviewed and appraised the literature, drafted and revised the manuscript and approves the final version. MR reviewed and appraised the literature, drafted and revised the manuscript and approves the final version. SS reviewed and appraised the literature, drafted and revised the manuscript and approves the final version. JL conceived the article, reviewed and appraised the literature, revised the manuscript and approves the final version. ACM conceived the article, reviewed and appraised the literature, drafted and revised the manuscript and approves the final version.
Corresponding author
Ethics declarations
Conflicts of interest
JL has received honoraria from Pfizer and MSD. All other authors declare that they have no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arulkumaran, N., Routledge, M., Schlebusch, S. et al. Antimicrobial-associated harm in critical care: a narrative review. Intensive Care Med 46, 225–235 (2020). https://doi.org/10.1007/s00134-020-05929-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-05929-3