Abstract
There is an ongoing discussion whether hyperoxia, i.e. ventilation with high inspiratory O2 concentrations (FIO2), and the consecutive hyperoxaemia, i.e. supraphysiological arterial O2 tensions (PaO2), have a place during the acute management of circulatory shock. This concept is based on experimental evidence that hyperoxaemia may contribute to the compensation of the imbalance between O2 supply and requirements. However, despite still being common practice, its use is limited due to possible oxygen toxicity resulting from the increased formation of reactive oxygen species (ROS) limits, especially under conditions of ischaemia/reperfusion. Several studies have reported that there is a U-shaped relation between PaO2 and mortality/morbidity in ICU patients. Interestingly, these mostly retrospective studies found that the lowest mortality coincided with PaO2 ~ 150 mmHg during the first 24 h of ICU stay, i.e. supraphysiological PaO2 levels. Most of the recent large-scale retrospective analyses studied general ICU populations, but there are major differences according to the underlying pathology studied as well as whether medical or surgical patients are concerned. Therefore, as far as possible from the data reported, we focus on the need of mechanical ventilation as well as the distinction between the absence or presence of circulatory shock. There seems to be no ideal target PaO2 except for avoiding prolonged exposure (> 24 h) to either hypoxaemia (PaO2 < 55–60 mmHg) or supraphysiological (PaO2 > 100 mmHg). Moreover, the need for mechanical ventilation, absence or presence of circulatory shock and/or the aetiology of tissue dysoxia, i.e. whether it is mainly due to impaired macro- and/or microcirculatory O2 transport and/or disturbed cellular O2 utilization, may determine whether any degree of hyperoxaemia causes deleterious side effects.
Similar content being viewed by others
Background
Oxygen (O2) is not only the final electron acceptor within the respiratory chain, but also one of the strongest oxidizing molecules [1, 2]. Approximately 1–3% of mitochondrial O2 consumption is directed towards the production of "reactive oxygen species" (ROS), i.e. the more ATP produced, the more ROS are generated [3, 4]. ROS formation is directly related to the O2 concentration [5], so that hyperoxia (i.e. breathing inspiratory O2 concentrations FIO2 > 0.21) and the consecutive hyperoxaemia (i.e. arterial PO2 > 100 mmHg) result in a dose-dependent increase of ROS formation [6, 7]. It is noteworthy in this context that the definition of hyperox(aem)ia may vary as well: while some authors use a threshold PaO2 value of 150 mmHg [8, 9], others refer to hyperox(aem)ia as PaO2 ≥ 300 mmHg [10,11,12,13,14]. The aggravated ROS formation resulting from increased O2 concentrations is particularly pronounced during ischaemia/reperfusion (I/R) and/or hypoxia/re-oxygenation [5]. Nevertheless, the dichotomy for O2 holds also true for ROS formation, in that despite their toxic potential ROS are vital players in host defence systems and as signalling molecules [15].
In line with the potential toxicity of increased ROS formation resulting from supplemental O2 administration, a meta-analysis of more than 16,000 patients previously concluded that patients with "liberal" oxygenation (defined as transcutaneous, pulse oximetry haemoglobin–O2 saturation [SpO2] median/range 96/94–99%) "had a dose-dependent increased risk of … mortality", yet found "no significant difference in disability, hospital-acquired pneumonia, or length of hospital stay" [16]. While providing robust data on a large general ICU population, only 8 out 25 studies analysed in this systematic review, however, had included patients undergoing mechanical ventilation. Moreover, the putative impact of the presence or absence of circulatory shock was not discussed at all. Finally, due to the scarcity of the literature available, a conclusive evaluation of some conditions normally necessitating ICU treatment could not be provided either, e.g. trauma-and-haemorrhage and/or traumatic brain injury [16]. Nevertheless, based on this meta-analysis, an expert panel concluded on a "strong recommendation" that when supplemental O2 therapy is used, SpO2 > 96% should be avoided in all in-hospital as well as prehospital medical patients. Explicitly, uncomplicated, elective surgical patients were not included because the expert panel had not reviewed the issue of peri-operative hyperoxia and surgical site infection, respectively [17].
On the other hand, more recently, in a population of mechanically ventilated ICU patients, a "conservative" oxygenation target (defined as SpO2 < 97%) yielded no benefit when compared to a "usual" oxygenation group [18], and even suggested that "usual (liberal) oxygen therapy might be preferred" in the subgroup of patients with sepsis [19]. Therefore, given the U-shaped relation between mortality/morbidity and PaO2 [20], this mini-review will discuss the questions i) whether there is an "ideal" PaO2 for ICU patients, and in particular; ii) if present, whether it possibly differs according to the underlying pathology. We will only discuss the available clinical data, since the vast majority of experimental models lack standard ICU care, which necessarily limits their translational value. Moreover, as far as possible from the data reported, we will focus on data from mechanically ventilated vs. spontaneously breathing patients. Finally, we will try to evaluate the possible impact of the presence or absence of circulatory shock, a condition where "administration of oxygen should be started immediately to increase oxygen delivery" [21]. This review will discuss pertinent clinical studies on general ICU populations and in the emergency department (ED), acute respiratory distress syndrome (ARDS), sepsis and septic shock, trauma and haemorrhage, traumatic brain injury, cardiopulmonary resuscitation (CPR) and post-cardiac management, and peri-operative hyperoxia. Last, the role of SpO2 vs. PaO2 measurements for the monitoring of oxygenation will be addressed.
General ICU and emergency department (ED) populations
A retrospective multicentre analysis of patients with an ICU stay > 24 h showed that the "hyperoxaemia dose", defined as the time integral of supraphysiological PaO2 (> 100 mmHg) was associated with mortality in ICU patients. Interestingly, however, no dose–response relationship could be established [22]. In line with these findings, a retrospective analysis of more than 25,000 mechanically ventilated ICU patients found that the proportion of time spent at 95 ≤ SpO2 ≤ 99% was associated with the lowest odds ratio for mortality, while both SpO2 ≤ 94 and = 100% coincided with increased mortality [23]. Similarly, an observational study analysing large ICU data bases of a total of 35,287 patients identified 94 ≤ SpO2 ≤ 98% as the optimal range with respect to survival [24]. In fact, targeting this interval, i.e. "conservative" oxygen therapy (PaO2 = 70–100 mmHg or SpO2 = 94–98%) vs. "standard" treatment (PaO2 ≤ 150 mmHg or SpO2 ≤ 98%) in a general ICU population of 434 patients with an expected length of stay of ≥ 72 h, had previously been associated with significantly reduced mortality (11.6 vs. 20.2%), de novo occurrence of shock (3.7 vs. 10.6%), liver failure (1.9 vs. 6.4%), and bacteraemia (5.1 vs. 10.1%). However, while the originally planned sample size had been 660 patients, the study was stopped early due to difficulties in enrolment after inclusion of 480 patients [25]. Moreover, only 2/3 of the patients needed mechanical ventilation, and only 30% of the patients presented with shock at inclusion [25].
However, another retrospective single-centre study in general ICU patients mechanically ventilated for at 7 days did not show any association between in-hospital mortality and time-weighted PaO2 > 120 mmHg [26]. Furthermore, other authors had even reported nadir mortality in a general ICU population at a mean PaO2 over the total ICU length of stay ≈ 120–150 mmHg, while exposure to PaO2 > 200 mmHg was indeed associated with increased mortality [27].
An observational cohort study analysed the outcome of patients and exposed to ED hyperoxia. The study included 688 out of a total of 3525 patients already mechanically ventilated in the ED, who were all normoxic (60 ≤ PaO2 ≤ 120 mmHg) on day 1 of their ICU stay. While ED normoxia was present in 50.9% of the patients, ED hyperoxia as defined as a PaO2 > 120 mmHg occurred in 43.6%. Hospital mortality at day 28 was higher in patients with ED hyperoxia (29.7%) than in those with ED normoxia (19.4%) [28]. Interestingly, survival curves of patients with ED hyperoxia and normoxia, respectively, cleaved at day 4–5 only of hospital stay, i.e. several days after normoxia had resumed.
In conclusion, in general ED and ICU populations, so far, the available clinical data do not suggest that there is any ideal target PaO2 except for avoiding prolonged exposure (> 24 h) to either hypoxemia or supraphysiological (PaO2 > 100 mmHg).
Acute respiratory distress syndrome (ARDS)
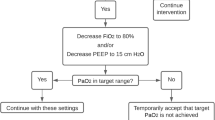
The current standard of care of patients with ARDS recommends targeting for arterial oxygenation defined as PaO2 = 65–75 mmHg and/or arterial haemoglobin O2 saturation (SaO2) = 90–95%, respectively [29]. In a secondary analysis of 2005 patients of the LUNG SAFE study, Madotto et al. reported an incidence of "hyperoxaemia" (PaO2 > 100 mm Hg) on day 1 or "sustained hyperoxaemia" (i.e. on day 1 and 2) in 30 and 12% of the patients, respectively. In 66% of these hyperoxaemic patients, "excess O2 use", i.e. an inspiratory O2 concentration FIO2 ≥ 0.6 and PaO2 > 100 mmHg, was present. The authors concluded that despite being frequently present, hyperoxaemia was mostly only transient. However, neither hyperoxaemia nor excess O2 use had any effect on patient outcome [30].
The LOCO2 trial [31] compared "conservative O2" therapy for 7 days (target PaO2 = 55–70 mm Hg and/or SaO2 as measured by pulse oximetry [SpO2] = 88–92%) to a "liberal O2" therapy arm (target PaO2 = 90–105 mm Hg and/or SpO2 ≥ 96%). Albeit the patients in the liberal O2 arm showed significantly higher PaO2 values than those in the conservative O2 group without major inter-group overlap, about half of the patients of the conservative O2 group presented with values beyond the upper target threshold of 70 mmHg. Nevertheless, during the 7 observation days, the conservative O2 group needed less controlled ventilation, lower PEEP levels, and prone positioning. In contrast, heart rate was higher in this group. However, the conservative O2 approach did not increase survival at 28 days, and the trial was prematurely stopped because of safety concerns after enrolment of 205 patients: at day 28, 34 of 99 patients (34%) in the conservative and 27 of 102 patients (26.5%) in the liberal O2 groups, respectively, had died. At day 90, mortality was even significantly higher in the conservative (44 of 99 [44%] patients) than in the liberal O2 arm (31 of 102 [30%] patients) [31].
Finally, in a total of 2,928 patients with acute hypoxemic respiratory failure, the most recent ICU-HOT trial compared a "lower" (PaO2 ≈ 60 mmHg) vs. a "higher" (PaO2 ≈ 90 mmHg) oxygenation target until 90 days after randomization [32]. More than half of the patients needed mechanical ventilation and/or vasopressor support (58 and 54%, respectively). Interestingly, in both study groups, the median/interquartile range PaO2 values were slightly higher than the target levels (71/67–77 vs. 93/87–99 mmHg, respectively). The two intervention groups did not show any difference with respect to mortality and morbidity.
In conclusion, in patients with ARDS, so far, the available clinical data do not suggest that there is any ideal target PaO2 except for avoiding prolonged exposure (> 24 h) to either hypoxemia, in particular with respect to long-term neuropsychological sequelae [33, 34], or supraphysiological (PaO2 > 100 mmHg).
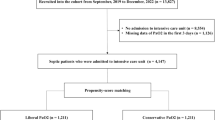
Sepsis and septic shock
Hyperoxaemia is associated with systemic vasoconstriction, i.e. might theoretically counteract vasodilation-related arterial hypotension [5], and has antibacterial potential [35]. However, in a retrospective analysis of 141 patients (out of a total enrolment of 503 patients) with ventilator-associated pneumonia (VAP), the number of days with hyperoxaemia (as defined by a PaO2 > 120 mmHg) was an independent risk factor for the occurrence of VAP, rather than suggesting any antibiotic property. It should be noted, however, that these patients also showed several other risk factors of VAP, e.g. more use of proton pump inhibitors, more frequent circulatory shock, more transfusion of packed red blood cells, and more frequent sedation [36].
The prospective, randomized, controlled HYPER2S trial [37] compared standard therapy with mechanical ventilation with 100% O2 during the first 24 h after diagnosis of septic shock. Despite a significantly lower SOFA score at day 7, the trial was prematurely stopped due to increased mortality in the treatment arm at days 28 and 90 (43 vs. 36 and 48 vs. 42%, respectively). Due to the premature stop of the trial, this increase in mortality did not reach statistical significance (p = 0.12 and 0.16, respectively) [37]. The detrimental effect of hyperoxia was further mirrored by a higher incidence of serious adverse events (85 vs. 76%, p = 0.02), in particular of ICU-acquired weakness (11 vs. 6%, p = 0.06). Of note, a post hoc analysis according to the Sepsis-3 criteria showed that the hyperoxia-related increase in mortality at day 28 was only present in patients with hyperlactataemia > 2 mmol/L (57% vs. 44%, p = 0.054), while no effect was present in patients with normal lactataemia (25 vs. 23%, p = 0.68) [38]. This finding suggests that the putative hyperoxaemia-related increase in tissue O2 availability may have led to excess ROS production and consecutive oxidative damage because of a sepsis-induced impaired cellular O2 extraction.
The above-mentioned "conservative" oxygenation target in the ICU-ROX study was not beneficial either in patients with sepsis: a post hoc analysis of the 251 patients fulfilling these criteria showed no statistically significant inter-group difference when compared to a "usual" oxygenation. Point estimates of treatment effects even consistently favoured the latter [19]. Hence, similar to ARDS, in patients with sepsis/septic shock, there seems to be no ideal target PaO2 except for avoiding prolonged exposure (> 24 h) to either hypoxemia or supraphysiological (PaO2 > 100 mmHg).
Trauma and haemorrhage
The blood loss-related reduction of O2 transport capacity and the fall in cardiac output during trauma and haemorrhage cause a tissue O2 debt, the rapid repayment of which determines outcome [39]. There is experimental evidence that during haemorrhage, the hyperoxia-related rise in PaO2 can improve microcirculatory and tissue O2 availability [40]. Moreover, lung-protective ventilation with an FIO2 = 1.0 even attenuated organ dysfunction in resuscitated, long-term large animal experiments [41, 42]. Nevertheless, clinical data remain equivocal. In 471 consecutive mechanically ventilated patients with a median injury score (ISS) of 29, Russell et al. reported that there was no association between mortality and maximum PaO2 in the first 24 h. This was true both for the overall analysis as well as in the subgroup with head trauma (n = 266) [43].
More recently, Baekgaard et al. reported on 5,912 patients of a French trauma registry (median ISS 16), 32% of whom presented with traumatic brain injury (TBI). Univariate analysis showed higher mortality (12 vs. 9%, p < 0.0001) in patients with hyperoxaemia as defined by PaO2 > 150 mmHg upon admission (43% of the population). However, propensity score matching for gender, age, prehospital heart rate and systolic blood pressure, temperature, haemoglobin and arterial lactate concentration, use of mechanical ventilation, presence of traumatic brain, initial Glasgow Coma Scale (GCS) score, ISS, American Society of Anesthesiologists physical health class > I, and presence of haemorrhagic shock yielded just the opposite result, i.e. hyperoxaemia was associated with even lower mortality [8]. Most recently, a large retrospective, propensity-matched, data analysis of a total of 864,340 trauma patients (median ISS = 9) investigated the possible association between supplemental O2 administration in the ED and in-hospital mortality and development of ARDS. In all three patient categories as predefined according to SpO2 < 94%, 94 ≤ SpO2 ≤ 97%, and SpO2 > 97%, respectively, supplemental O2 was associated with a significantly increased odds ratio of both mortality and incidence of ARDS, no matter the presence or absence of TBI [44]. Unfortunately, the authors did not provide information on the presence of circulatory shock nor the need for mechanical ventilation. Finally, a post hoc analysis of the Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis and Trauma (FORECAST) on 240 patients with ISS ≥ 16 studied the impact of hyperoxaemia during resuscitation (defined as PaO2 of ≥ 300 mmHg on hospital arrival and/or 3 h after arrival). The results highlighted the importance of the need for mechanical ventilation and/or the presence/absence of circulatory shock: hyperoxaemia was associated with prolonged ICU sty in patients not intubated in the ED, while no effect was present in mechanically ventilated patients [45]. Of note, unadjusted baseline characteristics not only showed a higher proportion of mechanically ventilated patients, but also significantly lower GCS (6 vs. 14) as well as more frequent need craniotomy and transfusion of blood products in the hyperoxaemic group [45].
Consequently, despite being common practice in daily care, in particular in patients with pronounced blood loss, so far, no specific target for PaO2 is available.
Traumatic brain injury
Two opposing statements ("…The emerging clinical experience demonstrates that hyperoxia is safe and beneficial to the brain…" [46] and "…Hyperoxia may be associated with increased mortality in patients with … traumatic brain injury…" [47]) highlight the discussion on the impact of supraphysiological PaO2 in TBI patients during the last decade. This controversy is further mirrored by the results of three clinical studies: In 193 TBI patients (40% with polytrauma) with a GCS of 4 ± 2, Asher et al. reported that maximum values of 250 < PaO2 < 450 mmHg during the first 72 h were associated with improved outcome [48]. In contrast, Rincon et al. reported in 1,212 mechanically ventilated TBI patients (57% with a GCS < 8) that PaO2 ≥ 300 mmHg during the first 24 h significantly increased mortality when compared to 60 ≤ PaO2 < 300 mmHg (33% vs. 23%) [13]. Finally, Raj et al. reporting on 1,116 moderate-to-severe (GCS 3–12) patients with TBI concluded that a PaO2 > 100 mmHg within the first 24 h of ICU admission had no predictive value for 6-month mortality [49].
Theoretically, hyperoxaemia may exert beneficial effects during the acute management of traumatic brain injury (TBI) as a result of the above-mentioned vasoconstriction, which would allow for reducing intracranial pressure without compromising tissue oxygenation. This potentially beneficial effect has been demonstrated in severe TBI patients (n = 42, mean GCS = 5.7) undergoing a combined hyperbaric oxygen (HBO) and normobaric (NBO) oxygen treatment. Ultimately, this approach not only significantly reduced mortality, but also improved neurological outcome at 6 months post injury as assessed using the Glasgow Outcome Scale-Extended (GOSE) [50].
In the context of the above-discussed hyperoxaemia-related increase of systemic O2 transport capacity, hyperoxaemia may be particularly important when TBI coincides with haemorrhage. Nevertheless, the existing data of the two existing prospective clinical studies again are equivocal: Taher et al. compared the effects of 6 h of FIO2 = 0.8 and 0.5 early after injury in 68 mechanically ventilated TBI patients with a GCS of 4 ± 2, demonstrating a tendency towards improved neurological outcome at 6 months [51]. However, the generalizability of the findings is limited, since patients with chronic co-morbidity, > 65 years of age, and, in particular, arterial hypotension were excluded.
The BRAINOXY [52] trial investigated the effect of FIO2 = 0.7 vs. 0.4 in 62 TBI patients (both isolated TBI and TBI in the context of polytrauma) during the time of mechanical ventilation (up to 14 days). As expected, the higher FIO2 was associated with nearly twice as high PaO2 levels during the observation period, but there was no inter-group difference for markers of oxidative stress, inflammation, neurological injury and/or pulmonary complications [52].
Large scale, retrospective studies provided comparably equivocal results: O’Briain et al. reported in > 24,000 mechanically ventilated TBI patients that hyperoxaemia (in PaO2 category increments up to > 500 mm Hg) during the first 24 h in the ICU did not affect mortality irrespective of the GCS at admission [53]. In contrast, a post hoc analysis of 417 of the 1213 patients of the Citicoline Brain Injury Treatment Trial (COBRIT) showed that 150 < PaO2 < 250 mmHg (referred to by the authors as "mild" hyperoxaemia) within the first 24 h after injury was associated with significantly lower mortality and, in particular, a better GOSE score and overall long-term functional and cognitive outcomes [9]. This possibly beneficial effect was also suggested by a retrospective study in 115 patients with severe TBI, which assessed the possible relation between PaO2 and cerebral metabolism as well as pressure-flow autoregulation using cerebral microdialysis and the pressure reactivity index, respectively. The authors concluded that a PaO2 "…above 90 mmHg and higher may improve oxidative cerebral energy metabolism and pressure autoregulation, particularly in cases of limited energy substrate supply in the early phase of TBI…". However, there was no significant relationship between PaO2 and clinical outcome as assessed using the GOSE [54].
In conclusion, it seems to be unequivocal that hyperoxaemia should be avoided after acute brain injury resulting from ischaemia [13] as well as subarachnoid [55] and/or intracerebral bleeding: Because of the vasoconstrictor properties of O2 [5] there is a consecutive risk of vasospasm-induced delayed cerebral ischaemia [56, 57]. Given the above-mentioned controversial results reported on TBI, the current knowledge on a possible PaO2 target in these patients is best characterized by the statements that—with respect to any possible neuroprotective properties of hyperox(aem)ia—there "… is probably a narrow effective dose, and benefit may be limited to at-risk tissue…" [58], and the conclusion that there is the " … need to identify optimal approaches to improve O2 delivery without exacerbating … oxidative stress or injury…" [59].
Cardiopulmonary resuscitation (CPR) and post-cardiac management
CPR represents whole-body I/R injury, and clearly, two phases of CPR have to be differentiated, i.e. the period of active cardiopulmonary resuscitation, and the post-resuscitation phase, which starts after return of spontaneous circulation (ROSC). For obvious reasons, studies on the impact of hyperox(aem)ia during the former are scarce given the common practice of ventilation with 100% O2 during CPR, but the available data suggest that there is a "dose-dependent" successful incidence of ROSC with incremental PaO2 values [60, 61].
The post-resuscitation phase has been thoroughly investigated during the last decade. Two large-scale retrospective American and Australian studies including 6,326 and 12,108 patients, respectively, found equivocal impact of arterial oxygenation on outcome after cardiac arrest. In the American study [10], hyperoxaemia (PaO2 ≥ 300 mmHg during the first of 24 ICU hours after ROSC) was associated with a significant, dose-dependent increase of mortality and worsening of neurological outcome for any 100 mmHg rise in PaO2 [62]). In contrast, in the Australian study, it did not "have a robust or consistently reproducible association with mortality" [11]. Similar deleterious effects of hyperoxaemia as defined by PaO2 > 300 mmHg have been reported by others in retrospective analyses of a total of 1,448 patients [14, 63,64,65]. Of note, one of these studies concluded that the "…optimal range of PaO2 for favourable neurological outcome…" could be a PaO2 interval of 70 < PaO2 < 240 mmHg [64]. In addition, in the other study, "moderate hyperoxia" (101 < PaO2 < 299 mmHg) according to the authors’ definition was even associated with improved organ function at 24 h [65]. Finally, in 5,258 patients after ROSC, Helmerhorst et al. had observed a similar U-shaped relation between mortality and the maximum PaO2 during the first 24 h in the ICU [66] as in the above-discussed general ICU population, the nadir mortality coinciding with a PaO2 ≈ 150–200 mmHg.
The most recent data confirm these conflicting results: In a prospective observational study on 280 patients Roberts et al. [67] concluded that PaO2 > 300 mmHg during the initial 6 h after ROSC was independently associated with death and poor neurological function. Moreover, any one-hour longer duration of hyperoxaemia was associated with a 3% increase in risk of poor outcome. In contrast, a post hoc sub-study of the Target Temperature Management (TTM) trial, including 939 patients after out-of-hospital-cardiac arrest, did not find any significant relation between hyperoxaemia (defined as PaO2 > 300 mmHg) within 37 h of ROSC and poor neurological outcome after 6 months [68]. Finally, an additional post hoc analysis of the above-mentioned ICU-ROX study including 161 patients with "suspected hypoxic–ischaemic encephalopathy" after cardiac arrest, a subgroup pre-specified and defined prior to randomization, did not show a statistically significant reduction in death or unfavourable neurological outcomes at day 180 [69]. This finding was in contrast to the analysis of the complete GOSE, which had suggested benefit of the "conservative oxygen" treatment and yielded significantly lower mortality at day 180 in the unadjusted analysis [18].
Again, as already suggested for ARDS, sepsis and septic shock, there seems to be no ideal target PaO2 for ROSC after CPR.
Peri-operative hyperoxia
Despite the recommendations of the World Health organization from 2016 [70] and subsequently by the US Centers for Disease Control in 2017 [71], the question whether or not there is evidence for the use of peri-operative hyperoxia to reduce surgical site infections remains a matter of debate. In line with previous ones [72, 73], the most recent meta-analysis on 17 RCT including 7,817 patients identified a weak signal (Odds ratio 0.80, confidence interval 0.64–0.99) favouring peri-operative hyperoxia in patients undergoing general anaesthesia with endotracheal intubation [74]. No effect was found in the overall analysis. Other authors cautioned this conclusion [75] or even could not confirm this result when analysis "…was restricted to objective- or investigator-identified low-bias studies, although those analyses were not as well-powered" [76]. Moreover, several concerns have to be raised concerning these recommendations. Most trials investigating the putative impact of peri-operative hyperoxia on surgical site infection compared FIO2 = 80% with FIO2 = 30%), which would yield a PaO2 ≈ 350–400 mmHg vs. PaO2 ≈ 120–150 mmHg, respectively, in patients without major acute or chronic cardiopulmonary disease. However, at least some observations reported standard daily practice frequently using FIO2 ≈ 40—60% [77, 78]. Finally, even if present, any beneficial effect of peri-operative hyperoxia on the incidence of surgical site infections has to be weighed by potential harm, e.g. pulmonary and/or cardiovascular complications as well as new or recurrent cancer [79,80,81,82,83]. In fact, the largest available study in this context on almost 74,000 patients, showed a dose-dependent increase in major post-operative respiratory complications and ultimately 30-day mortality of intra-operative FIO2 increments (median FIO2 = 0.3, = 0.41, = 0.52, = 0.58, and = 0.79, respectively) [84].
Hence, albeit a recent review article conjected "…that current evidence is in favour of hyperoxia in noncritically ill intubated adult surgical patients…" [85], peri-operative hyperoxia (and even the possible consecutively enhanced host-defence resulting from increased ROS formation [86]) remains an open question, because the "good", "bad", and "ugly" [87] of its use are still not fully understood.
SpO2 vs. PaO2 measurement for monitoring of oxygenation
As described in detail above, there is no ideal PaO2 target for critically ill patients so far, no matter the underlying aetiology. Hence, both hyperoxaemia (i.e. supraphysiological PaO2) and, more importantly, due to its short and long-term consequences, hypoxemia (i.e. PaO2 < 55–60 mmHg) should be avoided. For daily practice, this raises the question whether SpO2 suffices as a surrogate for PaO2. Hyperoxaemia and hypoxemia can be defined as PaO2 > 100 and < 55–60 mmHg, respectively. However, due to the sigmoid haemoglobin–O2 dissociation curve and its dependency on pH, PCO2, temperature, and erythrocyte 2,3-diphosphoglycerate concentration, the PaO2–SaO2 relation may vary. Moreover, frequently the available SpO2 devices cannot take into account increased met- or carboxy(CO)-haemoglobin levels or the interference of jaundice, because measurements are based on two wavelengths only. Hence, even normal SpO2 readings of 94% cannot exclude hypoxemia with PaO2 < 60 mmHg [88]. This is particularly important in the most severe patients, when vasoactive drugs must be used [89, 90]. To avoid the risk of hypoxaemia, and taking in account both the potential discrepancies between SpO2 and SaO2 as well as the above-discussed data, targeting 95 ≤ SpO2 ≤ 98% appears to be reasonably safe when PaO2 and/or SaO2 measurements are not available.
Conclusion
Several authors reported that in ICU patients there is a U-shaped relation between PaO2 and mortality/morbidity. Interestingly, these mostly retrospective studies found that the lowest mortality was present at PaO2 ~ 150 mm Hg. Nevertheless, such supraphysiological PaO2 values cannot be recommended in general, since the absence or presence of circulatory shock and/or the aetiology of tissue dysoxia, i.e. whether it is mainly due to impaired (macro- and/or microcirculatory) O2 transport and/or disturbed cellular O2 utilization may determine whether any supraphysiological PaO2 level is really beneficial and/or even causes deleterious side effects.
Availability of data and materials
Not applicable.
Change history
28 October 2021
The open access funding note was missing from this article and should have read ‘’Open Access funding enabled and organized by Projekt DEAL’’.
Abbreviations
- O2 :
-
Oxygen
- FIO2 :
-
Inspiratory O2 concentration
- PaO2 :
-
Arterial O2 tension
- ROS:
-
Reactive oxygen species
- I/R:
-
Ischaemia/reperfusion
- ATP:
-
Adenosine triphosphate
- ICU:
-
Intensive care unit
- SpO2 :
-
Pulse oximetry haemoglobin O2 saturation
- ED:
-
Emergency department
- ARDS:
-
Acute respiratory distress syndrome
- TBI:
-
Traumatic brain injury
- CPR:
-
Cardiopulmonary resuscitation
- SaO2 :
-
Arterial haemoglobin O2 saturation
- VAP:
-
Ventilator-associated pneumonia
- SOFA:
-
Sequential organ failure assessment
- ISS:
-
Injury severity score
- HBO:
-
Hyperbaric oxygen
- NBO:
-
Normobaric
- GCS:
-
Glasgow Coma Scale
- GOSE:
-
Glasgow Outcome Scale-Extended
- ROSC:
-
Return of spontaneous circulation
- RCT:
-
Randomized controlled trial
References
Asfar P, Singer M, Radermacher P. Understanding the benefits and harms of oxygen therapy. Intensive Care Med. 2015;41(6):1118–21.
Leverve XM. To cope with oxygen: a long and still tumultuous story for life. Crit Care Med. 2008;36(2):637–8.
Turrens J. Mitochondrial formation of reactive oxygen species. J Physiol. 2003;552(Pt 2):335–44.
Jamieson D, Chance B, Cadenas E, Boveris A. The relation of free radical production to hyperoxia. Annu Rev Physiol. 1986;48:703–19.
Hafner S, Beloncle F, Koch A, Radermacher P, Asfar P. Hyperoxia in intensive care, emergency, and peri-operative medicine: Dr. Jekyll or Mr. Hyde? A 2015 update. Ann Intensive Care 2015;5(1):42.
Khaw KS, Wang CC, Ngan Kee WD, Pang CP, Rogers MS. Effects of high inspired oxygen fraction during elective caesarean section under spinal anaesthesia on maternal and fetal oxygenation and lipid peroxidation. Br J Anaesth. 2002;88(1):18–23.
Hafner C, Pramhas S, Schaubmayr W, Assinger A, Gleiss A, Tretter EV, et al. Brief high oxygen concentration induces oxidative stress in leukocytes and platelets - a randomised cross-over pilot study in healthy male volunteers. Shock. 2021. https://doi.org/10.1097/SHK.0000000000001728.
Baekgaard J, Abback PS, Boubaya M, Moyer JD, Garrigue D, Raux M, et al. Early hyperoxemia is associated with lower adjusted mortality after severe trauma: Results from a French registry. Crit Care. 2020;24(1):604.
Alali AS, Temkin N, Vavilala MS, Lele AV, Barber J, Dikmen S, et al. Matching early arterial oxygenation to long-term outcome in severe traumatic brain injury: target values. J Neurosurg. 2019;132(2):537–44.
Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165–71.
Bellomo R, Bailey M, Eastwood GM, Nichol A, Pilcher D, Hart GK, et al. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care. 2011;15(2):R90.
Rincon F, Kang J, Vibbert M, Urtecho J, Athar MK, Jallo J. Significance of arterial hyperoxia and relationship with case fatality in traumatic brain injury: a multicentre cohort study. J Neurol Neurosurg Psychiatry. 2014;85(7):799–805.
Rincon F, Kang J, Maltenfort M, Urtecho J, Athar MK, et al. Association between hyperoxia and mortality after stroke: a multicenter cohort study. Crit Care Med. 2014;42(2):387–96.
Johnson NJ, Dodampahala K, Rosselot B, Perman SM, Mikkelsen ME, Goyal M, et al. The association between arterial oxygen tension and neurological outcome after cardiac arrest. Ther Hypothermia Temp Manag. 2017;7(1):36–41.
Magder S. Reactive oxygen species: toxic molecules or spark of life? Crit Care. 2006;10(1):208.
Chu DK, Kim LHY, Young PJ, Zamiri N, Almenawer SA, Jaeschke R, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (iota): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–705.
Siemieniuk RAC, Chu DK, Kim LH, Güell-Rous MR, Alhazzani W, Soccal PM, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ. 2018;363:k4169.
ICU-ROX Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, Eastwood G, Finfer S, Freebairn R, King V, Linke N, et al. Conservative Oxygen Therapy during Mechanical Ventilation in the ICU. N Engl J Med. 2020;382(11):989–98.
Young P, Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, et al, ICU-ROX Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Conservative oxygen therapy for mechanically ventilated adults with sepsis: a post hoc analysis of data from the intensive care unit randomized trial comparing two approaches to oxygen therapy (ICU-ROX). Intensive Care Med 2020;46(1):17–26.
Vincent Jl, Taccone FS, He X. Harmful Effects of Hyperoxia in Postcardiac Arrest, Sepsis, Traumatic Brain Injury, or Stroke: The Importance of Individualized Oxygen Therapy in Critically Ill Patients. Can Respir J 2017;2017:2834956.
Vincent JL, De Backer D. Circulatory Shock. N Engl J Med. 2013;369(18):1726–34.
Palmer E, Post B, Klapaukh R, Marra G, Macallum NS, Brealey D, et al. The Association between Supraphysiologic Arterial Oxygen Levels and Mortality in Critically Ill Patients. A Multicenter Observational Cohort Study. Am J Respir Crit Care Med. 2019;200(11):1373–80.
Zhou D, Li Z, Shi G, Zhou J. Time spent in oxygen saturation 95–99% is associated with reduced mortality in critically ill patients with mechanical ventilation. Crit Care. 2020;24:414.
van den Boom W, Hoy M, Sankaran J, Liu M, Chahed H, Feng M, See KC. The search for optimal oxygen saturation targets in critically ill patients: observational data from large ICU Databases. Chest. 2020;157(3):566–73.
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU Randomized Clinical Trial. JAMA. 2016;316(15):1583–9.
Kraft F, Andel H, Gamper J, Markstaller K, Ullrich R, Klein KU. Incidence of hyperoxia and related in-hospital mortality in critically ill patients: a retrospective data analysis. Acta Anaesthesiol Scand. 2018;62(3):347–56.
Helmerhorst HJF, Arts DL, Schultz MJ, van der Voort PHJ, Abu-Hanna A, de Jonge E, et al. Metrics of Arterial Hyperoxia and Associated Outcomes in Critical Care. Crit Care Med. 2017;45(2):187–95.
Page D, Ablordeppey E, Wessman BT, Mohr NM, Trzeciak S, Kollef MH, et al. Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study. Crit Care. 2018;22(1):9.
Bein T, Grasso S, Moerer O, Quintel M, Guerin C, Deja M, et al. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Med. 2016;42(5):699–711.
Madotto F, Rezoagli E, Pham T, Schmidt M, McNicholas B, Protti A, et al. Hyperoxemia and excess oxygen use in early acute respiratory distress syndrome: insights from the LUNG SAFE study. Crit Care. 2020;24(1):12.
Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382(11):999–1008.
Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, et al. HOT-ICU Investigators. Lower or higher oxygenation targets for acute hypoxemic respiratory failure. N Engl J Med 2021;384:1301–11.
Hopkins RO, Weaver LK, Pope D, Orme JF, Bigler ED, Larson-Lohr V. Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 1999;160(1):50–6.
Mikkelsen ME, Christie JD, Lanken PN, Biester RC, Thompson BT, Bellamy SL, et al. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185(12):1307–15.
Knighton DR, Halliday B, Hunt TK. Oxygen as an antibiotic The effect of inspired oxygen on infection. Arch Surg. 1984;119(2):199–204.
Six S, Jaffal K, Ledoux G, Jaillette E, Wallet F, Nseir S. Hyperoxemia as a risk factor for ventilator-associated pneumonia. Crit Care. 2016;20(1):195.
Asfar P, Schortgen F, Boisramé-Helms J, Charpentier J, Guérot E, Megarbane B, et al. Hyperoxia and hypertonic saline in patients with septic shock (HYPERS2S): a two-by-two factorial, multicentre, randomised, clinical trial. Lancet Respir Med. 2017;5(3):180–90.
Demiselle J, Wepler M, Hartmann C, Radermacher P, Schortgen F, Meziani F, et al. Hyperoxia toxicity in septic shock patients according to the Sepsis-3 criteria: a post hoc analysis of the HYPER2S trial. Ann Intensive Care. 2018;8(1):90.
Barbee RW, Reynolds PS, Ward KR. Assessing shock resuscitation strategies by oxygen debt repayment. Shock. 2010;33(2):113–22.
Dyson A, Simon F, Seifritz A, Zimmerling O, Matallo J, Calzia E, et al. Bladder tissue oxygen tension monitoring in pigs subjected to a range of cardiorespiratory and pharmacological challenges. Intensive Care Med. 2012;38(11):1868–76.
Knöller E, Stenzel T, Broeskamp F, Hornung R, Scheuerle A, McCook O, et al. Effects of hyperoxia and mild therapeutic hypothermia during resuscitation from porcine hemorrhagic shock. Crit Care Med. 2016;44:e264–77.
Hartmann C, Loconte M, Antonucci E, Holzhauser M, Hölle T, Katzsch D, et al. Effects of Hyperoxia During Resuscitation From Hemorrhagic Shock in Swine With Preexisting Coronary Artery Disease. Crit Care Med. 2017;45(12):e1270–9.
Russell DW, Janz DR, Emerson WL, May AK, Bernard GR, Zhao Z, et al. Early exposure to hyperoxia and mortality in critically ill patients with severe traumatic injuries. BMC Pulm Med. 2017;17(1):29.
Christensen MA, Steinmetz J, Velmahos G, Rasmussen LS. Supplemental oxygen therapy in trauma patients: an exploratory registry-based study. Acta Anaesthesiol Scand. 2021. https://doi.org/10.1111/aas.13829.
Yamamoto R, Fujishima S, Sasaki J, Gando S, Saitoh D, Shiraishi A, et al; Japanese Association for Acute Medicine (JAAM) Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis and Trauma (FORECAST) Study Group. Hyperoxemia during resuscitation of trauma patients and increased intensive care unit length of stay: inverse probability of treatment weighting analysis. World J Emerg Surg 2021;16(1):19.
Narotam PK. Eubaric hyperoxia: controversies in the management of acute traumatic brain injury. Crit Care. 2013;17(5):197.
Damiani E, Adrario E, Girardis M, Romano R, Pelaia P, Singer M, et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Crit Care. 2014;18(6):711.
Asher SR, Curry P, Sharma D, Wang J, O’Keefe GE, Daniel-Johnson J, Vavilala MS. Survival advantage and PaO2 threshold in severe traumatic brain injury. J Neurosurg Anesthesiol. 2013;25(2):168–73.
Raj R, Bendel S, Reinikainen M, Kivisaari R, Siironen J, Lång M, et al. Hyperoxemia and long-term outcome after traumatic brain injury. Crit Care. 2013;17(4):R177.
Rockswold SB, Rockswold GL, Zaun DA, Liu J. A prospective, randomized Phase II clinical trial to evaluate the effect of combined hyperbaric and normobaric hyperoxia on cerebral metabolism, intracranial pressure, oxygen toxicity, and clinical outcome in severe traumatic brain injury. J Neurosurg. 2013;118(6):1317–28.
Taher A, Pilehvari Z, Poorolajal J, Aghajanloo M. Effects of normobaric hyperoxia in traumatic brain injury: a randomized controlled clinical trial. Trauma Mon. 2016;21(1):e26772.
Lång M, Skrifvars MB, Siironen J, Tanskanen P, Ala-Peijari M, Koivisto T, et al. A pilot study of hyperoxemia on neurological injury, inflammation and oxidative stress. Acta Anaesthesiol Scand. 2018;62(6):801–10.
O’Briain D, Nickson C, Pilcher DV, Udy AA. Early hyperoxia in patients with traumatic brain injury admitted to intensive care in Australia and New Zealand: a retrospective multicenter cohort study. Neurocrit Care. 2018;29(3):443–51.
Wettervik TS, Engquist H, Howells T, Lenell S, Rostami E, Hillered L, et al. Arterial oxygenation in traumatic brain injury-relation to cerebral energy metabolism, autoregulation, and clinical outcome. J Intensive Care Med. 2020;27:885066620944097.
Yokoyama S, Hifumi T, Kawakita K, Tamiya T, Minamino M, Kuroda Y. Early hyperoxia in the intensive care unit is significantly associated with unfavorable neurological outcomes in patients with mild-to-moderate aneurysmal subarachnoid hemorrhage. Shock. 2019;51(5):593–8.
Jeon SB, Choi HA, Badjatia N, Schmidt JM, Lantigua H, Claassen J, et al. Hyperoxia may be related to delayed cerebral ischemia and poor outcome after subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2014;85(12):1301–7.
Fukuda S, Koga Y, Fujita M, Suehiro E, Kaneda K, Oda Y, et al. Hyperoxemia during the hyperacute phase of aneurysmal subarachnoid hemorrhage is associated with delayed cerebral ischemia and poor outcome: a retrospective observational study. J Neurosurg. 2021;134(1):25–32.
Stocchetti N, Taccone FS, Citerio G, Pepe PE, Le Roux PD, Oddo M, et al. Neuroprotection in acute brain injury: an up-to-date review. Crit Care. 2015;19(1):186.
Kochanek PM, Bayır H. Titrating the dose of oxygen after severe traumatic brain injury in the era of precision medicine. J Neurotrauma. 2017;34(22):3067–9.
Spindelboeck W, Schindler O, Moser A, Hausler F, Wallner S, Strasser C, et al. Increasing arterial oxygen partial pressure during cardiopulmonary resuscitation is associated with improved rates of hospital admission. Resuscitation. 2013;84(6):770–5.
Spindelboeck W, Gemes G, Strasser C, Toescher K, Kores B, Metnitz P, et al. Arterial blood gases during and their dynamic changes after cardiopulmonary resuscitation: a prospective clinical study. Resuscitation. 2016;106:24–9.
Kilgannon JH, Jones AE, Parrillo JE, Dellinger RP, Milcarek B, Hunter K, et al. Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest. Circulation. 2011;123(23):2717–22.
Janz DR, Hollenbeck RD, Pollock JS, McPherson JA, Rice TW. Hyperoxia is associated with increased mortality in patients treated with mild therapeutic hypothermia after sudden cardiac arrest. Crit Care Med. 2012;40(12):3135–9.
Wang CH, Huang CH, Chang WT, Tsai MS, Lu TC, Yu PH, et al. Association between early arterial blood gas tensions and neurological outcome in adult patients following in-hospital cardiac arrest. Resuscitation. 2015;89:1–7.
Elmer J, Scutella M, Pullalarevu R, Wang B, Vaghasia N, Trzeciak S, et al. The association between hyperoxia and patient outcomes after cardiac arrest: analysis of a high-resolution database. Intensive Care Med. 2015;41(1):49–57.
Helmerhorst HJ, Roos-Blom MJ, van Westerloo DJ, Abu-Hanna A, de Keizer NF, de Jonge E. Associations of arterial carbon dioxide and arterial oxygen concentrations with hospital mortality after resuscitation from cardiac arrest. Crit Care. 2015;19:348.
Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Pierce L, Donnino M, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: prospective multicenter protocol-directed cohort study. Circulation. 2018;137(20):2114–24.
Ebner F, Ullén S, Åneman A, Cronberg T, Mattsson N, Friberg H, et al. Associations Between Partial Pressure of Oxygen and Neurological Outcome in Out-Of-Hospital Cardiac Arrest Patients: An Explorative Analysis of a Randomized Trial. Crit Care. 2019;23(1):30.
Young P, Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, et al. ICU-ROX Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group Conservative oxygen therapy for mechanically ventilated adults with suspected hypoxic ischaemic encephalopathy. Intensive Care Med. 2020;46(12):2411–22.
Allegranzi B, Zayed B, Bischoff P, Kubilay NZ, de Jonge S, de Vries F, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e288-303.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–91.
Hovaguimian F, Lysakowski C, Elia N, Tramèr MR. Effect of intraoperative high inspired oxygen fraction on surgical site infection, postoperative nausea and vomiting, and pulmonary function: systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2013;119(2):303–16.
Yang W, Liu Y, Zhang Y, Zhao QH, He SF. Effect of intra-operative high inspired oxygen fraction on surgical site infection: a meta-analysis of randomized controlled trials. J Hosp Infect. 2016;93(4):329–38.
de Jonge S, Egger M, Latif A, Loke YK, Berenholtz S, Boermeester M, et al. Effectiveness of 80% vs 30–35% fraction of inspired oxygen in patients undergoing surgery: an updated systematic review and meta-analysis. Br J Anaesth. 2019;122(3):325–34.
Hovaguimian F, Elia N, Tramèr MR. Supplemental oxygen and the risk of surgical site infection: evidence of compromised data requires correction of previously published meta-analysis. Anesthesiology. 2019;131(4):932–3.
Cohen B, Schacham YN, Ruetzler K, Ahuja S, Yang D, Mascha EJ, et al. Effect of intraoperative hyperoxia on the incidence of surgical site infections: a meta-analysis. Br J Anaesth. 2018;120(6):1176–86.
Morkane CM, McKenna H, Cumpstey AF, Oldman AH, Grocott MPW, Martin DS. Pan London Perioperative Audit and Research Network (PLAN); South Coast Perioperative Audit and Research Collaboration (SPARC). Intraoperative oxygenation in adult patients undergoing surgery (iOPS): a retrospective observational study across 29 UK hospitals. Perioper Med. 2018;7:17.
LAS Vegas investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol. 2017;34(8):492–507.
Meyhoff CS, Jorgensen LN, Wetterslev J, Siersma VD, Rasmussen LS; PROXI Trial Group. Risk of new or recurrent cancer after a high perioperative inspiratory oxygen fraction during abdominal surgery. Br J Anaesth 2014;113(1): 74–81.
Fonnes S, Gögenur I, Søndergaard ES, Siersma VD, Jorgensen LN, Wetterslev J, et al. Perioperative hyperoxia - Long-term impact on cardiovascular complications after abdominal surgery, a post hoc analysis of the PROXI trial. Int J Cardiol. 2016;215:238–43.
Mattishent K, Thavarajah M, Sinha A, Peel A, Egger M, Solomkin J. Safety of 80% vs 30–35% fraction of inspired oxygen in patients undergoing surgery: a systematic review and meta-analysis. Br J Anaesth. 2019;122(3):311–24.
Meyhoff CS. Perioperative hyperoxia: why guidelines, research and clinical practice collide. Br J Anaesth. 2019;122(3):289–91.
Grocott MPW, Miller TE, Mythen MMG, Martin DS, de Jonge S, Latif A, et al. Perioperative oxygen therapy: meaningful outcomes and unintended consequences? Br J Anaesth. 2019;123(1):e6-7.
Staehr-Rye AK, Meyhoff CS, Scheffenbichler FT, Vidal Melo MF, Gätke MR, Walsh JL, et al. High intraoperative inspiratory oxygen fraction and risk of major respiratory complications. Br J Anaesth. 2017;119(1):140–9.
Weenink RP, de Jonge SW, van Hulst RA, Wingelaar TT, van Ooij PAM, Immink RV, et al. Perioperative hyperoxyphobia: justified or not? Benefits and harms of hyperoxia during surgery. J Clin Med. 2020;9(3):642.
Kotani N, Hashimoto H, Sessler DI, Muraoka M, Hashiba E, Kubota T, Matsuki A. Supplemental intraoperative oxygen augments antimicrobial and proinflammatory responses of alveolar macrophages. Anesthesiology. 2000;93(1):15–25.
Knight PR, Holm BA. The three components of hyperoxia. Anesthesiology. 2000;93(1):3–5.
Jubran A, Tobin MJ. Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients. Chest. 1990;97(6):1420–5.
Van de Louw A, Cracco C, Cerf C, Harf A, Duvaldestin P, Lemaire F, Brochard L. Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 2001;27(10):1606–13.
Perkins GD, McAuley DF, Giles S, Routledge H, Gao F. Do changes in pulse oximeter oxygen saturation predict equivalent changes in arterial oxygen saturation? Crit Care. 2003;7(4):R67.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. PR received grants from the Deutsche Forschungsgemeinschaft (CRC 1149, GRK 2003) and the German Ministry of Defence.
Author information
Authors and Affiliations
Contributions
PA and PR drafted the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors read and approved the final manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Demiselle, J., Calzia, E., Hartmann, C. et al. Target arterial PO2 according to the underlying pathology: a mini-review of the available data in mechanically ventilated patients. Ann. Intensive Care 11, 88 (2021). https://doi.org/10.1186/s13613-021-00872-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-021-00872-y