Abstract
During septic shock, fluid therapy is aimed at increasing cardiac output and improving tissue oxygenation, but it poses two problems: it has inconsistent and transient efficacy, and it has many well-documented deleterious effects. We suggest that there is a place for its personalization according to the patient characteristics and the clinical situation, at all stages of circulatory failure. Regarding the choice of fluid for volume expansion, isotonic saline induces hyperchloremic acidosis, but only for very large volumes administered. We suggest that balanced solutions should be reserved for patients who have already received large volumes and in whom the chloremia is rising. The initial volume expansion, intended to compensate for the constant hypovolaemia in the initial phase of septic shock, cannot be adapted to the patient’s weight only, as suggested by the Surviving Sepsis Campaign, but should also consider potential absolute hypovolemia induced by fluid losses. After the initial fluid infusion, preload responsiveness may rapidly disappear, and it should be assessed. The choice between tests used for this purpose depends on the presence or absence of mechanical ventilation, the monitoring in place and the risk of fluid accumulation. In non-intubated patients, the passive leg raising test and the mini-fluid challenge are suitable. In patients without cardiac output monitoring, tests like the tidal volume challenge, the passive leg raising test and the mini-fluid challenge can be used as they can be performed by measuring changes in pulse pressure variation, assessed through an arterial line. The mini-fluid challenge should not be repeated in patients who already received large volumes of fluids. The variables to assess fluid accumulation depend on the clinical condition. In acute respiratory distress syndrome, pulmonary arterial occlusion pressure, extravascular lung water and pulmonary vascular permeability index assess the risk of worsening alveolar oedema better than arterial oxygenation. In case of abdominal problems, the intra-abdominal pressure should be taken into account. Finally, fluid depletion in the de-escalation phase is considered in patients with significant fluid accumulation. Fluid removal can be guided by preload responsiveness testing, since haemodynamic deterioration is likely to occur in patients with a preload dependent state.
Similar content being viewed by others
Background
The first therapeutic measure in septic shock, volume expansion, is seemingly simple: a few hundred millilitres of fluid injected intravenously over a few minutes. However, nothing is simple in the strategy of using fluids in septic patients. Several different types of fluids are available today [1]. The effects of a fluid bolus are inconsistent and transient [2]. Fluids are risky treatments, particularly during septic shock [3]. Then, many questions raise in practice. Which fluid to choose? Should it be infused? How to evaluate its risk and refrain from infusing it? How to predict its effects? How to evaluate them?
To these questions, one can provide a standard and unequivocal answer. This is what the current guidelines do [4], without distinguishing according to the clinical context and the patient characteristics. The aim is likely to make them general enough to be applied widely, which is undoubtedly laudable. Another reason is that these guidelines are based on existing randomized controlled trials, which have often paid little attention to the particularities of patients they included. So, while these recommendations are of great value, there is probably room for a more personalized fluid management [5, 6]. Contrary to a “universal” strategy, the idea that “one size does not fit all” has been defended for many years about several strategies in critical care medicine [7, 8]. The need for personalization of treatment has emerged as a virtuous goal to pursue [5], especially in septic shock [6, 9]. This is the case for fluids as for any other treatment.
In this review, we will describe what a personalized fluid strategy in septic shock can be, based not only on the existing publications, but also on the pathophysiological concepts underlying the effects of fluids. From the choice of fluid type to the decision to remove the fluid administered in excess, we will try to show that, at each stage, the choices can reasonably be individualized.
How to customize the choice of fluid type?
No colloids, but balanced crystalloids…
In septic shock, crystalloids are indicated in first intention by the Surviving Sepsis Campaign (SSC) [4]. However, even though few evidence supports this choice, iso-oncotic albumin may be chosen for instance in patients with low albuminemia and perhaps with fluid accumulation, to increase the plasma oncotic pressure.
The current debate is mainly between the use of balanced or unbalanced crystalloids. Using saline as the main fluid source can induce hyperchloremic acidosis, which may decrease kidney cortical perfusion and could induce renal failure. Several studies have suggested that compared to chloride-rich solutions, balanced solutions reduce the incidence of renal failure [10, 11] and possibly mortality [11,12,13].
Accordingly, the 2021 SSC guidelines suggested to prefer balanced crystalloids in all septic shock patients [4]. This weak recommendation is mainly based on the SMART study, which had its own limitations (a single centre, no individual randomization and questionable identification of sepsis) [13].
Balanced crystalloids, but for all patients?
Should we favour these balanced solutions as first intention in all septic shock patients? Like other authors [6], we think that this choice should rather be personalized. Normal saline may induce hyperchloremia [14], but only if large volumes are administered. In a 70-kg patient, 12 litres must be infused for the blood bicarbonate level to drop by 10 mmol/L [15]. Balanced crystalloids should be logically reserved for patients requiring large fluid volumes and in whom chloremia rises significantly [16] (Fig. 1). Moreover, unbalanced crystalloids must be preferred in case of traumatic brain injury [17] and hypochloremia. In any case, chloremia should be measured to tailor the type of fluids [16].
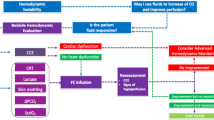
Criteria to customize the fluid strategy at different steps of septic shock. ARDS acute respiratory distress syndrome, CO cardiac output, C(O2) oxygen content, CRT capillary refill time, CVP central venous pressure, EEXPO end-expiratory occlusion, HR heart rate, ICU intensive care unit, MAP mean arterial pressure, P/F ratio ratio of the arterial oxygen partial pressure to the inspired oxygen fraction, PAOP pulmonary artery occlusion pressure, PCO2 carbon dioxide partial pressure, PLR passive leg raising, PPV pulse pressure variation, PI perfusion index, RR: respiratory rate, RV right ventricular, SvO2 mixed, venous oxygen saturation, ScvO2 central venous oxygen saturation, SVV stroke volume variation, Vt tidal volume
Indirectly, this opinion is reinforced by the results of the PLUS study [18]. Previous studies had demonstrated a beneficial [11] or neutral [19, 20] effect of balanced crystalloids compared to 0.9% saline. The PLUS study compared PlasmaLyte vs. normal saline in critically ill patients (not only septic) [18]. The study was negative: mortality and risk of acute renal failure were not lower with the balanced crystalloid, including in septic patients. But is this surprising? The study included an indistinct population of intensive care unit (ICU) patients, who received <2 litres of fluid per day during the first 2 days. Then, chloremia was ultimately very little different between groups [18], so that the balanced solution could not exert any benefit in the treated group. The study may have been positive if the use of balanced solution had been conditioned to the infused volume and chloremia.
We must personalize the fluid balance of patients in septic shock!
Fluid is harmful... but studies that tested fluid restriction showed no effect on mortality
On the one hand, fluid accumulation during the ICU is harmful [2]. Numerous studies have demonstrated that the cumulative fluid balance independently influences mortality in ICU patients [21], particularly during septic shock [3] and acute respiratory distress syndrome (ARDS) [22].
On the other hand, the several interventional studies that compared “liberal” vs. “conservative” or “restrictive” fluid strategies [23,24,25,26,27,28,29,30] provided consistent results: such strategies reduce the fluid balance, without deleterious effects, especially on the kidneys, but with no reduction in mortality, even if this was not the primary objective of some studies [25,26,27]. Some showed that the reduction in fluid balance decreased the duration of mechanical ventilation and the ICU stay [28, 29].
… but they have two major flaws
First, a maximal reduction of the fluid balance can only be achieved if all possible means are used for this purpose (Fig. 2). However, studies have restricted either resuscitation fluids [24, 26, 30, 31], or maintenance and replacement fluids [26, 27, 31], or protocolized fluid removal [27], but never all three at the same time. In the CLASSIC study, fluid restriction was limited to fluid bolus infusion [25]. Then, the total volume administered was little different between groups (at day-5, only 700 mL saved in the restrictive group [25]), reducing the chances of observing a difference in outcome. Conversely, in the RADAR-2 study, a strategy based on limiting maintenance fluids and removing fluid reduced the cumulative fluid balance to a larger extent (3 300 mL at day-5) [27].
The second shortcoming is that these studies did not individualize the strategy according to the patient characteristics. Some have included patients particularly at risk of fluid accumulation, such as ARDS patients [28]; others have been conducted in an indistinct population [27], including patients in whom the expected benefit of a conservative strategy was necessarily less. Also, no study has tested an individualized fluid restriction on the physiological state of the patient. For instance, preload responsiveness has not been considered while this is known to reduce the fluid balance [32, 33].
Thus, if the reduction of the cumulative fluid balance seems to be a goal to pursue in septic shock patients, the strategy to achieve it should not be standardized. We suggest a method which considers all the resuscitation phases (Fig. 2) and which is personalized (Fig. 1).
How to customize the initial fluid volume?
The latest SSC guidelines state that septic patients with hypotension or an elevated blood lactate should receive ≥30 mL/kg of crystalloid within 3 hours of presentation [4]. This volume, which is only based on an observational study [34], aims to compensate for relative and absolute hypovolaemia during initial septic shock. The patient’s weight is the only parameter of individualization. Yet, the degree of initial volume deficit obviously differs among patients. First, relative hypovolaemia is linked to venous vasodilation, depending on shock severity. Second, in some patients, fluid losses may account for absolute hypovolaemia, which must also be compensated. For example, the fluid deficit must be larger during peritonitis than during pneumonia. The recommendation of an arbitrary volume of 30 mL/kg inevitably leads to under-resuscitation in some patients and fluid overload in others [35]. In addition, tolerance to fluid administration also depends on the cardiac function. The initial fluid therapy should then be individualized. For instance, deciding to reduce the initial volume infused only based on the patient condition may increase mortality [34].
In the very initial phase, as hypovolaemia is constant, testing preload responsiveness is not warranted and may delay resuscitation. Afterwards, volume expansion should be individualized according to the degree of preload responsiveness, to avoid unnecessary fluid infusion (Fig. 1) [36]. This is recommended by the SSC which, on this point, suggests individualization of treatment [4]. Assessing preload responsiveness should not be delayed as it disappears quickly after the onset of septic shock and it [37, 38]. In the ANDROMEDA-SHOCK study, after having received 27 mL/kg of fluids, 70% of patients were still preload responsive at inclusion, and among them, <20% remained so four hours later [38]. Guiding initial fluid therapy by evaluating preload responsiveness during septic shock can reduce the fluid balance [32].
How to customize the choice of test or index of preload responsiveness?
Reviews detailing indices and tests to detect preload responsiveness can be found elsewhere [39]. Our goal here is to describe what leads to choosing one over another. This choice depends on three questions (Fig. 1).
Is the patient intubated?
The passive leg raising (PLR) test and the mini-fluid challenge do not require mechanical ventilation. This makes them usable, for example, in the emergency department, while patients are not yet intubated [39]. Of course, tests based on cardiopulmonary interactions can only be used in intubated and ventilated patients. Pulse pressure variation (PPV) and stroke volume variation (SVV) (in absolute value) can only be used in patients without spontaneous breathing, with a tidal volume (Vt) ≥8 mL/kg, with a compliance of the respiratory system ≥30 mL/cmH2O, without intra-abdominal hypertension, with sinus cardiac rhythm and with a ratio of heart rate to respiratory rate ≥3.6 [40], i.e. in a minority of shock patients [39]. The changes in diameter of inferior and superior vena cava have the same limitations (except arrhythmia and for superior vena cava, the high respiratory rate). Even under optimal conditions of use, it has a lesser diagnostic value, especially for the inferior vena cava distensibility [41].
The end-expiratory occlusion (EEXPO) test (end-expiratory pause of 15 seconds, which increases cardiac output (CO) in the event of preload responsiveness [42]), can be used in ventilated patients even in case of arrhythmia, whatever the Vt and the positive end-expiratory pressure level. However, the patient must tolerate this rather long breathing interruption [43].
In ventilated patients with a Vt of 6 mL/kg, the Vt challenge (temporary increase in Vt to 8 mL/kg, which increases PPV in case of preload responsiveness [44]) is valid with spontaneous breathing, which makes it widely usable. Its validity is better and better demonstrated [39]. Recruitment manoeuvres [45] are only indicated in ARDS patients and not routinely [46], which greatly limits their use. Finally, in prone positioning, the Trendelenburg manoeuvre may be used to transfer blood to cardiac cavities and detect preload responsiveness [47]. It has received little validation at the moment. In prone position, the Vt challenge is also valid [48] (Fig. 1).
Which haemodynamic monitoring is in place?
The great advantage of the Vt challenge [44], the PLR test [49, 50] and perhaps the mini-fluid challenge [51], is that they can be carried out with the simple PPV, i.e. only requiring a single arterial line. For the PLR test, many other variables can replace CO, such as end-tidal carbon dioxide in ventilated patients [52], or the perfusion index of plethysmography [53, 54].
The EEXPO test requires a precise measurement of CO, because the changes in stroke volume induced are small [42]. If echocardiography is used, end-expiratory and end-inspiratory pauses should be combined [55] to amplify the changes in velocity time integral and to make them more compatible with the precision of echocardiography [56].
What is the risk of fluid accumulation?
The mini-fluid challenge requires the injection of 100-150 mL of fluid, which cannot be withdrawn if ineffective [57]. It is then reasonable not to repeat it if the risk of fluid accumulation is high. From this point of view, it is probably better suited to the operating room than the ICU (Fig. 1).
How to personalize the decision to add a vasopressor to fluid?
Vasopressors may have synergistic effects with fluids
Norepinephrine is usually started once fluid boluses no longer exert any benefit, to increase arterial pressure [4]. However, its effects on systemic venous return should not be overlooked, as they may contribute to limiting the fluid balance during septic shock (Fig. 2). By binding to the venous alpha-adrenergic receptors, norepinephrine induces vasoconstriction which increases the part of stressed blood volume [58]. It increases mean systemic pressure, exerting a fluidlike effect [59]. In addition, volume expansion performed under vasopressor may exert a larger effect on cardiac preload, because it occurs in a constricted venous territory [60].
Vasopressors may be administered early in some patients
These venous effects of norepinephrine are synergistic with the administration of fluid, which may reduce the quantity of fluid administered for resuscitation (Fig. 2). Observational studies in septic patients suggested that an early start of norepinephrine could reduce the fluid balance [61, 62], and one of them matching patients with a propensity score suggested a better survival when norepinephrine was administered very early [63]. However, opposite observational results have been reported [64].
The CLOVERS study randomized patients between a restrictive strategy, prioritizing lower intravenous fluid volumes and vasopressors, and a liberal strategy, prioritizing higher fluid volumes before starting vasopressors. Although less fluid was administered within the first 24 hours, mortality at day-90 did not differ between groups [31]. However, the interventional arm combined early norepinephrine administration with a restrictive fluid strategy, suffering from the flaws of the studies mentioned above, so the prognostic impact of early norepinephrine administration alone cannot be inferred from these results.
Moreover, in this study, patients in whom norepinephrine was administered earlier were not selected [31]. This early administration of norepinephrine should likely be considered in the most hypotensive septic patients, to prompt blood pressure restoration. Also, norepinephrine is likely most powerful in patients with marked vasodilation, as indicated by a low diastolic pressure (e.g. <40 mmHg) (Fig. 1). The diastolic shock index (heart rate divided by diastolic arterial pressure), which predicts death better than each variable alone, may also be considered for this purpose [65].
In addition, the effectiveness of a fluid bolus on CO is ephemeral. In the perioperative context, the effects on CO of a 250-mL crystalloid bolus were shown to disappear after 10 minutes [66]. This duration could be even shorter in septic patients, due to vasodilation and capillary leakage. Even if it has not been investigated, the effects of a fluid bolus on microcirculation are also likely transient. Therefore, in septic patients, restoring haemodynamics with norepinephrine probably allows a more persistent effect, although this has not been proved yet.
How to customize the criteria for stopping fluid infusion?
Good fluid management should include safety criteria, indicating that the risk of fluid infusion outweighs the expected benefit [67]. These criteria are particularly important in the stabilization phase, after having corrected the initial hypovolaemia [67] (Fig. 2). Two clinical situations may justify monitoring of particular indices.
In patients with ARDS
In these patients, to alert to the risk of additional fluid infusion, one often uses the ratio of arterial partial pressure of oxygen (PaO2) to fractional inspiration of oxygen (FiO2). However, it can also be lowered by pulmonary consolidations, shunt related to microthrombi, etc., which are not influenced by additional fluid infusion.
“Sophisticated” haemodynamic monitoring techniques estimate the pulmonary risk of fluid resuscitation more directly. The pulmonary artery catheter estimates the pulmonary capillary pressure, which propels fluid into the interstitium. The estimation of this pressure by echocardiography is poorly reliable in critically ill patients [68].
Extravascular lung water and pulmonary vascular permeability measured by transpulmonary thermodilution directly reflect the risk of fluid leakage towards the interstitium and alveoli [69]. The maximum value of lung water influences the prognosis of ARDS patients, independently of other severity criteria [70].
Lung ultrasound evidences interstitial lung oedema by B-lines [71]. While reliable for diagnosing interstitial oedema, its value for quantifying the total volume of pulmonary oedema can only go through a tedious count of the B-lines number [72]. Moreover, it neglects alveolar oedema, so that it poorly reflects total lung water [73].
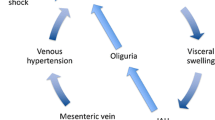
In patients with intra-abdominal hypertension
Especially in patients with abdominal problems, the intra-abdominal pressure (IAP) should be considered to estimate the risk of fluid accumulation which, via visceral and parietal oedema, increases IAP [74]. Intra-abdominal hypertension impairs the perfusion of abdominal organs, mainly the kidneys, and independently influences the prognosis of ICU patients [75]. This variable must be considered before deciding to administer a fluid bolus during the stabilization phase [76].
Don't forget CVP!
Regardless of the patient, even if CVP does not predict preload responsiveness, its measurement provides a great deal of information that is often overlooked [77]. CVP is the backward pressure of organ blood flow [78], and increased CVP levels are associated with organ dysfunction [79]. Limiting the increase in CVP may be a reasonable goal, and it might be justified to target higher mean arterial pressure targets in patients with elevated CVP.
How to personalize therapeutic targets?
Fluid boluses are aimed at increasing mean systemic pressure, cardiac preload, consequently stroke volume and CO, and ultimately at improving tissue oxygenation. However, the therapeutic targets must be adapted to the available haemodynamic monitoring and to the context.
Outside the ICU
When fluid therapy is conducted in the wards, in the pre-hospital or in the emergency department, the clinical examination must look for clinical signs of improvement in tissue perfusion: disappearance of skin mottling, shortening of capillary refill time, which disappears quite faster and might change even after a single fluid bolus [80, 81]. Improved organ function, especially increased diuresis, is rarely available because of the very short observation time (Fig. 1). Although these signs should always be looked for, they poorly reflect CO changes [82].
The primary effect of a bolus of fluid is to increase CO, and arterial pressure increases only incidentally [83]. Of note, the target of mean arterial pressure may be adapted to the existence of previous hypertension [84]. However, pulse pressure is the one that should be observed to monitor CO changes, because it is the pressure value that best reflects stroke volume. Changes in mean arterial pressure are attenuated, as the sympathetic system tends to keep it constant as CO varies. It is surprising to see that restoring mean arterial pressure can be considered as the objective of fluid therapy [85, 86].
However, even changes in pulse pressure imperfectly reflect CO [83, 87, 88], likely even more when assessed through a brachial cuff. Similarly, the decrease in heart rate is unreliable to detect the fluid-induced increase in CO [88]. This is what justifies measuring CO directly, when possible, to better assess the fluid effects.
In the ICU
More variables are available to estimate fluid efficacy. CO is easily measured, either by transpulmonary thermodilution, pulmonary arterial catheter, recommended in the most severe patients [89], or by echocardiography. If no direct measurement of CO is available but an arterial line is in place, a decrease in PPV reflects the decrease in preload responsiveness and demonstrates the response to fluid [90]. In intubated and perfectly stably ventilated patients, the increase in end-tidal carbon dioxide parallels the increase in CO [52, 91]. The amplitude of the plethysmography signal, quantified by the perfusion index, could also reflect the fluid-induced increase in CO, as has been suggested by a few studies [53, 54, 92].
Also, the effects on tissue oxygenation must be assessed [67], as an increased CO does not always result in an improved oxygen consumption, either because oxygen consumption and delivery are independent [93] or because the microcirculation is deranged [94]. In the ICU, several variables are available for this purpose. The reduction of lactate, which is associated with a favourable prognosis [95], is a valid therapeutic objective. Through the central venous catheter which is very often inserted, venous oxygen saturation and carbon dioxide-derived variables [96] show improved tissue oxygenation. These variables are more reliably measured from mixed venous blood if a pulmonary artery catheter is in place. In cases where venous oxygen saturation is normal, the ratio of the veno-arterial difference in carbon dioxide partial pressure to the arteriovenous difference in oxygen content, an estimate of the respiratory quotient, has been suggested as a marker of anaerobic metabolism with faster response than lactate and less false positives [96]. Its normal value has been reported to be <1.4 [97], though different thresholds have been reported [98].
How to customize fluid depletion?
One of the ways to reduce the total fluid balance is to undertake active fluid depletion, at the “evacuation” phase of the resuscitation–optimization–stabilization–evacuation (ROSE) concept (Fig. 2). Indeed, the reduction of resuscitation fluids alone is insufficient, because maintenance and replacement fluids represent a large proportion of the fluids infused in the ICU [99]. The modalities for this de-escalation are variable [100], and they should be personalized by considering usefulness and safety.
In which patients should fluid removal be undertaken?
Fluid depletion should be the most beneficial in patients with the largest fluid accumulation, as indicated by the variables mentioned above: high left ventricular filling pressure, high CVP, very lung water, signs of pulmonary congestion on CT scan and elevated IAP. The presence of soft tissue oedema does not necessarily have to be required, as they may on the contrary be accompanied by a depleted intravascular sector.
Conversely, if fluid accumulation is low, for example in easily resolving septic shock, the benefit of fluid depletion is less obvious. The risk of undertaking it must therefore be weighed against the possible benefits.
How to remove fluid?
Diuretics are used first. However, in case of oliguria or anuria, ultrafiltration during renal replacement therapy is the alternative solution [101]. In case of low albumin, 20% hyperoncotic albumin could induce a synergistic effect on fluid removal. In patients ventilated for acute lung injury, a strategy associating positive end-expiratory pressure adjusted to IAP followed by infusion of hyperoncotic albumin and furosemide resulted in negative cumulative fluid balance and decreased lung water and IAP [102].
How to choose the dose of fluid to withdraw?
The risk of too much fluid withdrawal is to alter the haemodynamic state. To ensure the safety of fluid depletion, physiological conditions must be considered, which is rarely done in practice [100]. First, the haemodynamic state must be stable, and the vasopressors must be at low dose or stopped.
Then, decreasing cardiac preload with fluid removal can only alter the haemodynamic condition in case of preload responsiveness. Conversely, if ventricles are preload unresponsive, fluid removal must be well tolerated. One should condition the decision to withdraw fluid to the existence of a preload unresponsiveness. In a study in critically ill patients in a stabilized phase of shock, fluid removal undertaken by ultrafiltration did not induce intra-dialytic hypotension in patients who did not have preload responsiveness, as well as proved by a negative PLR test before depletion [103] (Fig. 1). Even if at the priming of the extracorporeal circuit, a decrease in CO is much more frequent in the case of preload responsiveness than in the case of preload unresponsiveness [104], other factors may be responsible for intra-dialytic hypotension. However, the fact remains that the existence of a preload responsiveness must urge not to withdraw additional fluid.
Conclusion
Despite its apparent simplicity, fluid therapy is complex. Fluids are drugs, inconsistently effective and endowed with notable deleterious effects. Like any medicine, they must be administered at the right dose and only to patients who need them. To guide fluid therapy, rather than relying on an identical strategy for all patients, it is possible to personalize decisions. Consider the characteristics of the patient (the severity of the vasodilation, the importance of the fluid accumulation), his/her clinical history (to assess the depth of the initial hypovolaemia), his/her physiological conditions (in particular preload responsiveness), should logically ensure effective and safe fluid delivery and removal. If these individual criteria are not considered, clinical studies investigating the various fluid therapy strategies are and will remain negative.
Availability of data and materials
Not applicable.
References
Vincent JL. Types of intravenous fluid: WHICH fluid for which patient, and do RCTs help? Anaesth Crit Care Pain Med. 2020;39(6):753–4.
Malbrain M, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal PJ, Joannes-Boyau O, Teboul JL, Rice TW, Mythen M, Monnet X. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8(1):66.
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34(2):344–53.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, McIntyre L, Ostermann M, Prescott HC, et al. Executive summary: surviving sepsis campaign: international guidelines for the management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):1974–82.
De Backer D, Cecconi M, Chew MS, Hajjar L, Monnet X, Ospina-Tascon GA, Ostermann M, Pinsky MR, Vincent JL. A plea for personalization of the hemodynamic management of septic shock. Crit Care. 2022;26(1):372.
Vincent JL, Singer M, Einav S, Moreno R, Wendon J, Teboul JL, Bakker J, Hernandez G, Annane D, de Man AME, et al. Equilibrating SSC guidelines with individualized care. Crit Care. 2021;25(1):397.
Perel A. Bench-to-bedside review: the initial hemodynamic resuscitation of the septic patient according to Surviving Sepsis Campaign guidelines–does one size fit all? Crit Care. 2008;12(5):223.
Vincent JL, van der Poll T, Marshall JC. The end of “one size fits all” sepsis therapies: toward an individualized approach. Biomedicines. 2022;10(9):2260.
Bakker J, Kattan E, Annane D, Castro R, Cecconi M, De Backer D, Dubin A, Evans L, Gong MN, Hamzaoui O, et al. Current practice and evolving concepts in septic shock resuscitation. Intensive Care Med. 2022;48(2):148–63.
Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308(15):1566–72.
Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, Stollings JL, Kumar AB, Hughes CG, Hernandez A, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378(9):829–39.
Raghunathan K, Shaw A, Nathanson B, Sturmer T, Brookhart A, Stefan MS, Setoguchi S, Beadles C, Lindenauer PK. Association between the choice of IV crystalloid and in-hospital mortality among critically ill adults with sepsis*. Crit Care Med. 2014;42(7):1585–91.
Brown RM, Wang L, Coston TD, Krishnan NI, Casey JD, Wanderer JP, Ehrenfeld JM, Byrne DW, Stollings JL, Siew ED, et al. Balanced crystalloids versus saline in sepsis. A secondary analysis of the SMART clinical trial. Am J Respir Crit Care Med. 2019;200(12):1487–95.
Bellomo R, Morimatsu H, French C, Cole L, Story D, Uchino S, Naka T, Investigators SS. The effects of saline or albumin resuscitation on acid-base status and serum electrolytes. Crit Care Med. 2006;34(12):2891–7.
O’Dell E, Tibby SM, Durward A, Murdoch IA. Hyperchloremia is the dominant cause of metabolic acidosis in the postresuscitation phase of pediatric meningococcal sepsis. Crit Care Med. 2007;35(10):2390–4.
Vincent JL, De Backer D. Saline versus balanced solutions: Are clinical trials comparing two crystalloid solutions really needed? Crit Care. 2016;20(1):250.
Zampieri FG, Machado FR, Biondi RS, Freitas FGR, Veiga VC, Figueiredo RC, Lovato WJ, Amendola CP, Assuncao MSC, Serpa-Neto A, et al. Effect of slower vs faster intravenous fluid bolus rates on mortality in critically ill patients: the basics randomized clinical trial. JAMA. 2021;326(9):830–8.
Finfer S, Micallef S, Hammond N, Navarra L, Bellomo R, Billot L, Delaney A, Gallagher M, Gattas D, Li Q, et al. Balanced multielectrolyte solution versus saline in critically ill adults. N Engl J Med. 2022;386(9):815–26.
Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, McGuinness S, Mehrtens J, Myburgh J, Psirides A, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA. 2015;314(16):1701–10.
Liu C, Lu G, Wang D, Lei Y, Mao Z, Hu P, Hu J, Liu R, Han D, Zhou F. Balanced crystalloids versus normal saline for fluid resuscitation in critically ill patients: a systematic review and meta-analysis with trial sequential analysis. Am J Emerg Med. 2019;37(11):2072–8.
Messmer AS, Zingg C, Muller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients—a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48(12):1862–70.
Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, Teboul JL, Monnet X. Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome. Crit Care Med. 2013;41(2):472–80.
Meyhoff TS, Moller MH, Hjortrup PB, Cronhjort M, Perner A, Wetterslev J. Lower vs higher fluid volumes during initial management of sepsis: a systematic review with meta-analysis and trial sequential analysis. Chest. 2020;157(6):1478–96.
Corl KA, Prodromou M, Merchant RC, Gareen I, Marks S, Banerjee D, Amass T, Abbasi A, Delcompare C, Palmisciano A, et al. The restrictive IV fluid trial in severe sepsis and septic shock (RIFTS): a randomized pilot study. Crit Care Med. 2019;47(7):951–9.
Meyhoff TS, Hjortrup PB, Wetterslev J, Sivapalan P, Laake JH, Cronhjort M, Jakob SM, Cecconi M, Nalos M, Ostermann M, et al. Restriction of intravenous fluid in ICU patients with septic shock. N Engl J Med. 2022;386(26):2459–70.
Macdonald SPJ, Keijzers G, Taylor DM, Kinnear F, Arendts G, Fatovich DM, Bellomo R, McCutcheon D, Fraser JF, Ascencio-Lane JC, et al. Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): a pilot randomised controlled trial. Intensive Care Med. 2018;44(12):2070–8.
Silversides JA, McMullan R, Emerson LM, Bradbury I, Bannard-Smith J, Szakmany T, Trinder J, Rostron AJ, Johnston P, Ferguson AJ, et al. Feasibility of conservative fluid administration and deresuscitation compared with usual care in critical illness: the Role of Active Deresuscitation After Resuscitation-2 (RADAR-2) randomised clinical trial. Intensive Care Med. 2022;48(2):190–200.
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75.
Silversides JA, Major E, Ferguson AJ, Mann EE, McAuley DF, Marshall JC, Blackwood B, Fan E. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis. Intensive Care Med. 2017;43(2):155–70.
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettila V, Aaen A, Lodahl D, Berthelsen RE, Christensen H, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016;42(11):1695–705.
Shapiro NI, Douglas IS, Brower RG, Brown SM, Exline MC, Ginde AA, Gong MN, Grissom CK, Hayden D, National Heart Lung, and Blood Institute Prevention Early Treatment of Acute Lung Injury Clinical Trials Network, et al. Early restrictive or liberal fluid management for sepsis-induced hypotension. N Engl J Med. 2023;388(6):499–510.
Douglas IS, Alapat PM, Corl KA, Exline MC, Forni LG, Holder AL, Kaufman DA, Khan A, Levy MM, Martin GS, et al. Fluid response evaluation in sepsis hypotension and shock: a randomized clinical trial. Chest. 2020;158(4):1431–45.
Richard JC, Bayle F, Bourdin G, Leray V, Debord S, Delannoy B, Stoian AC, Wallet F, Yonis H, Guerin C. Preload dependence indices to titrate volume expansion during septic shock: a randomized controlled trial. Crit Care. 2015;19:5.
Kuttab HI, Lykins JD, Hughes MD, Wroblewski K, Keast EP, Kukoyi O, Kopec JA, Hall S, Ward MA. Evaluation and predictors of fluid resuscitation in patients with severe sepsis and septic shock. Crit Care Med. 2019;47(11):1582–90.
Jozwiak M, Hamzaoui O, Monnet X, Teboul JL. Fluid resuscitation during early sepsis: a need for individualization. Minerva Anestesiol. 2018;84(8):987–92.
De Backer D, Aissaoui N, Cecconi M, Chew MS, Denault A, Hajjar L, Hernandez G, Messina A, Myatra SN, Ostermann M, et al. How can assessing hemodynamics help to assess volume status? Intensive Care Med. 2022;48(10):1482–94.
Roger C, Zieleskiewicz L, Demattei C, Lakhal K, Piton G, Louart B, Constantin JM, Chabanne R, Faure JS, Mahjoub Y, et al. Time course of fluid responsiveness in sepsis: the fluid challenge revisiting (FCREV) study. Crit Care. 2019;23(1):179.
Kattan E, Ospina-Tascon GA, Teboul JL, Castro R, Cecconi M, Ferri G, Bakker J, Hernandez G, Investigators A-S. Systematic assessment of fluid responsiveness during early septic shock resuscitation: secondary analysis of the ANDROMEDA-SHOCK trial. Crit Care. 2020;24(1):23.
Monnet X, Shi R, Teboul JL. Prediction of fluid responsiveness. What’s new? Ann Intensive Care. 2022;12(1):46.
De Backer D, Taccone FS, Holsten R, Ibrahimi F, Vincent JL. Influence of respiratory rate on stroke volume variation in mechanically ventilated patients. Anesthesiology. 2009;110(5):1092–7.
Vignon P, Repesse X, Begot E, Leger J, Jacob C, Bouferrache K, Slama M, Prat G, Vieillard-Baron A. Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med. 2017;195(8):1022–32.
Gavelli F, Shi R, Teboul JL, Azzolina D, Monnet X. The end-expiratory occlusion test for detecting preload responsiveness: a systematic review and meta-analysis. Ann Intensive Care. 2020;10(1):65.
Gavelli F, Teboul JL, Monnet X. The end-expiratory occlusion test: Please, let me hold your breath! Crit Care. 2019;23(1):274.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45(3):415–21.
Messina A, Colombo D, Barra FL, Cammarota G, De Mattei G, Longhini F, Romagnoli S, DellaCorte F, De Backer D, Cecconi M, et al. Sigh maneuver to enhance assessment of fluid responsiveness during pressure support ventilation. Crit Care. 2019;23(1):31.
Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, Forel JM, Guerin C, Jaber S, Mekontso-Dessap A, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69.
Yonis H, Bitker L, Aublanc M, Perinel Ragey S, Riad Z, Lissonde F, Louf-Durier A, Debord S, Gobert F, Tapponnier R, et al. Change in cardiac output during Trendelenburg maneuver is a reliable predictor of fluid responsiveness in patients with acute respiratory distress syndrome in the prone position under protective ventilation. Crit Care. 2017;21(1):295.
Shi R, Ayed S, Moretto F, Azzolina D, De Vita N, Gavelli F, Carelli S, Pavot A, Lai C, Monnet X, et al. Tidal volume challenge to predict preload responsiveness in patients with acute respiratory distress syndrome under prone position. Crit Care. 2022;26(1):219.
Taccheri T, Gavelli F, Teboul JL, Shi R, Monnet X. Do changes in pulse pressure variation and inferior vena cava distensibility during passive leg raising and tidal volume challenge detect preload responsiveness in case of low tidal volume ventilation? Crit Care. 2021;25(1):110.
Hamzaoui O, Shi R, Carelli S, Sztrymf B, Prat D, Jacobs F, Monnet X, Gouezel C, Teboul JL. Changes in pulse pressure variation to assess preload responsiveness in mechanically ventilated patients with spontaneous breathing activity: an observational study. Br J Anaesth. 2021;127(4):532–8.
Mallat J, Meddour M, Durville E, Lemyze M, Pepy F, Temime J, Vangrunderbeeck N, Tronchon L, Thevenin D, Tavernier B. Decrease in pulse pressure and stroke volume variations after mini-fluid challenge accurately predicts fluid responsivenessdagger. Br J Anaesth. 2015;115(3):449–56.
Monnet X, Bataille A, Magalhaes E, Barrois J, Le Corre M, Gosset C, Guerin L, Richard C, Teboul JL. End-tidal carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med. 2013;39(1):93–100.
Beurton A, Gavelli F, Teboul JL, De Vita N, Monnet X. Changes in the plethysmographic perfusion index during an end-expiratory occlusion detect a positive passive leg raising test. Crit Care Med. 2021;49(2):e151–60.
Beurton A, Teboul JL, Gavelli F, Gonzalez FA, Girotto V, Galarza L, Anguel N, Richard C, Monnet X. The effects of passive leg raising may be detected by the plethysmographic oxygen saturation signal in critically ill patients. Crit Care. 2019;23(1):19.
Jozwiak M, Depret F, Teboul JL, Alphonsine JE, Lai C, Richard C, Monnet X. Predicting fluid responsiveness in critically ill patients by using combined end-expiratory and end-inspiratory occlusions with echocardiography. Crit Care Med. 2017;45(11):e1131–8.
Jozwiak M, Mercado P, Teboul JL, Benmalek A, Gimenez J, Depret F, Richard C, Monnet X. What is the lowest change in cardiac output that transthoracic echocardiography can detect? Crit Care. 2019;23(1):116.
Messina A, Dell’Anna A, Baggiani M, Torrini F, Maresca GM, Bennett V, Saderi L, Sotgiu G, Antonelli M, Cecconi M. Functional hemodynamic tests: a systematic review and a metanalysis on the reliability of the end-expiratory occlusion test and of the mini-fluid challenge in predicting fluid responsiveness. Crit Care. 2019;23(1):264.
Persichini R, Lai C, Teboul JL, Adda I, Guerin L, Monnet X. Venous return and mean systemic filling pressure: physiology and clinical applications. Crit Care. 2022;26(1):150.
Persichini R, Silva S, Teboul JL, Jozwiak M, Chemla D, Richard C, Monnet X. Effects of norepinephrine on mean systemic pressure and venous return in human septic shock*. Crit Care Med. 2012;40(12):3146–53.
Adda I, Lai C, Teboul JL, Guerin L, Gavelli F, Monnet X. Norepinephrine potentiates the efficacy of volume expansion on mean systemic pressure in septic shock. Crit Care. 2021;25(1):302.
Kusakabe A, Sweeny A, Keijzers G, Steering Committee of the AFOSG. Early vs. late vassopressor therapy in the management of patients with sepsis and hypotension, a multicenter observational study. Arch Med Res. 2021;52(8):836–42.
Bai X, Yu W, Ji W, Lin Z, Tan S, Duan K, Dong Y, Xu L, Li N. Early versus delayed administration of norepinephrine in patients with septic shock. Crit Care. 2014;18(5):532.
Ospina-Tascon GA, Hernandez G, Alvarez I, Calderon-Tapia LE, Manzano-Nunez R, Sanchez-Ortiz AI, Quinones E, Ruiz-Yucuma JE, Aldana JL, Teboul JL, et al. Effects of very early start of norepinephrine in patients with septic shock: a propensity score-based analysis. Crit Care. 2020;24(1):52.
Yeo HJ, Lee YS, Kim TH, Jang JH, Lee HB, Oh DK, Park MH, Lim CM, Cho WH, Korean Sepsis Alliance I. Vasopressor initiation within 1 hour of fluid loading is associated with increased mortality in septic shock patients: analysis of national registry data. Crit Care Med. 2022;50(4):e351–60.
Ospina-Tascon GA, Teboul JL, Hernandez G, Alvarez I, Sanchez-Ortiz AI, Calderon-Tapia LE, Manzano-Nunez R, Quinones E, Madrinan-Navia HJ, Ruiz JE, et al. Diastolic shock index and clinical outcomes in patients with septic shock. Ann Intensive Care. 2020;10(1):41.
Aya HD, Ster IC, Fletcher N, Grounds RM, Rhodes A, Cecconi M. Pharmacodynamic analysis of a fluid challenge. Crit Care Med. 2016;44(5):880–91.
Monnet X, Teboul JL. My patient has received fluid. How to assess its efficacy and side effects? Ann Intensive Care. 2018;8(1):54.
Mercado P, Maizel J, Marc J, Beyls C, Zerbib Y, Zogheib E, Titeca-Beauport D, Joris M, Kontar L, Riviere A, et al. Doppler echocardiographic indices are specific but not sensitive to predict pulmonary artery occlusion pressure in critically ill patients under mechanical ventilation. Crit Care Med. 2021;49(1):e1–10.
Monnet X, Teboul JL. Transpulmonary thermodilution: advantages and limits. Crit Care. 2017;21(1):147.
Gavelli F, Shi R, Teboul JL, Azzolina D, Mercado P, Jozwiak M, Chew MS, Huber W, Kirov MY, Kuzkov VV, et al. Extravascular lung water levels are associated with mortality: a systematic review and meta-analysis. Crit Care. 2022;26(1):202.
Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199(6):701–14.
Ferre A, Guillot M, Lichtenstein D, Meziere G, Richard C, Teboul JL, Monnet X. Lung ultrasound allows the diagnosis of weaning-induced pulmonary oedema. Intensive Care Med. 2019;45(5):601–8.
Seibel A, Zechner PM, Berghold A, Holter M, Brass P, Michels G, Leister N, Gemes G, Donauer R, Giebler RM, et al. B-Lines for the assessment of extravascular lung water: Just focused or semi-quantitative? Acta Anaesthesiol Scand. 2020;64(7):953–60.
Holodinsky JK, Roberts DJ, Ball CG, Blaser AR, Starkopf J, Zygun DA, Stelfox HT, Malbrain ML, Jaeschke RC, Kirkpatrick AW. Risk factors for intra-abdominal hypertension and abdominal compartment syndrome among adult intensive care unit patients: a systematic review and meta-analysis. Crit Care. 2013;17(5):R249.
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–206.
Malbrain M, Langer T, Annane D, Gattinoni L, Elbers P, Hahn RG, De Laet I, Minini A, Wong A, Ince C, et al. Intravenous fluid therapy in the perioperative and critical care setting: executive summary of the International Fluid Academy (IFA). Ann Intensive Care. 2020;10(1):64.
De Backer D, Vincent JL. Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care. 2018;22(1):43.
Vellinga NA, Ince C, Boerma EC. Elevated central venous pressure is associated with impairment of microcirculatory blood flow in sepsis: a hypothesis generating post hoc analysis. BMC Anesthesiol. 2013;13:17.
Legrand M, Dupuis C, Simon C, Gayat E, Mateo J, Lukaszewicz AC, Payen D. Association between systemic hemodynamics and septic acute kidney injury in critically ill patients: a retrospective observational study. Crit Care. 2013;17(6):R278.
Raia L, Gabarre P, Bonny V, Urbina T, Missri L, Boelle PY, Baudel JL, Guidet B, Maury E, Joffre J, et al. Kinetics of capillary refill time after fluid challenge. Ann Intensive Care. 2022;12(1):74.
Jacquet-Lagreze M, Bouhamri N, Portran P, Schweizer R, Baudin F, Lilot M, Fornier W, Fellahi JL. Capillary refill time variation induced by passive leg raising predicts capillary refill time response to volume expansion. Crit Care. 2019;23(1):281.
Hiemstra B, Koster G, Wiersema R, Hummel YM, van der Harst P, Snieder H, Eck RJ, Kaufmann T, Scheeren TWL, Perner A, et al. The diagnostic accuracy of clinical examination for estimating cardiac index in critically ill patients: the Simple Intensive Care Studies-I. Intensive Care Med. 2019;45(2):190–200.
Monnet X, Letierce A, Hamzaoui O, Chemla D, Anguel N, Osman D, Richard C, Teboul JL. Arterial pressure allows monitoring the changes in cardiac output induced by volume expansion but not by norepinephrine*. Crit Care Med. 2011;39:1394–9.
Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, Dequin PF, Gergaud S, Weiss N, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370(17):1583–93.
Messina A, Calabro L, Pugliese L, Lulja A, Sopuch A, Rosalba D, Morenghi E, Hernandez G, Monnet X, Cecconi M. Fluid challenge in critically ill patients receiving haemodynamic monitoring: a systematic review and comparison of two decades. Crit Care. 2022;26(1):186.
Wall O, Cutuli S, Wilson A, Eastwood G, Lipka-Falck A, Tornberg D, Bellomo R, Cronhjort M. An observational study of intensivists’ expectations and effects of fluid boluses in critically ill patients. PLoS ONE. 2022;17(3): e0265770.
Pierrakos C, Velissaris D, Scolletta S, Heenen S, De Backer D, Vincent JL. Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med. 2012;38(3):422–8.
Ait-Hamou Z, Teboul JL, Anguel N, Monnet X. How to detect a positive response to a fluid bolus when cardiac output is not measured? Ann Intensive Care. 2019;9(1):138.
Cecconi M, Arulkumaran N, Kilic J, Ebm C, Rhodes A. Update on hemodynamic monitoring and management in septic patients. Minerva Anestesiol. 2014;80(6):701–11.
Mallat J, Fischer MO, Granier M, Vinsonneau C, Jonard M, Mahjoub Y, Baghdadi FA, Preau S, Poher F, Rebet O, et al. Passive leg raising-induced changes in pulse pressure variation to assess fluid responsiveness in mechanically ventilated patients: a multicentre prospective observational study. Br J Anaesth. 2022;129(3):308–16.
Monge Garcia MI, Gil Cano A, Gracia Romero M, Monterroso Pintado R, Perez Madueno V, Diaz Monrove JC. Non-invasive assessment of fluid responsiveness by changes in partial end-tidal CO2 pressure during a passive leg-raising maneuver. Ann Intensive Care. 2012;2:9.
de Courson H, Michard F, Chavignier C, Verchere E, Nouette-Gaulain K, Biais M. Do changes in perfusion index reflect changes in stroke volume during preload-modifying manoeuvres? J Clin Monit Comput. 2020;34(6):1193–8.
Monnet X, Julien F, Ait-Hamou N, Lequoy M, Gosset C, Jozwiak M, Persichini R, Anguel N, Richard C, Teboul JL. Markers of anaerobic metabolism are better than central venous oxygen saturation for detecting whether hemodynamic resuscitation will reduce tissue hypoxia. Intensive Care Med. 2011;37(Supp 1):S282.
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med. 2010;36(11):1813–25.
Jones AE. Lactate clearance for assessing response to resuscitation in severe sepsis. Acad Emerg Med. 2013;20(8):844–7.
Gavelli F, Teboul JL, Monnet X. How can CO2-derived indices guide resuscitation in critically ill patients? J Thorac Dis. 2019;11(Suppl 11):S1528–37.
Mekontso-Dessap A, Castelain V, Anguel N, Bahloul M, Schauvliege F, Richard C, Teboul JL. Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med. 2002;28(3):272–7.
Dubin A, Pozo MO, Hurtado J. Central venous minus arterial carbon dioxide pressure to arterial minus central venous oxygen content ratio as an indicator of tissue oxygenation: a narrative review. Rev Bras Ter Intensiva. 2020;32(1):115–22.
Van Regenmortel N, Verbrugghe W, Roelant E, Van den Wyngaert T, Jorens PG. Maintenance fluid therapy and fluid creep impose more significant fluid, sodium, and chloride burdens than resuscitation fluids in critically ill patients: a retrospective study in a tertiary mixed ICU population. Intensive Care Med. 2018;44(4):409–17.
Silversides JA, McAuley DF, Blackwood B, Fan E, Ferguson AJ, Marshall JC. Fluid management and deresuscitation practices: a survey of critical care physicians. J Intensive Care Soc. 2020;21(2):111–8.
Malbrain M, Martin G, Ostermann M. Everything you need to know about deresuscitation. Intensive Care Med. 2022;48(12):1781–6.
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Martin G, Huber W, Malbrain ML. Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Ann Intensive Care. 2012;2(Suppl 1):S15.
Monnet X, Cipriani F, Camous L, Sentenac P, Dres M, Krastinova E, Anguel N, Richard C, Teboul JL. The passive leg raising test to guide fluid removal in critically ill patients. Ann Intensive Care. 2016;6(1):46.
Huang D, Ma H, Ma J, Hong L, Lian X, Wu Y, Wu Y, Wang S, Qin T, Tan N. A novel supplemental maneuver to predict fluid responsiveness in critically ill patients: blood pump-out test performed before renal replacement therapy. Ann Transl Med. 2020;8(12):786.
Acknowledgements
Not applicable
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
XM, CL and J-LT wrote the original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate:
Not applicable
Consent for publication:
Not applicable
Competing interests
XM is a member of the Medical Advisory Board of Pulsion Medical Systems, Getinge, he received fees for scientific lectures from Pulsion Medical Systems, Getinge and Baxter, and limited research grants from Pulsion Medical Systems, Getinge. CL received fees for lectures from Sedana Medical. J-LT is a member of the Medical Advisory Board of Pulsion Medical Systems, Getinge, he received fees for scientific lectures from Pulsion Medical Systems, Getinge, and limited research grants from Pulsion Medical Systems, Getinge.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Monnet, X., Lai, C. & Teboul, JL. How I personalize fluid therapy in septic shock?. Crit Care 27, 123 (2023). https://doi.org/10.1186/s13054-023-04363-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04363-3