Abstract
Background
There is conflicting clinical evidence whether platelet-rich plasma (PRP) therapies could translate to an increased meniscus healing rate and improved functional outcomes. The objective of this systematic review and meta-analysis was to compare the failure rate and patient-reported functional outcomes in meniscus repair augmented with and without PRP.
Methods
We comprehensively searched the PubMed, Web of Science, Medline, Embase, and Cochrane Library databases to identify studies that compared the clinical efficacy of meniscus repair performed with PRP versus without PRP. The primary outcome was the meniscus repair failure rate, while the secondary outcomes were knee-specific patient-reported outcomes, including the International Knee Documentation Committee (IKDC) score, Lysholm knee scale, visual analog scale, Tegner activity level score, Western Ontario and McMaster Universities Osteoarthritis Index score, Single Assessment Numeric Evaluation score, and Knee injury and Osteoarthritis Outcome Score. Furthermore, subgroup analyses were performed by stratifying the studies according to the PRP preparation technique to investigate the potential sources of heterogeneity among studies.
Results
Our meta-analysis included nine studies (two RCTs and seven non-RCTs) with 1164 participants. The failure rate in the PRP group was significantly lower than that in the non-PRP group [odds ratio: 0.64, 95% confidence interval (CI) (0.42, 0.96), P = 0.03]. Furthermore, the PRP group was associated with a statistically significant improvement in the visual analog scale for pain [Mean difference (MD): − 0.76, 95% CI (− 1.32, − 0.21), P = 0.007] and Knee injury and Osteoarthritis Outcome Score-symptom [MD: 8.02, 95% CI (2.99, 13.05), P = 0.002] compared with the non-PRP group. However, neither the IKDC score nor the Lysholm knee scale showed any differences between the two groups. In addition, the results of subgroup analyses favored PRP over platelet-rich fibrin matrix (PRFM) regarding the IKDC score.
Conclusions
Although meniscus repairs augmented with PRP led to significantly lower failure rates and better postoperative pain control compared with those of the non-PRP group, there is insufficient RCT evidence to support PRP augmentation of meniscus repair improving functional outcomes. Moreover, PRP could be recommended in meniscus repair augmentation compared with PRFM. PRFM was shown to have no benefit in improving functional outcomes.
Similar content being viewed by others
Introduction
The menisci are fibrocartilaginous structures in the tibiofemoral joint. A complete meniscus structure has the functions of lubrication, nutrition, joint stability, shock absorption, and load transmission during dynamic movements [1, 2]. Meniscus injury is thought to be a unique challenge because of the absence of healing at the avascular zone, the instability of the knee joint, the accelerated degeneration of articular cartilage, and the increased rate of early-onset osteoarthritis [3, 4]. At present, it is the consensus that meniscus repair or stimulation of meniscus regeneration in the treatment of meniscus injury could potentially prevent or delay osteoarthritis onset [5]. However, the improvement of regeneration and the increase in the healing rate after injury have been significant challenges.
Platelet-rich plasma (PRP) is defined as an autologous blood-derived product that contains highly concentrated platelets, associated growth factors, and other bioactive components [6]. PRP has been demonstrated to display positive effects on tissue healing by stimulating cell proliferation, cell migration, angiogenesis, and extracellular matrix production in numerous cell types in both in vitro and in vivo models [7, 8]. Despite a paucity of large-scale clinical evidence to support the use of PRP therapy, there has been widespread application for various musculoskeletal injuries involving tendon, ligament, cartilage, and/or bone owing to the enthusiasm regarding its potential [9,10,11,12]. Many PRP growth factors, including platelet-derived growth factor and transforming growth factor beta, have been shown to modulate the inflammatory process and regulate chondrocyte viability, contributing to tissue maintenance and meniscus repair [13,14,15]. Furthermore, various clinical studies have verified that PRP injection provided good functional scores and radiological improvement in the patients with symptomatic meniscal lesions [1, 16,17,18]. By contrast, several retrospective comparative studies showed that there were no significant improvements in pain relief or functional improvement on PRP application in meniscus repair [19,20,21].
Consequently, the effectiveness of PRP for meniscus repair is greatly debated. Although there have been three published systematic review studies on PRP augmentation in meniscus repair treatment [22,23,24], their major limitations were that they included only a few studies with a limited number of patients as well as studies with heterogeneity of different PRP preparations. Therefore, the aim of present investigation was to systematically review and perform a meta-analysis of the literature to investigate PRP efficacy in meniscus repair, including the most recent matched case–control studies [25, 26]. In addition, different forms of PRP preparations were evaluated by subgroup analyses.
Methods
Literature search and selection criteria
Our systematic review and meta-analysis were performed in the PROSPERO registration (No. 300489). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used. Two independent reviewers performed the literature search in accordance with the PRISMA guidelines and reviewed the search results. The PubMed, Web of Science, Medline, Embase, and the Cochrane Library databases were systematically searched. No publication date restriction was applied. To include all the articles about the clinical efficacy of meniscus repair performed with PRP, a structured literature search was applied using the following string: ((“PRP” OR “platelet-rich plasma” OR “plasma-rich fibrin”) AND (“meniscus” OR “menisci” OR “meniscal”)).
The adopted inclusion criteria were as follows: (1) original articles; (2) comparative studies involving meniscus repair with or without PRP augmentation; (3) the studies were analyzed with at least one of the following outcomes: visual analog scale (VAS) scores, meniscus repair failures and knee-specific patient-reported outcome scores; and (4) full-text articles available in English. Exclusion criteria were as follows: (1) studies including patients undergoing other surgical treatments unrelated to meniscus repair; (2) PRP not the sole difference between the experimental and the control group; (3) animal studies, basic science investigations, review articles, or technique papers; and (4) articles published in other languages. We retrieved the full texts of eligible studies, and only the most recent or the single article provided with the most information was included when duplicates were identified.
Data extraction and quality assessment
The following data from studies were extracted by two independent reviewers: the first author’s name, publication year, country, sample size, type and dosage of PRP implementation, follow-up time, and the characteristics of the study population. Clinical outcomes recorded were the meniscus repair failure rate and knee-specific patient-reported outcomes: International Knee Documentation Committee (IKDC) score, Lysholm knee scale, VAS scores for pain, Tegner activity level score, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, Single Assessment Numeric Evaluation (SANE) score, and Knee injury and Osteoarthritis Outcome Score (KOOS). PRP preparations were classified into four subtypes: leukocyte-poor (LP) pure PRP, leukocyte-rich (LR) pure PRP, LP platelet-rich fibrin matrix (PRFM), and LR PRFM [27]. Studies were defined as LP/LR or PRP/PRFM by the manufacturers’ specifications and whether they had more or fewer leukocytes than autologous blood. Where requisite data were lacking in the publications, the original investigators were contacted.
The Newcastle-Ottawa Quality Assessment Scale (NOS) was used for assessing non-randomized studies with the following three broad categories: selection (S1: Definition of cases; S2: Representativeness of the cases; S3: Selection of controls; S4: Adequate control definition), comparability (C1: Comparability of cases; C2: Study controls for the basis of the analysis), and exposure (E1: Ascertainment of the exposure; E2: Ascertainment of the same method used for cases and controls; E3: Non-response rate) [28]. This scale is assigned from 0 to 9 points, with studies scoring below 6 points considered low quality, 6 and 7 points represent moderate quality, while 8 and 9 points indicate high quality [29]. The quality of randomized controlled trials (RCTs) was assessed by the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions, including the following items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias.
Statistical analysis
Meta-analysis was conducted in Review Manager (RevMan Version 5.4, The Cochrane Collaboration, Oxford, UK) and STATA version 14.0 (Stata Corporation; College Station, TX, USA). Continuous outcomes were addressed as standardized mean differences (MDs), and the dichotomous data were expressed as odds ratios (ORs). The effect sizes were reported with 95% confidence intervals (95% CIs). Heterogeneity of an article was estimated by the chi-squared test and I2 statistic. If in the chi-squared test P < 0.1 or the I2 statistic > 50%, heterogeneity was considered to be significant, and a random effect model was used to decrease the impact of heterogeneity on the results in this situation. Otherwise, a fixed-effects model was applied for the meta-analysis. Sensitivity analyses and subgroup analyses were conducted to investigate possible sources of heterogeneity and the stability of the results. P values of < 0.05 were considered to be statistically significant.
Results
Study selection
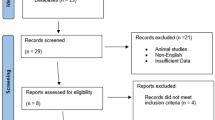
Our search strategy initially identified 220 possible studies, and no additional records were found during manual searches of references. After removing 88 duplicate studies, a total of 116 records were excluded because they were deemed irrelevant according to the title and abstract. After thoroughly reviewing the full texts of the 16 potentially eligible articles, nine articles (two RCTs and seven non-RCTs) were selected for the final analysis, which were published between 2015 and 2021 [19, 20, 25, 26, 30,31,32,33,34]. A flowchart depicting the study selection strategy is shown in Fig. 1.
Study characteristics and quality assessment
Nine articles with 1164 participants were included in this systematic review: 519 augmented with PRP (experimental group) and 645 without PRP (control group). All participants were diagnosed with meniscal injuries based on physical examination, magnetic resonance imaging (MRI), or arthroscopy at the time of surgery. In addition, the treatment options and PRP preparation and administration varied among the enrolled studies. We identified six studies in which PRP was delivered arthroscopically and sutured or injected into the repair site [19, 20, 25, 31,32,33], one study with in situ PRP injection into the repaired lesion after mini-arthrotomy [30], one study with multiple intra-articular PRP injections after meniscus repair surgery [26], and one study with minimally invasive (percutaneous) intrameniscal PRP application [34]. Furthermore, there were seven studies using LR-PRP, with two other studies not specifying LR versus LP formulations [20, 26]. Two studies utilized PRP with a fibrin matrix [20] or clot [32] that was inserted into the repair site. The remaining seven studies injected thrombin-activated PRP into the meniscus repair site. Detailed information about the baseline and characteristics are presented in Table 1.
Following the instructions in the Cochrane Handbook for Systematic Reviews of Interventions, five aspects related to the risk of bias were assessed in two RCTs [31, 34], including allocation, blinding, incomplete outcome data, selective reporting, and other potential sources of bias. In both these RCT studies, the patients, data collectors, and assessors were blinded and the random component in the sequence generation process was described. All participant exclusions and excessive drop-out in each study were reported. The results of the NOS for the quality of the seven non-RCTs are presented in Table 2. Five studies were graded as good [19, 25, 26, 30, 32] and two graded as fair [20, 33]. In particular, the studies by Griffin et al. and Everhart et al. [20, 33] were deemed problematic because they lacked the representativeness of the cases and did not take adequate actions to avoid bias in the study analysis.
Failure rate
A total of 708 patients from seven studies were considered to display repair failure when they developed a recurrence of meniscal symptoms and requirement for reoperation, or this was shown when evaluated by second-look arthroscopy or MRI postoperatively [19, 20, 26, 30, 31, 33, 34]. In the PRP group, 16.7% of patients experienced treatment failure, while in the control group, this was 21.6%. The result of the meta-analysis showed that the failure rate in the PRP group was significantly lower than that in the control group (OR: 0.64, 95% CI [0.42, 0.96], P = 0.03). There was low heterogeneity in the outcomes between the groups (P = 0.48, I2 = 0%) (Table 3, Fig. 2).
Patient-reported outcomes
The VAS score for pain was reported in three studies, with 75 patients treated with PRP and 63 with a control [19, 31, 34]. There was a statistically significant difference favoring PRP [MD: − 0.76, 95% CI (− 1.32, − 0.21), P = 0.007]. Random effects models were used because of statistical heterogeneity through meta-analysis (P = 0.10 and I2 = 57%). However, because the number of included studies was small, subgroup analyses were not performed (Table 3, Fig. 3).
The IKDC score was obtained from six studies involving 513 participants [20, 25, 26, 30,31,32]. The pooling results showed that the IKDC score was not significantly different between the PRP and control groups [MD: 0.66, 95% CI (0.27, 1.60), P = 0.16, I2 = 93%], and neither was the Lysholm knee scale [MD: − 0.13, 95% CI (− 0.78, 0.52), P = 0.70, I2 = 69%] (Table 3, Fig. 3). There was considerable heterogeneity among the studies. Sensitivity analysis did not detect the source of the heterogeneity, and we performed subgroup meta-analysis to investigate the possible sources of heterogeneity among the studies according to various confounding factors.
All five KOOS subscales, pain, symptom, activity of daily living (ADL), sport/recreation, and quality of life (QoL), were recorded in three studies, with 78 patients treated with PRR and 65 with a control [30, 31, 34]. When the data of all studies were pooled, there was a significant difference between the PRP group and controls in KOOS-symptom [MD: 8.02, 95% CI (2.99, 13.05), P = 0.002, I2 = 95%], while no significant differences were detected between the two groups regarding KOOS-pain, KOOS-ADL, KOOS-sport/recreation or KOOS-QoL [MD: 12.18, 95% CI (− 0.66, 25.03), P = 0.06; MD: 4.21, 95% CI (− 7.64, 16.07), P = 0.49; MD: 4.87, 95% CI (− 11.58, 21.31), P = 0.56; and MD: 4.78 95% CI (− 0.71, 10.28), P = 0.09, respectively]. Sensitivity analysis failed to eliminate heterogeneity, and random effects models were adopted for analysis (Table 3, Fig. 4).
Furthermore, the Tegner activity level score [32] and SANE score [25] were each applied in one study, neither of which found significant differences in self-reported knee function scores between the PRP and matched-control groups. The subjective WOMAC score was used in two studies [31, 34]. Of these, one study found significantly better scores in the PRP group (P = 0.002) [31], however, the other study showed no statistical difference between the two groups (Table 3) [34].
Subgroup analyses of the different varieties of PRP applications
Furthermore, subgroup analyses were performed to investigate the potential sources of heterogeneity among studies. This analysis was performed by stratifying the studies according to the PRP preparation technique. PRP and PRFM are both processed from autologous blood, but they differ in their preparation methods [35]. PRP is collected with anticoagulant and is immediately processed, whereas PRFM is collected immediately without anticoagulant, such that it forms a fibrin-rich clot that has to be sutured into the repair site or using a specialized delivery system.
Regarding the IKDC score, subgroup analysis showed that PRFM had no significant association with the IKDC score [MD: − 0.35, 95% CI (− 0.91, 0.21), P = 0.22]. However, a significant correlation between PRP and the IKDC score was observed [MD: 1.56, 95% CI (0.18, 2.94), P = 0.03]. In addition, we conducted subgroup analysis based upon the Lysholm knee scale. There was no significant association between the Lysholm knee scale and different preparation techniques of PRP [MD: 0.27, 95% CI (− 0.14, 0.69), P = 0.20] or PRFM [MD: − 0.69, 95% CI (− 1.47, 0.08), P = 0.08] (Fig. 5).
Discussion
Injuries to the menisci are the most common condition among knee joint-related morbidities, can hardly heal, and frequently progress into structural breakdown, followed by the initiation of osteoarthritis [36]. With the importance of the meniscus in joint function and diseases becoming recognized, there is a need for an accelerated and performant healing strategy [37]. Biologic augmentation techniques, including PRP, have gained significant interest as viable treatment options to enhance repair healing following meniscus injury [23]. Some basic science and clinical studies have suggested that PRP is gaining increasing attention as an adjuvant for meniscus repair and its safety has been established, whereas other studies have shown the opposite regarding the repair [25, 38]. Therefore, in the present systematic review and meta-analysis, which was based on nine studies with 1164 participants, the results showed a trend that PRP augmentation could reduce the repair failure rate and provide better postoperative pain control. However, there were no significant differences with regard to most of the patient-reported functional outcomes. The results of subgroup analyses favored PRP over PRFM regarding the improvement of functional outcomes.
The beneficial effect of PRP on the meniscus repair failure rate is supported by prior basic science research, because an in vitro and animal study of PRP found the therapy to increase the concentration of various growth factors and upregulate the viability of meniscal cells [8, 14, 39]. Many in vitro studies have demonstrated that the injection of various growth factors could stimulate meniscal tissue repair [40]. By supplying the injury site with a wide range of growth factors, including platelet-derived growth factor, vascular endothelial growth factor, and transforming growth factor beta, PRP promotes cell proliferation, migration, and extracellular collagen matrix formation not only in torn meniscus zones, but also in the entire joint environment [41, 42]. Synoviocytes are affected by platelet releasate, and meniscal cells appear to be induced by PRP and act synergically toward meniscus healing [39]. Consequently, the forest plots demonstrated that the failure rate of meniscus repair treatment in the PRP group improved significantly compared with that in the non-PRP group. Although a recent meta-analysis on the application of PRP in arthroscopic meniscus repair showed no significant difference in the failure rate [43], only three studies on the failure rate were included [19, 30, 33].
The effects of PRP on pain reduction have been previously observed in other studies and several authors have reported the analgesic properties of platelets [44, 45]. Postoperative pain was mainly induced by inflammation [46]. Inflammatory factors (such as interleukin-1β, interleukin-6, and tumor necrosis factor-α) are released after surgery, which decrease the nociceptor threshold and play an important role in the occurrence of pain [47, 48]. PRP involves the modulation of the meniscal environment by introducing autologous blood products into the targeted tissue, and the growth factors contained in the PRP concentrate can lead to the inhibition of the local inflammatory response and promote chondrogenesis. Moreover, PRP reduces pain by influencing the expression of mediators (such as prostaglandin E2, substance P, dopamine, and 5-hydroxy-tryptamine) [49]. Consequently, our pooled results showed that the postoperative pain VAS scores of the PRP group were significantly lower than those of the control group.
However, the functional outcomes showed no significant difference between the groups regarding KOOS-pain, KOOS-ADL, KOOS-sport/recreation, or KOOS-QoL, except for KOOS-symptom. Neither the IKDC score nor the Lysholm knee scale showed any difference between the non-PRP and PRP groups, which was consistent with previous systematic reviews [22, 23]. Heterogeneity could be the acknowledged significant limitation that resulted from a lack of standardization in PRP dosing and preparation, however, there was no further investigation of this in previous systematic reviews. Therefore, subgroup analyses were firstly performed to evaluate the different PRP preparation systems in our study. Significant correlation of the IKDC score was demonstrated in the PRP subgroup analysis, but no significant correlations were found in the PRFM subgroup analysis.
Consequently, PRP should be recommended instead of PRFM in meniscus repair augmentation. Although positive anabolic effects of PRFM on meniscocytes harvested from the primary culture of a rabbit meniscus were demonstrated [50], PRFM may do the opposite and inhibit meniscus healing. PRFM is a PRP variant whereby a fibrin matrix is formed by activation of the fibrin-clotting cascade, which has to be sutured into the repair site or applied using the fateful rod system, which is a novel device used to deliver platelet-rich fibrin into the joint [20, 32]. As a consequence, the space-occupying effect of fibrin clot in PRFM may result in a gap at the repair site after it dissolves. Additionally, PRFM is known to increase the presence of inflammatory mediators at the repair site [51]. Therefore, fibrovascular scar tissue may have contributed to the initially stronger biomechanical properties of the repair without improving the structural properties with respect to collagen and cartilage organization [52, 53]. Rodeo et al. found that autologous PRFM applied to the tendon-bone interface at the time of surgery did not have a positive effect on the healing tendon-bone interface, tendon vascularity, muscle strength, or shoulder symptoms. Indeed, regression analysis suggested that PRFM may have an inhibitory effect on tendon healing [53], which was consistent with our study that PRFM has been shown to have no benefit in improving functional outcomes.
Moreover, the effect of the leukocyte counts on tissue healing remains greatly debated. Recent research was performed to ascertain whether there was evidence to support the use of LP- or LR-PRP as an adjunct to arthroscopic rotator cuff repair [54]. However, significant differences in platelet concentrations between various commercially produced PRP media remain a confounding variable and make broad generalizations between LR- and LP-PRP based solely on leukocytes impossible [55]. In the present systematic review, there were seven studies utilizing LR-PRP, with two other studies not specifying LR versus LP formulations. Because no studies in this review compared LR- and LP-PRP, no conclusions can be made as to the relative effects. Therefore, we suggest that further studies should be performed to ascertain whether there is evidence to support the use of LP- or LR-PRP as an adjunct to meniscus repair augmentation.
To our knowledge, the present study is the meta-analysis with the largest number of participants to evaluate the use of PRP in meniscus repair treatment. Additional information regarding the heterogeneity issues was obtained by subgroup analyses on the PRP preparation. However, there were still several limitations in our study. First and foremost, the few RCT studies included in this review limit the strength of the conclusions. Second, there is a multitude of confounding factors that may affect the results in our meta-analysis, and this was due to the different types of meniscal injury, repair therapies, and operative technique and the different forms and dosages of PRP applications. Third, because there was an insufficient number of eligible studies, we did not conduct subgroup or meta-regression analyses for the different PRP types, preparations, or applications.
Conclusions
Although the studies were mostly non-randomized, meniscus repairs augmented with PRP led to significantly lower failure rates and subsequently improved postoperative pain control when compared with repairs without PRP. However, most studies reported no significant differences in patient-reported outcome scores. The findings of our meta-analysis suggest that PRP could be recommended in patients requiring meniscus repair instead of PRFM. In addition, adequately powered prospective randomized trials are needed to further investigate the efficacy of different forms of PRP on meniscus repair treatment because current evidence is limited to small, mostly non-randomized studies and there is a lack of consensus.
Availability of data and materials
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PRP:
-
Platelet-rich plasma
- PRFM:
-
Platelet-rich fibrin matrix
- LP:
-
Leukocyte-poor
- LR:
-
Leukocyte-rich
- RCTs:
-
Randomized controlled trials
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- VAS:
-
Visual analog scale
- IKDC:
-
International knee documentation committee
- SANE:
-
Single assessment numeric evaluation
- KOOS:
-
Knee injury and osteoarthritis outcome score
- ADL:
-
Activity of daily living
- QoL:
-
Quality of life
- WOMAC:
-
Western Ontario and McMaster universities osteoarthritis index
- NOS:
-
Newcastle-Ottawa quality assessment scale
- ORs:
-
Odds ratios
- CI:
-
Confidence interval
- MD:
-
Mean difference
- MRI:
-
Magnetic resonance imaging
References
Guenoun D, Magalon J, de Torquemada I, Vandeville C, Sabatier F, Champsaur P, et al. Treatment of degenerative meniscal tear with intrameniscal injection of platelets rich plasma. Diagn Interv Imaging. 2020;101(3):169–76. https://doi.org/10.1016/j.diii.2019.10.003.
Fox AJS, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28(2):269–87. https://doi.org/10.1002/ca.22456.
Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, et al. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1177–94. https://doi.org/10.1007/s00167-020-05847-3.
Verdonk R, Madry H, Shabshin N, Dirisamer F, Peretti GM, Pujol N, et al. The role of meniscal tissue in joint protection in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1763–74. https://doi.org/10.1007/s00167-016-4069-2.
Di Matteo B, Altomare D, Garibaldi R, La Porta A, Manca A, Kon E. Ultrasound-guided meniscal injection of autologous growth factors: a brief report. Cartilage. 2021. https://doi.org/10.1177/19476035211037390.
Kurnaz R, Balta O. Effect of platelet-rich plasma and platelet-rich fibrin matrix on healing of vertical meniscal tears in a rabbit model. Acta Orthop Traumatol Turc. 2020;54(2):186–95. https://doi.org/10.5152/j.aott.2020.02.20.
Freymann U, Metzlaff S, Krüger J-P, Hirsh G, Endres M, Petersen W, et al. Effect of human serum and 2 different types of platelet concentrates on human meniscus cell migration, proliferation, and matrix formation. Arthroscopy. 2016;32(6):1106–16. https://doi.org/10.1016/j.arthro.2015.11.033.
Wang C-C, Lee C-H, Peng Y-J, Salter DM, Lee H-S. Platelet-rich plasma attenuates 30-kDa fibronectin fragment-induced chemokine and matrix metalloproteinase expression by meniscocytes and articular chondrocytes. Am J Sports Med. 2015;43(10):2481–9. https://doi.org/10.1177/0363546515597489.
Zhang JY, Fabricant PD, Ishmael CR, Wang JC, Petrigliano FA, Jones KJ. Utilization of platelet-rich plasma for musculoskeletal injuries: an analysis of current treatment trends in the United States. Orthop J Sports Med. 2016;4(12):2325967116676241. https://doi.org/10.1177/2325967116676241.
Karjalainen TV, Silagy M, O’Bryan E, Johnston RV, Cyril S, Buchbinder R. Autologous blood and platelet-rich plasma injection therapy for lateral elbow pain. Cochrane Datab Syst Rev. 2021;9:CD010951. https://doi.org/10.1002/14651858.
Lv Z-T, Zhang J-M, Pang Z-Y, Wang Z, Huang J-M, Zhu W-T. The efficacy of platelet rich plasma on anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Platelets. 2021. https://doi.org/10.1080/09537104.2021.1902969.
Li Y, Li T, Li J, Tang X, Li R, Xiong Y. Platelet-rich plasma has better results for retear rate, pain, and outcome than platelet-rich fibrin after rotator cuff repair: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2021. https://doi.org/10.1016/j.arthro.2021.05.023.
Sakata R, Reddi AH. Platelet-rich plasma modulates actions on articular cartilage lubrication and regeneration. Tissue Eng Part B Rev. 2016;22(5):408–19.
Qi Y, Tang R, Shi Z, Feng G, Zhang W. Wnt5a/Platelet-rich plasma synergistically inhibits IL-1β-induced inflammatory activity through NF-κB signaling pathway and prevents cartilage damage and promotes meniscus regeneration. J Tissue Eng Regen Med. 2021;15(7):612–24. https://doi.org/10.1002/term.3198.
Freymann U, Degrassi L, Krüger JP, Metzlaff S, Endres M, Petersen W. Effect of serum and platelet-rich plasma on human early or advanced degenerative meniscus cells. Connect Tissue Res. 2017;58(6):509–19. https://doi.org/10.1080/03008207.2016.1260563.
Mitev K, Longurov A. Intra-articular platelet-rich plasma injections for treating knee pain associated with articular cartilage and degenerative meniscal lesions. Open Access Maced J Med Sci. 2019;7(15):2484–7. https://doi.org/10.3889/oamjms.2019.674.
Özyalvaç ON, Tüzüner T, Gürpinar T, Obut A, Acar B, Akman YE. Radiological and functional outcomes of ultrasound-guided PRP injections in intrasubstance meniscal degenerations. J Orthop Surg (Hong Kong). 2019;27(2):2309499019852779. https://doi.org/10.1177/2309499019852779.
Alessio-Mazzola M, Felli L, Trentini R, Formica M, Capello AG, Lovisolo S, et al. Efficacy of autologous platelet-rich plasma injections for grade 3 symptomatic degenerative meniscal lesions: a 1-year follow-up prospective study. Sports Health. 2021. https://doi.org/10.1177/19417381211011074.
Dai W-L, Zhang H, Lin Z-M, Shi Z-J, Wang J. Efficacy of platelet-rich plasma in arthroscopic repair for discoid lateral meniscus tears. BMC Musculoskelet Disord. 2019;20(1):113. https://doi.org/10.1186/s12891-019-2500-9.
Griffin JW, Hadeed MM, Werner BC, Diduch DR, Carson EW, Miller MD. Platelet-rich plasma in meniscal repair: Does augmentation improve surgical outcomes? Clin Orthop Relat Res. 2015;473(5):1665–72. https://doi.org/10.1007/s11999-015-4170-8.
Hutchinson ID, Rodeo SA, Perrone GS, Murray MM. Can platelet-rich plasma enhance anterior cruciate ligament and meniscal repair? J Knee Surg. 2015;28(1):19–28. https://doi.org/10.1055/s-0034-1387166.
Haunschild ED, Huddleston HP, Chahla J, Gilat R, Cole BJ, Yanke AB. Platelet-rich plasma augmentation in meniscal repair surgery: a systematic review of comparative studies. Arthroscopy. 2020;36(6):1765–74. https://doi.org/10.1016/j.arthro.2020.01.038.
Belk JW, Kraeutler MJ, Thon SG, Littlefield CP, Smith JH, McCarty EC. Augmentation of meniscal repair with platelet-rich plasma: a systematic review of comparative studies. Orthop J Sports Med. 2020;8(6):2325967120926145. https://doi.org/10.1177/2325967120926145.
Sochacki KR, Safran MR, Abrams GD, Donahue J, Chu C, Sherman SL. Platelet-rich plasma augmentation for isolated arthroscopic meniscal repairs leads to significantly lower failure rates: a systematic review of comparative studies. Orthop J Sports Med. 2020;8(11):2325967120964534. https://doi.org/10.1177/2325967120964534.
Bailey L, Weldon M, Kleihege J, Lauck K, Syed M, Mascarenhas R, et al. Platelet-rich plasma augmentation of meniscal repair in the setting of anterior cruciate ligament reconstruction. Am J Sports Med. 2021;49(12):3287–92. https://doi.org/10.1177/03635465211036471.
Yang C-P, Hung K-T, Weng C-J, Chen AC-Y, Hsu K-Y, Chan Y-S. Clinical outcomes of meniscus repair with or without multiple intra-articular injections of platelet rich plasma after surgery. J Clin Med. 2021. https://doi.org/10.3390/jcm10122546.
Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang C-Q, Pinto NR, Bielecki T. Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014;4(1):3–9.
Quigley JM, Thompson JC, Halfpenny NJ, Scott DA. Critical appraisal of nonrandomized studies-a review of recommended and commonly used tools. J Eval Clin Pract. 2019;25(1):44–52. https://doi.org/10.1111/jep.12889.
Drew MK, Finch CF. The relationship between training load and injury, illness and soreness: a systematic and literature review. Sports Med. 2016;46(6):861–83. https://doi.org/10.1007/s40279-015-0459-8.
Pujol N, Salle De Chou E, Boisrenoult P, Beaufils P. Platelet-rich plasma for open meniscal repair in young patients: any benefit? Knee Surg Sports Traumatol Arthrosc. 2015;23(1):51–8. https://doi.org/10.1007/s00167-014-3417-3.
Kaminski R, Kulinski K, Kozar-Kaminska K, Wielgus M, Langner M, Wasko MK, et al. A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. Biomed Res Int. 2018;2018:9315815. https://doi.org/10.1155/2018/9315815.
Kemmochi M, Sasaki S, Takahashi M, Nishimura T, Aizawa C, Kikuchi J. The use of platelet-rich fibrin with platelet-rich plasma support meniscal repair surgery. J Orthop. 2018;15(2):711–20. https://doi.org/10.1016/j.jor.2018.05.006.
Everhart JS, Cavendish PA, Eikenberry A, Magnussen RA, Kaeding CC, Flanigan DC. Platelet-rich plasma reduces failure risk for isolated meniscal repairs but provides no benefit for meniscal repairs with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(8):1789–96. https://doi.org/10.1177/0363546519852616.
Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-term outcomes of percutaneous trephination with a platelet rich plasma intrameniscal injection for the repair of degenerative meniscal lesions. A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20040856.
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 2009;27(3):158–67. https://doi.org/10.1016/j.tibtech.2008.11.009.
Tarafder S, Park G, Lee CH. Explant models for meniscus metabolism, injury, repair, and healing. Connect Tissue Res. 2020;61(3–4):292–303. https://doi.org/10.1080/03008207.2019.1702031.
Yan W, Dai W, Cheng J, Fan Y, Wu T, Zhao F, et al. Advances in the mechanisms affecting meniscal avascular zone repair and therapies. Front Cell Dev Biol. 2021;9: 758217. https://doi.org/10.3389/fcell.2021.758217.
Sheean AJ, Anz AW, Bradley JP. Platelet-rich plasma: fundamentals and clinical applications. Arthroscopy. 2021;37(9):2732–4. https://doi.org/10.1016/j.arthro.2021.07.003.
Filardo G, Kon E, Roffi A, Di Matteo B, Merli ML, Marcacci M. Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2459–74. https://doi.org/10.1007/s00167-013-2743-1.
Scotti C, Hirschmann MT, Antinolfi P, Martin I, Peretti GM. Meniscus repair and regeneration: review on current methods and research potential. Eur Cell Mater. 2013;26:150–70. https://doi.org/10.22203/ecm.v026a11.
Wang S-Z, Rui Y-F, Tan Q, Wang C. Enhancing intervertebral disc repair and regeneration through biology: platelet-rich plasma as an alternative strategy. Arthritis Res Ther. 2013;15(5):220. https://doi.org/10.1186/ar4353.
Hajipour H, Farzadi L, Latifi Z, Keyhanvar N, Navali N, Fattahi A, et al. An update on platelet-rich plasma (PRP) therapy in endometrium and ovary related infertilities: clinical and molecular aspects. Syst Biol Reprod Med. 2021;67(3):177–88. https://doi.org/10.1080/19396368.2020.1862357.
Migliorini F, Cuozzo F, Cipollaro L, Oliva F, Hildebrand F, Maffulli N. Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: a meta-analysis. J Orthop Traumatol. 2022;23(1):8. https://doi.org/10.1186/s10195-022-00630-1.
Moretti L, Maccagnano G, Coviello M, Cassano GD, Franchini A, Laneve A, et al. Platelet rich plasma injections for knee osteoarthritis treatment: a prospective clinical study. J Clin Med. 2022;11(9):2640. https://doi.org/10.3390/jcm11092640.
Guillibert C, Charpin C, Raffray M, Benmenni A, Dehaut FX, El Ghobeira G, et al. Single injection of high volume of autologous pure PRP provides a significant improvement in knee osteoarthritis: a prospective routine care study. Int J Mol Sci. 2019;20(6):1327. https://doi.org/10.3390/ijms20061327.
Memtsoudis SG, Valle AGD, Jules-Elysse K, Poultsides L, Reid S, Starcher B, et al. Perioperative inflammatory response in total knee arthroplasty patients: impact of limb preconditioning. Reg Anesth Pain Med. 2010;35(5):412–6. https://doi.org/10.1097/aap.0b013e3181e82e8e.
Rabbitts JA, Palermo TM, Lang EA. A conceptual model of biopsychosocial mechanisms of transition from acute to chronic postsurgical pain in children and adolescents. J Pain Res. 2020;13:3071–80. https://doi.org/10.2147/JPR.S239320.
Barkai O, Puig S, Lev S, Title B, Katz B, Eli-Berchoer L, et al. Platelet-derived growth factor activates nociceptive neurons by inhibiting M-current and contributes to inflammatory pain. Pain. 2019;160(6):1281–96. https://doi.org/10.1097/j.pain.0000000000001523.
Kon E, Di Matteo B, Delgado D, Cole BJ, Dorotei A, Dragoo JL, et al. Platelet-rich plasma for the treatment of knee osteoarthritis: an expert opinion and proposal for a novel classification and coding system. Expert Opin Biol Ther. 2020;20(12):1447–60. https://doi.org/10.1080/14712598.2020.1798925.
Wong C-C, Kuo T-F, Yang T-L, Tsuang Y-H, Lin M-F, Chang C-H, et al. Platelet-rich fibrin facilitates rabbit meniscal repair by promoting meniscocytes proliferation, migration, and extracellular matrix synthesis. Int J Mol Sci. 2017. https://doi.org/10.3390/ijms18081722.
Hasan S, Weinberg M, Khatib O, Jazrawi L, Strauss EJ. The effect of platelet-rich fibrin matrix on rotator cuff healing in a rat model. Int J Sports Med. 2016;37(1):36–42. https://doi.org/10.1055/s-0035-1554637.
Rodeo SA, Potter HG, Kawamura S, Turner AS, Kim HJ, Atkinson BL. Biologic augmentation of rotator cuff tendon-healing with use of a mixture of osteoinductive growth factors. J Bone Joint Surg Am. 2007;89(11):2485–97. https://doi.org/10.2106/JBJS.C.01627.
Rodeo SA, Delos D, Williams RJ, Adler RS, Pearle A, Warren RF. The effect of platelet-rich fibrin matrix on rotator cuff tendon healing: a prospective, randomized clinical study. Am J Sports Med. 2012;40(6):1234–41. https://doi.org/10.1177/0363546512442924.
Hurley ET, Colasanti CA, Anil U, Luthringer TA, Alaia MJ, Campbell KA, et al. The effect of platelet-rich plasma leukocyte concentration on arthroscopic rotator cuff repair: a network meta-analysis of randomized controlled trials. Am J Sports Med. 2021;49(9):2528–35. https://doi.org/10.1177/0363546520975435.
Dragoo JL, Braun HJ, Durham JL, Ridley BA, Odegaard JI, Luong R, et al. Comparison of the acute inflammatory response of two commercial platelet-rich plasma systems in healthy rabbit tendons. Am J Sports Med. 2012;40(6):1274–81. https://doi.org/10.1177/0363546512442334.
Acknowledgements
None.
Funding
This study was funded by the National Key R&D Program of China (2018YFF0301105) and the National Natural Science Foundation of China (No. 81630064 and 81871786).
Author information
Authors and Affiliations
Contributions
ZL contributed to study conception and design, data analysis and interpretation, and a draft of the manuscript. XW contributed to the literature search and critical revision of the manuscript. Both authors have approved the final version to be submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Weng, X. Platelet-rich plasma use in meniscus repair treatment: a systematic review and meta-analysis of clinical studies. J Orthop Surg Res 17, 446 (2022). https://doi.org/10.1186/s13018-022-03293-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03293-0