Abstract
Background
The current study aims to evaluate the nipple and skin sensation following nipple-sparing mastectomy (NSM) and identify patient-, surgical-, or treatment-related factors affecting nipple or skin sensation in this cohort.
Methods
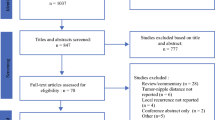
Patients who received NSM with postoperative nipple and skin sensation test evaluation at a single institution over the past 10 years were retrospectively retrieved from a prospectively collected breast cancer surgery database.
Results
A total of 460 NSM procedures were included in this current study, with the mean age of 48.3 ± 9.1. Three-hundred eighty-three (83.3%) patients had breast reconstructions. One-hundred seventy-four (37.8%) received conventional NSM (C-NSM), 195 (42.4%) endoscopic-assisted NSM (E-NSM), and 91 (19.8%) robotic-assisted NSM (R-NSM) procedures. For nipple sensation assessment, 15 (3.3%) were grade 0, 83 (18.2%) grade I, 229 (49.7%) grade II, and 133 (28.9%) grade III (normal sensation), respectively, with mean grade score of 2.1 ± 0.7. The preserved (grade III) nipple sensation rate was 36.2% (63/174) in the C-NSM group, 26.7% (52/195) in the E-NSM group, and 19.7% (18/91) in the R-NSM group (P = 0.06). The “time since surgery to last evaluation” was significantly longer in the C-NSM group (45.6 ± 34 months) or E-NSM group (44.7 ± 35.8 months) as compared to R-NSM group (31.8 ± 16 months, P < 0.01). In multivariate analysis, peri-areolar incision showed higher grade of nipple sensation (OR: 2.1, P = 0.02) compared to upper outer quadrant incision, and longer follow-up time post-NSM showed significant improvement of nipple or skin sensation (> 60 months vs. ≦ 12 months: nipple odds ratio (OR) = 5.75, P < 0.01; skin, OR = 1.97, P < 0.05).
Conclusion
Our current analysis showed some factors to be related to postoperative nipple or skin sensation, and longer “time after surgery” was associated with significant improvement of nipple and skin sensation in patients who received NSM, regardless of the surgical approaches.
Synopsis
Our current analysis showed a significant portion of patients with decrease or loss of nipple or skin sensation after nipple-sparing mastectomy (NSM). Several factors associated with preserved nipple or skin sensation were identified, including age, surgical methods, surgical wound location, and association of time from surgery showing that improvement of partial nipple or skin sensation was evident after a longer follow-up.
Highlights
• Diminished or loss of nipple sensation had been reported in 10–75% of patients who received nipple-sparing mastectomy (NSM).
• “Time from surgery to last evaluation” was a significant factor associated with sensation recovery or preservation in nipple or skin sensation post NSM.
• Skin incisions and types of operations (conventional versus endoscopic or robotic assisted NSM) were highly correlated with nipple and skin sensation post-NSM.
• Nipple ischemia necrosis grading was unrelated to preserved or lost nipple sensation post-NSM.
• Post-mastectomy radiotherapy was not associated with nipple or skin sensation post-NSM.
Similar content being viewed by others
Introduction
Compared with skin-sparing mastectomy (SSM), patients who received nipple-sparing mastectomy (NSM) showed significantly improved aesthetic outcomes and quality of life (QoL) [1,2,3]. NSM is now increasingly adopted as one of the standards for patients undergoing mastectomy without nipple-areolar complex (NAC) involvement due to acceptable oncologic safety [4,5,6].
Diminished or loss of nipple sensation had been reported in 10–75% of patients post-NSM [7,8,9,10]. For this patient group, losing their nipple sensation despite NAC preservation would result in lower satisfaction and QoL than patients who received breast-conserving surgery [11].
Novel surgical techniques of NSM, like endoscopic- or robotic-assisted NSM (R-NSM), had shown a decreased risk of nipple ischemia necrosis [12, 13]. There has been a paucity of studies reporting on the effect of different surgical approaches on nipple or skin sensation post-surgery due to the relatively recent advent of these surgical methods in the past decade. One recently reported randomized controlled trial showed R-NSM to be significantly associated with better nipple sensation compared with conventional nipple-sparing mastectomy (C-NSM) [14]. Further studies or investigations on whether these novel NSM techniques result in better preservation of nipple or skin sensation compared with C-NSM is of utmost importance.
Compared to other research areas of NSM studies, sensation preservation or related factors were underreported. Some studies have reported nipple sensation loss post-NSM, but they were limited to a small number of patients which further limit risk factors analysis of nipple or skin sensation loss [14, 15]. Furthermore, it remains unclear whether the duration of “time since surgery” would result in the recovery of nipple or skin sensation [16, 17].
The aims of the current study were to evaluate the nipple and skin sensation status post-NSM and compared the impact of different surgical approaches, like robotic — versus endoscopic — or conventional NSM on sensation preservation. Further evaluation on the influence of “time since surgery” on the sensation of the nipple or skin and related risk factors would be performed as well.
Materials and methods
Patients
Patients who received NSM at Changhua Christian Hospital (CCH) from August 2011 to April 2022 were retrospectively retrieved from a prospectively collected breast cancer surgery database. Patients were invited to receive nipple and skin sensation tests during regular follow-up. Those without detailed clinicopathologic information or nipple and skin sensation evaluations were excluded. This study was approved by the Institutional Review Board of CCH (CCH IRB no.: 190414). All patients provided written informed consent.
Clinicopathologic factors, surgical approaches (C-NSM, E-NSM, or R-NSM), types of breast reconstructions, and surgical wound incisions were recorded. Degrees of nipple or skin sensation post-NSM were assessed during outpatient follow-up. The factors related to loss or preservation of nipple or skin sensation were identified. Patients who had received nipple or skin sensation tests more than once were used to test the recovery curve of nipple or skin sensation post-operation in a longitudinal follow-up.
The current research also performed a literature review of reported studies [1, 9, 13, 18,19,20,21,22] regarding nipple or skin sensation post-NSM. The study design and patient allocations are shown in Fig. 1.
Indications of NSM
NSM was indicated for breast cancer patients who opted for mastectomy but keen to preserve their NAC. Patients selected for NSM should have no gross involvement of NAC as evaluated preoperatively through clinical examinations and imaging studies (mammography, sonography, with or without breast magnetic resonance imaging). Patients with nipple involvement reported during intraoperative frozen sections were excluded from inclusion into the current study as the procedure was changed to SSM instead.
Nipple and skin sensation assessment
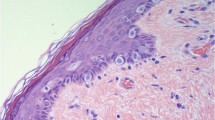
Patients who received NSM were followed up at the outpatient clinic and invited to have nipple and skin sensation tests by clinical study nurses according to the study protocol. The sensation assessment was first performed with finger touching the healthy contralateral side to demonstrate touch sensation of a normal breast. The same was then repeated on the nipple and skin of the operated side. Patients were then asked to score their sensation to touch of the nipple or area of the skin during an examination. Five areas of the measurement points were as follows: nipple, upper breast skin, medial breast skin, inferior breast skin, and lateral breast skin. Grading of the nipple or breast skin sensation was divided into four degrees (grade 0: no sensation at all, grade I: numbness sensation, grade II: fairly sensate, and grade III: normal sensation, Fig. 2).
Nipple and breast skin sensation test. The sensation assessment was first evaluated by finger touching the healthy side to show the feeling of touch sensation of a normal breast. Then perform the same touch on the operative side of the nipple and skin. Patients were asked to answer score of sensation when feeling the touch of the nipple or area of skin during an examination. Five area measurement points are as follows: the nipple, upper breast skin, medial breast skin, inferior breast skin, and lateral breast skin were tested, and the nipple or breast skin sensation were divided into four degrees (0–3): grade 0 (no sensation at all), grade I (numbness sensation), grade II (fairly sensate), and grade III (normal sensate)
Factors associated with nipple or skin sensation
Factors associated with the change in nipple sensation were identified by comparing patients with preserved nipple or skin sensation versus patients with decreased or lost nipple or skin sensation. Potential factors evaluated include patient-related characteristics, surgery-related factors, postoperative factors, and follow-up duration (time of operation to last performance of nipple or skin test). Patients were divided into retained nipple or skin sensation (grade III) versus diminished or loss sensation groups (grades II, I, and 0).
Type of skin incisions and operation methods
Common skin incisions used in the current study were upper-outer-oblique (radial), peri-areolar, single axillary, or lateral chest incisions. Operation methods for NSM used in the current study consisted of C-NSM, E-NSM, or R-NSM. C-NSM is usually performed via upper outer oblique (radial) incision or sometimes peri-areolar incision. Some E-NSM patients received dual-axillary-areolar incisions (categorized as peri-areolar incision) or single axillary or lateral chest incisions. R-NSM usually adopted a single axillary incision or lateral chest incision. The type of incisions and operation methods is as shown in Fig. 3.
Operation methods and skin incision types. Common skin incisions used in the current study were upper-outer-oblique (radial), peri-areolar, single axillary, or lateral chest incisions. Operation methods for NSM used in the current study included conventional NSM (C-NSM), endoscopic-assisted NSM (E-NSM), or robotic-assisted NSM (R-NSM). C-NSM is usually performed by upper outer oblique (radial) incision or sometimes peri-areolar incision. Some E-NSM patients received dual-axillary-areolar incisions (categorized as peri-areolar incision) or single axillary or lateral chest incisions. R-NSM usually adopts a single axillary incision or lateral chest incision
Statistical analysis
Baseline data were analyzed using chi-square tests (categorical data) or Student’s t-test (continuous data). The chi-square test analyzes the association between breast skin sensation and risk factors. All enrolled patients would receive at least one nipple or skin sensation evaluations, and for patients with more than one nipple and skin sensation assessment, the final evaluation score was used for the final risk factor evaluation analysis. Multivariate logistic regression was performed to assess the association of nipple or skin sensation with other factors. Results were considered statistically significant if the two-tailed P-value was < 0.05 for all tests. Statistical analysis was performed using SAS 9.4 version (SAS Inc., Cary, NC, USA).
Results
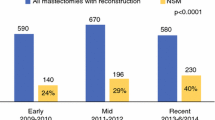
A total of 460 NSM procedures were enrolled in the current study, and their mean age was 48.3 ± 9.1 years old. There was 383 (83.3%) immediate breast reconstruction, and 77 cases (16.7%) were without breast reconstructions. One-hundred seventy-four (37.8%) received C-NSM, 195 (42.4%) E-NSM, and 91 (19.8%) were R-NSM procedures. The mean body mass index (BMI) was 23.7 ± 3.7, and 116 (27.1%) received radiotherapy after surgery. The clinicopathologic factors were summarized in Table 1.
All NSM procedures with nipple sensation assessed were evaluated at a mean of 42.4 ± 32.5 months post-operation (time since surgery). Fifteen (3.3%) cases were graded as 0, 18.2% (83/460) grade I, 49.7% (229/460) grade II, and 28.9% (133/460) grade III. The overall mean score of nipple sensation was 2.1 ± 0.7, and the average grade score of skin sensation over four quadrants was 2.1 ± 0.7 (Table 2) as well.
In analysis of different surgical approaches, preserved or normal (grade III) nipple sensation rate was 36.2% (63/174) in C-NSM group, 26.7% (52/195) in E-NSM group, and 19.7% (18/91) in the R-NSM group (P = 0.06, Table 2). It has to be noted that “time since surgery to last evaluation” was noted to be significantly longer in the C-NSM group (45.6 ± 34 months) or E-NSM group (44.7 ± 35.8 months) as compared to R-NSM group (31.8 ± 16 months, P < 0.01). (C-NSM group (45.6 ± 34 months) compared with E-NSM group (44.7 ± 35.8 months) was not statistically significant, P = 0.79.) In terms of surgical wound placement, preserved nipple sensation was noted to be 23.9% (17/71) in the upper outer oblique (radial) incision group (time since surgery: 54.6 ± 32.7 months), 38.5% (60/156) in the peri-areolar-related incision group (54.2 ± 37.8 months), 33.3% (6/18) in the inframammary fold incision group (44.8 ± 43.6 months), and 23.3% (50/216) in the single axillary or lateral chest incision (29.63 ± 20.6 months; nipple sensation: P = 0.04, time since surgery: P = 0.01, Table 2).
As for factors related to preserved nipple sensation, 133 (28.9%) grade III nipple sensation NSM procedures group were compared with 327 (71.1%) abnormal nipple sensation group (Table 3). The statistically significant factors for nipple-related sensation are age (50.4 ± 9 versus 47.5 ± 9, P < 0.01), tumor location (P = 0.03), different BMI categories (P = 0.04), different surgical methods (P = 0.01), axillary staging method (P = 0.04), surgical wound location (0.01), and follow-up duration (52.1 ± 32.4 versus 38.4 ± 31.8 months, P < 0.01). Statistically significant differences in skin sensation were found in different surgical methods (P < 0.01), surgical wound locations (P < 0.01), adjuvant radiotherapy (P = 0.01), and follow-up duration (48.5 ± 32.6 versus 39.2 ± 32.1 months, P < 0.01).
Of these 460 NSM procedures, 29 (6.4%) had transient nipple ischemia and 32(6.9%) with partial nipple necrosis. There was no direct correlation between nipple ischemia/necrosis and subsequent nipple sensation. Possible factors of nipple or skin sensation were further validated in univariate and multivariate analysis (Table 4). In univariate analysis, surgical methods, wound location, and follow-up time were noted as significant risk factors. In multivariate analysis, longer follow-up time showed significantly improved nipple or skin sensation (> 60 versus ≦ 12 months: nipple odds ratio (OR) = 5.75, P < 0.01; skin: OR = 1.97, p < 0.05). Peri-areolar wound location showed higher nipple sensation (OR: 2.1, P = 0.02), while single axillary or lateral chest incision showed decreased skin sensation (OR: 0.4, P < 0.01) when compared with the upper outer quadrant incision (Table 4). The R-NSM group showed decreased nipple (OR = 0.4, P < 0.01) or skin (OR = 0.16, P < 0.01) sensation, and E-NSM group also had lower skin sensation (OR = 0.42, P < 0.01) compared with C-NSM group.
The results of the current study were summarized and compared with other reported series in the literature as shown in Table 5.
Discussion
In this current study, 460 cases NSM procedures from Aug 2011 to April 2022 were enrolled and with clear evaluations of the impact of time lapses on the recovery of nipple or skin sensation. The mean follow-up duration of 42.4 ± 32.5 months (ranged: 1–143) was adequate to evaluate the recovery of skin or nipple sensation. In all cases, the sensation assessment evaluation uses “five areas measurement points” (Fig. 2). With 230 cases having more than one measurement time (some patients even had more than five times evaluated throughout the follow-up), 28.9% (133/460) and 34.5% (159/460) of the NSM procedures retained nipple sensations and skin sensations (grade III), respectively.
Recent studies on the incidence of nipple and skin sensation loss or recovery have varied and inconclusive results due to different maneuvers used and timing of sensation assessment among different reported studies (Table 5). The reported nipple sensation ranged from 10 to 75% (Table 5) [7,8,9, 19, 23,24,25]. In general, the skin had superior filament discrimination compared to the NAC. A study evaluating 150 healthy women regarding normal breast sensitivity found that the skin of the superior quadrant was the most sensitive part of the breast, followed by the areola, and the least sensitive part was the nipple [26]. Nonetheless, we found that the mean average grade score of breast skin sensation post-NSM over four quadrants was 2.1 ± 0.7, which was similar to the nipple sensation (2.1 ± 0.7, Table 2) in our study.
From univariate and multivariate analysis in our study, factors related to nipple or skin sensation were surgical approaches, wound incision types, and long follow-up duration (Tables 3 and 4). In a recently published RCT [14], R-NSM was associated with better preserved nipple sensation than C-NSM (31.6% versus 0%, P = 0.0002). In the current study, the preserved (grade III) nipple sensation rate was 36.2% (63/174) in the C-NSM group (mean follow up time 45.6 ± 34 months), 26.7% (52/195) in the E-NSM group (44.7 ± 35.8 months), and 19.7% (18/91) in the R-NSM (31.8 ± 16 months) group (nipple sensation: P = 0.06, follow up duration: P < 0.01 (C-NSM or E-NSM versus R-NSM), Table 2). In multivariate analysis, E-NSM or R-NSM showed decreased nipple or skin sensation if compared with C-NSM (Table 4). For patients who received R-NSM or E-NSM (since 2014) procedures, single axillary (or lateral chest incision) was the most frequently adopted incision type, however, which was associated with significantly decreased skin sensation. Peri-areolar incision showed significantly better nipple sensation than upper outer incision (Tables 3 and 4), which was rarely reported before, if any.
“Time from surgery to last evaluation” was a significant factor associated with sensation recovery or preservation in nipple (52.1 ± 32.4 versus 38.4 ± 31.8, P < 0.01) or skin sensation (48.5 ± 32.6 versus 39.2 ± 32.1, P < 0.01) post NSM. In multivariate analysis, follow-up duration is a significant factor in preserving nipple (OR = 5.75, P < 0.01) or skin (OR = 1.97, P < 0.05) sensation. In subgroup analysis of different surgical methods on the impact of nipple or skin sensation, there was significantly longer follow-up duration in C-NSM group (45.6 ± 34 months) or E-NSM (44.7 ± 35.8 months) than R-NSM (31.8 ± 16) group (P < 0.01, Table 2). The concept of “time since surgery” is associated with improved nipple sensation. Rodriguez-Unda et al. [27] suggested that factors such as age, time since surgery, and surgical approach have been linked to nerve regeneration. Shridharani et al. [28] showed that the sensory nerve of the nipple and skin flap “need time” to reinnervation. The actual time needed was unclear; however, it showed progressive improvement of constant touch over time with a lag period of the first 12 months. It seems that it takes 18 to 24 months of sensory recovery after breast reconstruction. These assumptions were consistent with our findings of follow-up time and nipple sensation in Table 4.
The sensory nerves of the NAC and breast skin come from lateral and cutaneous branches of the 3rd–5th intercostal nerves (mainly the 4th lateral cutaneous branch). The lateral cutaneous branches were a greater branch that took a deep course from muscle penetrating breast parenchyma and pierced to the posterior surface of nipple [29,30,31,32,33]. Montagne and Macpherson et al. [34] demonstrated that the neural elements concentrate at the base of the nipple, with few at the side of the nipple and even fewer in the areolar. Therefore, it is unsurprising how nipple and skin sensations were lost or diminished after NSM [35, 36], especially when retro-areolar tissue sampling was performed for intraoperative frozen section.
In the current study, nipple and skin flap sensation differed according to different surgical incisions and operation methods, which was rarely discussed before. E-NSM or R-NSM did not showed improved nipple or skin sensation than C-NSM even in multivariate analysis (Tables 2, 3 and 4). Skin incision and types of operations were highly correlated. A single axillary or lateral chest incision, which was frequently the preferred incision in E-NSM or R-NSM procedures, and upper-outer, inframammary, or peri-areolar incisions were frequently used by C-NSM procedures (Fig. 3). In multivariate analysis, peri-areolar incision showed significantly higher nipple sensation preservation, while singe axillary or lateral chest incision showed significantly decrease skin sensation (Table 4). Based on the anatomic basis of nerve supply, the single axilla or lateral chest incision, which started dissection from a “lateral to medial” fashion with incision lateral to the lateral border of the breast, might increase the risk of injury of the lateral cutaneous branches of 4th intercostal nerve when coursing into the breast [19]. The dissection plane of peri-areolar, inframammary, or upper outer incision started “medial to lateral” and usually stopped at the lateral border of the breast, which might help in preserving the entry of the lateral cutaneous branch of 4th intercostal nerve and therefore led to higher preservation of skin sensation.
The peri-areolar incision was associated with higher nipple sensation in multivariate analysis (Table 4). In our current study, sub-nipple samplings were routinely performed to prevent occult cancer left behind NAC. Peri-areolar incision was associated with higher risk of NAC ischemia necrosis, and surgeons tend to leave thicker skin flap to avoid over-thinning of retro-areolar tissue and subsequent NAC total necrosis. However, in E-NSM or R-NSM, the risk of total NAC necrosis was decreased due to the placement of skin incision far away from NAC, and usually, the skin flap beneath NAC was thinner due to oncologic safety consideration. These unique technical differences might have contributed to the observation of higher nipple sensation preservation in peri-areolar incision (frequent used in C-NSM) than single axilla or lateral chest incision (usually used in E-NSM or R-NSM, Fig. 3, Tables 3 and 4).
In some studies, there was hypothesis that the factors contributing to nipple necrosis might be correlated with loss of nipple sensation as well owing to the virtue of related neurovascular bundle anatomy when dissecting the superficial breast and skin fascia [20, 21, 37]. However, we found no correlations between NAC ischemia necrosis grading and nipple or skin sensation post-NSM (Table 3). Post-mastectomy radiotherapy (PMRT) was indicated in patients with poorer prognostic factors, like tumor size > 5 cm or lymph nodes metastasis, to decrease disease recurrence and prolonged survival [22]. There was 27% of NSM procedures in the current cohort who received PMRT, but these were not associated with lower preservation of nipple sensation. In contrast, we observed a higher preserved skin sensation in patients who received PMRT (41.3% versus 31.9%, P = 0.01). These findings were consistent with Khan et al. [7], which showed that PMRT did not deteriorate nipple or skin sensation.
In our current study, the focus is on nipple and skin sensation post NSM, and the authors successfully identified factors associated with preserved nipple or skin sensation with further validation of the relationship between nipple or skin sensation recovery to the duration of “time since surgery.” Our study is limited due to its retrospective nature, small sample size, and possible selection bias. Furthermore, the results of nipple or skin sensation test were subjective and not equally measured within a specific time period. However, our study enrolled a large number of NSM cases with detailed clinicopathologic, perioperative parameters, and different surgical approaches or incisions to enable us to have a comprehensive analysis of possible factors related to preserved nipple or skin sensation post NSM. A long-term follow-up of mean 42.4 ± 32.5 months also enabled us to show gradual recovery of nipple or skin sensation with different “time after surgery” period. Therefore, the results and information derived from the current study are valuable.
Conclusion
In our current study, the authors successfully demonstrated strong evidence that a significant improvement of nipple and skin sensation in patients who received NSM had to do with a longer “time after surgery” period. The results derived from this study will thus enable better discussion with patient regarding the impact of different operations methods and skin incision on skin and nipple sensation. This is definitely valuable in improving patients’ outcomes and QoL following NSM, especially in an era of shared decision-making prior to surgery.
Availability of data and materials
The data used in the current study could be provided by request to the principal investigator HWL after acceptance of the manuscript.
Abbreviations
- NSM:
-
Nipple-sparing mastectomy
- C-NSM:
-
Conventional NSM
- E-NSM:
-
Endoscopic-assisted NSM
- R-NSM:
-
Robotic-assisted NSM
- NAC:
-
Nipple areolar complex
- OR:
-
Odds ratio
- SSM:
-
Skin-sparing mastectomy
- CCH:
-
Changhua Christian Hospital
- IRB:
-
Institutional review board
- QoL:
-
Quality of life
References
Djohan R, Gage E, Gatherwright J, Pavri S, Firouz J, Bernard S, Yetman R. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg. 2010;125(3):818–29. https://doi.org/10.1097/PRS.0b013e3181ccdaa4.
Mesdag V, Régis C, Tresch E, Chauvet MP, Boulanger L, Collinet P, Giard S. Nipple sparing mastectomy for breast cancer is associated with high patient satisfaction and safe oncological outcomes. J Gynecol Obstet Hum Reprod. 2017;46(8):637–42. https://doi.org/10.1016/j.jogoh.2017.07.003.
Agha RA, Al Omran Y, Wellstead G, Sagoo H, Barai I, Rajmohan S, Borrelli MR, Vella-Baldacchino M, Orgill DP, Rusby JE. Systematic review of therapeutic nipple-sparing versus skin-sparing mastectomy. BJS Open. 2018;3(2):135–45. https://doi.org/10.1002/bjs5.50119.
Galimberti V, Vicini E, Corso G, Morigi C, Fontana S, Sacchini V, Veronesi P. Nipple-sparing and skin-sparing mastectomy: review of aims, oncological safety and contraindications. Breast. 2017;34 Suppl 1(Suppl 1):S82–4. https://doi.org/10.1016/j.breast.2017.06.034.
Headon HL, Kasem A, Mokbel K. The oncological safety of nipple-sparing mastectomy: a systematic review of the literature with a pooled analysis of 12,358 procedures. Arch Plast Surg. 2016;43(4):328–38. https://doi.org/10.5999/aps.2016.43.4.328.
Gerber B, Krause A, Dieterich M, Kundt G, Reimer T. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg. 2009;249(3):461–8. https://doi.org/10.1097/SLA.0b013e31819a044f.
Khan A, Zhang J, Sollazzo V, Mohammed K, Gui G. Sensory change of the reconstructed breast envelope after skin-sparing mastectomy. Eur J Surg Oncol. 2016;42(7):973–9. https://doi.org/10.1016/j.ejso.2016.03.018.
Akdeniz Dogan Z, Farhadi J. Evaluation of sensation on mastectomy skin flaps following immediate breast reconstruction. J Reconstr Microsurg. 2020;36(6):420–5. https://doi.org/10.1055/s-0040-1702157.
Gahm J, Hansson P, Brandberg Y, Wickman M. Breast sensibility after bilateral risk-reducing mastectomy and immediate breast reconstruction: a prospective study. J Plast Reconstr Aesthet Surg. 2013;66(11):1521–7. https://doi.org/10.1016/j.bjps.2013.06.054.
Peled AW, Duralde E, Foster RD, Fiscalini AS, Esserman LJ, Hwang ES, Sbitany H. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg. 2014;72(Suppl 1):S48-52. https://doi.org/10.1097/SAP.0000000000000020.
Casaubon JT, Kuehn RB, Pesek SE, Raker CA, Edmonson DA, Stuckey A, Gass JS. Breast-specific sensuality and appearance satisfaction: comparison of breast-conserving surgery and nipple-sparing mastectomy. J Am Coll Surg. 2020;230(6):990–8. https://doi.org/10.1016/j.jamcollsurg.2020.02.048.
Lai HW, Lee YY, Chen ST, Liao CY, Tsai TL, Chen DR, Lai YC, Kao WP, Wu WP. Nipple-areolar complex (NAC) or skin flap ischemia necrosis post nipple-sparing mastectomy (NSM)-analysis of clinicopathologic factors and breast magnetic resonance imaging (MRI) features. World J Surg Oncol. 2023;21(1):23. https://doi.org/10.1186/s12957-023-02898-x.
Park HS, Lee J, Lai HW, Park JM, Ryu JM, Lee JE, Kim JY, Marrazzo E, De Scalzi AM, Corso G, Montemurro F, Gazzetta G, Pozzi G, Toesca A. Surgical and oncologic outcomes of robotic and conventional nipple-sparing mastectomy with immediate reconstruction: International Multicenter Pooled Data Analysis. Ann Surg Oncol. 2022;29(11):6646–57. https://doi.org/10.1245/s10434-022-11865-x. Epub 2022 May 18.
Chirappapha P, Petit JY, Rietjens M, De Lorenzi F, Garusi C, Martella S, Barbieri B, Gottardi A, Andrea M, Giuseppe L, Hamza A, Lohsiriwat V. Nipple sparing mastectomy: does breast morphological factor related to necrotic complications? Plast Reconstr Surg Glob Open. 2014;2(1):e99. https://doi.org/10.1097/GOX.0000000000000038.
Shaffer K, Danko M, DeLaere A, Chant E, Pople B, Grisby S, Dekhne N. Patient satisfaction following nipple-sparing mastectomy and assessment of nipple-areolar sensation. Breast J. 2019;25(3):542–4. https://doi.org/10.1111/tbj.13274.
Dossett LA, Lowe J, Sun W, Lee MC, Smith PD, Jacobsen PB, Laronga C. Prospective evaluation of skin and nipple-areola sensation and patient satisfaction after nipple-sparing mastectomy. J Surg Oncol. 2016;114(1):11–6. https://doi.org/10.1002/jso.24264.
Hammond JB, Kandi LA, Armstrong VL, Kosiorek HE, Rebecca AM, Casey WJ 3rd, Kruger EA, Cronin PA, Pockaj BA, Teven CM. Long-term breast and nipple sensation after nipple-sparing mastectomy with implant reconstruction: relevance to physical, psychosocial, and sexual well-being. J Plast Reconstr Aesthet Surg. 2022;75(9):2914–9. https://doi.org/10.1016/j.bjps.2022.06.034.
Toesca A, Sangalli C, Maisonneuve P, Massari G, Girardi A, Baker JL, Lissidini G, Invento A, Farante G, Corso G, Rietjens M, Peradze N, Gottardi A, Magnoni F, Bottiglieri L, Lazzeroni M, Montagna E, Labo P, Orecchia R, Galimberti V, Intra M, Sacchini V, Veronesi P. A randomized trial of robotic mastectomy versus open surgery in women with breast cancer or BrCA mutation. Ann Surg. 2022;276(1):11–9. https://doi.org/10.1097/SLA.0000000000004969.
Benediktsson KP, Perbeck L, Geigant E, Solders G. Touch sensibility in the breast after subcutaneous mastectomy and immediate reconstruction with a prosthesis. Br J Plast Surg. 1997;50(6):443–9. https://doi.org/10.1016/s0007-1226(97)90332-5.
Würinger E. Secondary reduction mammaplasty. Plast Reconstr Surg. 2002;109(2):812–4. https://doi.org/10.1097/00006534-200202000-00064.
Komorowski AL, Zanini V, Regolo L, Carolei A, Wysocki WM, Costa A. Necrotic complications after nipple- and areola-sparing mastectomy. World J Surg. 2006;30(8):1410–3. https://doi.org/10.1007/s00268-005-0650-4.
Li Y, Moran MS, Huo Q, Yang Q, Haffty BG. Post-mastectomy radiotherapy for breast cancer patients with t1–t2 and 1–3 positive lymph nodes: a meta-analysis. PLoS One. 2013;8(12):e81765. https://doi.org/10.1371/journal.pone.0081765.
Longo B, Campanale A, di Pompeo Santanelli F. Nipple-areola complex cutaneous sensitivity: a systematic approach to classification and breast volume. J Plast Reconstr Aesthet Surg. 2014;67(12):1630–6. https://doi.org/10.1016/j.bjps.2014.08.043.
Howard MA, Sisco M, Yao K, Winchester DJ, Barrera E, Warner J, Jaffe J, Hulick P, Kuchta K, Pusic AL, Sener SF. Patient satisfaction with nipple-sparing mastectomy: a prospective study of patient reported outcomes using the BREAST-Q. J Surg Oncol. 2016;114(4):416–22. https://doi.org/10.1002/jso.24364.
Peled AW, Amara D, Piper ML, Klassen AF, Tsangaris E, Pusic AL. Development and validation of a nipple-specific scale for the BREAST-Q to assess patient-reported outcomes following nipple-sparing mastectomy. Plast Reconstr Surg. 2019;143(4):1010–7. https://doi.org/10.1097/PRS.0000000000005426.
Tairych GV, Kuzbari R, Rigel S, Todoroff BP, Schneider B, Deutinger M. Normal cutaneous sensibility of the breast. Plast Reconstr Surg. 1998;102(3):701–4. https://doi.org/10.1097/00006534-199809030-00013.
Rodriguez-Unda NA, Bello RJ, Clarke-Pearson EM, Sanyal A, Cooney CM, Manahan MA, Rosson GD. Nipple-sparing mastectomy improves long-term nipple but not skin sensation after breast reconstruction: quantification of long-term sensation in nipple sparing versus non-nipple sparing mastectomy. Ann Plast Surg. 2017;78(6):697–703. https://doi.org/10.1097/SAP.0000000000000900.
Shridharani SM, Magarakis M, Stapleton SM, Basdag B, Seal SM, Rosson GD. Breast sensation after breast reconstruction: a systematic review. J Reconstr Microsurg. 2010;26(5):303–10. https://doi.org/10.1055/s-0030-1249313.
Sarhadi NS, Shaw-Dunn J, Soutar DS. Nerve supply of the breast with special reference to the nipple and areola: Sir Astley Cooper revisited. Clin Anat. 1997;10(4):283–8. https://doi.org/10.1002/(SICI)1098-2353(1997)10:4%3c283::AID-CA12%3e3.0.CO;2-G.
Riccio CA, Zeiderman MR, Chowdhry S, Brooks RM, Kelishadi SS, Tutela JP, Choo J, Yonick DV, Wilhelmi BJ. Plastic surgery of the breast: keeping the nipple sensitive. Eplasty. 2015;2(15):e28.
Bijkerk E, Cornelissen AJM, Sommer M, Van Der Hulst RRWJ, Lataster A, Tuinder SMH. Intercostal nerve block of the anterior cutaneous branches and the sensibility of the female breast. Clin Anat. 2020;33(7):1025–32. https://doi.org/10.1002/ca.23532.
Schlenz I, Kuzbari R, Gruber H, Holle J. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105(3):905–9. https://doi.org/10.1097/00006534-200003000-00012.
O’Connell RL, Rusby JE. Anatomy relevant to conservative mastectomy. Gland Surg. 2015;4(6):476–83. https://doi.org/10.3978/j.issn.2227-684X.2015.02.06.
Montagna W, Macpherson EE. Proceedings: some neglected aspects of the anatomy of human breasts. J Invest Dermatol. 1974;63(1):10–6. https://doi.org/10.1111/1523-1747.ep12677284.
Jaspars JJ, Posma AN, van Immerseel AA, Gittenberger-de Groot AC. The cutaneous innervation of the female breast and nipple-areola complex: implications for surgery. Br J Plast Surg. 1997;50(4):249–59. https://doi.org/10.1016/s0007-1226(97)91155-3.
Sarhadi NS, Shaw-Dunn J, Soutar DS. Nerve supply of the breast with special reference to the nipple and areola: Sir Astley Cooper revisited. Clin Anat. 1997;10(4):283–8. https://doi.org/10.1002/(SICI)1098-2353(1997)10:4%3c283::AID-CA12%3e3.0.CO;2-G.
Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101(6):1486–93. https://doi.org/10.1097/00006534-199805000-00009.
Acknowledgements
The authors would like to thank Chin-Mei Tai, Yi-Ru Ke, Yi-Yuan Lee, An-Ting Yeh, Yun-Ting Chang, Chi Wei Mok, and Shu-Hsin Pai for their assistance in this study.
Funding
This study was funded by the Ministry of Science and Technology of Taiwan, and the number of this funding was MOST 111–2314-B-371–010. This study also sponsors research funding provided by the Changhua Christian Hospital 109-CCH-IRP-093, 110-CCH-IRP-042, 111-CCH-IRP-087, and 112-CCH-IRP-051.
Author information
Authors and Affiliations
Contributions
HWL, KC, FTFC, YLC were responsible for the Study concept. SLL, DYF, FTFC, YLC were covering the Data collection. STC, DRC, SIH, FTFC were major for the Statics analysis. HWL, KC, MHS, CWM are responsible for manuscript writing. FTFC, MHS, HIY, CWM are responsible for manuscript review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of CCH (CCH IRB No.:190414). All patients provided written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lai, HW., Chang, YL., Chandrachamnong, K. et al. Factors associated with alteration of nipple or skin sensation and impact of duration of time following nipple-sparing mastectomy (NSM): an analysis of 460 cases with comparison of conventional versus endoscopic- or robotic-assisted NSM. World J Surg Onc 21, 222 (2023). https://doi.org/10.1186/s12957-023-03107-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03107-5