Abstract
Purpose of Review
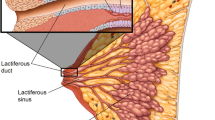
In patients undergoing mastectomy, benefits of nipple preservation include improved esthetics and quality of life. The purpose of this review is to evaluate the oncologic safety of nipple-sparing mastectomy (NSM) in women with breast cancer, focusing on complications, recurrence, and patient reported outcomes.
Recent Findings
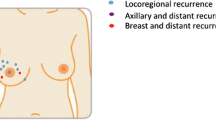
Clinical presentation, risk factors for nipple involvement, and preoperative imaging may be helpful in choosing appropriate candidates. Recent series suggest that complications after NSM are slightly increased when compared to traditional mastectomy but likely related to increased risk of nipple necrosis. Pathologic assessment of the nipple is necessary. Local recurrence after NSM appears similar to patients after traditional mastectomy; however, studies evaluating local recurrence are of lower quality and have short follow-up. NSM is associated with improved psychosocial and sexual well-being after surgery.
Summary
Studies evaluating oncologic safety of therapeutic NSM suggest that it is a viable option for appropriate patients, as risk of local recurrence and survival appears to be similar to patients undergoing traditional mastectomy. However, careful patient selection is critical.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wei CW, Scott AM, Price AN, et al. Psychosocial and sexual well-being following nipple-sparing mastectomy and reconstruction. Breast J. 2016;22(1):10–7.
Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. NEJM. 1999;340:77–84.
•• Agha RA, Al Omran Y, Wellstead G, et al. Systematic review of therapeutic nipple-sparing mastectomy versus skin sparing mastectomy. BJS Open. 2019;3:135–45 Most recent and extensive systematic review of 14 studies, demonstrated higher risk of complications with NSM but no statistical difference in LR (p=0.45) or mortality (p=0.34).
National Comprehensive Cancer Network. Breast cancer (Version 5.2020). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. .
Cense HA, Rutgers EJ, Cardozo ML, Van Lanschot JJ. Nipple-sparing mastectomy in breast cancer: a viable option? EJSO. 2001;27:521–6.
Jun S, Bae SJ, Yoon JC, et al. Significance of non-mass enhancement in the subareolar region on preoperative breast magnetic resonance imaging for nipple-sparing mastectomy. Clin Breast Cancer. 2020; epublished ahead of print.
Mariscotti G, Durando M, Houssami N, et al. Preoperative MRI evaluation of lesion nipple distance in breast cancer patients: thresholds for predicting occult nipple areola complex involvement. Clin Radiol. 2018;73:735e–45e.
Daar DA, Abdou SA, Rosario L, et al. Is there a preferred incision location for nipple-sparing mastectomy? A systematic review and meta-analysis. Plast Reconstr Surg. 2019:906e–19e.
Suarez-Zamora DS, Barrera-Herrera LE, Palau-Lazaro MA, et al. Accuracy and interobserver agreement of retroareolar frozen sections in nipple-sparing mastectomies. Ann Diagn Pathol. 2017;29:46–51.
Alperovich M, Choi M, Karp NS, Singh B, Ayo D, Frey JD, et al. Nipple-sparing mastectomy and sub-areolar biopsy: to freeze or not to freeze? Evaluating the role of sub-areolar intraoperative frozen section. Breast J. 2016;22(1):18–23.
Eisenberg RK, Chan JS, Swistel AJ, Hoda SA. Pathological evaluation of nipple-sparing mastectomies with emphasis on occult nipple involvement: the Weill-Cornell experience with 325 cases. Breast J. 2014;20(1):18–23.
Albright EL, Schroeder MC, Foster K, Sugg SL, Erdahl LM, Weigel RJ, et al. Nipple-sparing mastectomy is not associated with a delay of adjuvant treatment. Ann Surg Oncol. 2018;25(7):1928–35.
Wong SM, Chun YS, Sagara Y, Golshan M, Erdmann-Sager J. National patterns of breast reconstruction and nipple-sparing mastectomy for breast cancer, 2005–2015. Ann Surg Oncol. 2019;26:3194–203.
Headon HL, Kasem A, Mokbel K. The oncological safety of nipple-sparing mastectomy: a systematic review of the literature with a pooled analysis of 12,358 procedures. Arch Plast Surg. 2016;43:328–38.
Mota BS, Riera R, Ricci MD, et al. Nipple- and areola-sparing mastectomy for the treatment of breast cancer (review). Cochrane Database Syst Rev. 2016;11.
• Romanoff A, Zabor EC, Stempel M, et al. A comparison of patient-reported outcomes after nipple- sparing mastectomy and conventional mastectomy with reconstruction. Ann Surg Oncol. 2018;25(10):2909–16 This is a well-organized comparison of patient reported outcomes in this setting, demonstrated increased sexual and psychosocial well-being in women with NSM.
•• Wang M, Huang J, Chagpar AB. Is nipple sparing mastectomy associated with increased complications, readmission and length of stay compared to skin sparing mastectomy? Am J Surg. 2020;219(6):1030–5 Extensive evaluation of complications for patients undergoing NSM when compared to SSM. Showed higher rates of complications with NSM likely due to technical complexity but no difference in readmission rates or reoperations.
Park S, Yoon C, Bae SJ, et al. Comparison of complications according to incision types in nipple- sparing mastectomy and immediate reconstruction. Breast. 2020;53 E-published ahead of print.
Balci FL, Kara H, Dulgeroglu O, Uras C. Oncologic safety of nipple-sparing mastectomy in patients with short tumor-nipple distance. Breast J. 2019;25:612–8.
Garwood E, Moore D, Ewing C, et al. Total skin-sparing mastectomy complications and local recurrence rates in 2 cohorts of patients. Ann Surg. 2009;249(1):26–32.
Frey JD, Alperovich M, Levine JP, Choi M, Karp NS. Does smoking history confer a higher risk for reconstructive complications in nipple-sparing mastectomy? Breast J. 2017;23(4):415–20.
Bartholomew AJ, Dervishaj OA, Sosin M, Kerivan LT, Tung SS, Caragacianu DL, et al. Neoadjuvant chemotherapy and nipple-sparing mastectomy: timing and postoperative complications. Ann Surg Oncol. 2019;26:2768–72.
Alperovich M, Choi M, Frey JD, et al. Nipple-sparing mastectomy in patients with prior breast irradiation: are patients at higher risk for reconstructive complications? Plast Reconstr Surg. 2014;134(2):202e–6e.
Tang R, Coopey SB, Colwell AS, Specht MC, Gadd MA, Kansal K, et al. Nipple-sparing mastectomy in irradiated breasts: selecting patients to minimize complications. Ann Surg Oncol. 2015;22:3331–7.
Reish RG, Lin A, Phillips NA, Winograd J, Liao EC, Cetrulo CL Jr, et al. Breast reconstruction outcomes after nipple-sparing mastectomy and radiation therapy. Plast Reconstr Surg. 2015;135(4):959–66.
De La Cruz LM, Moody AM, Tappy EE, et al. Overall survival, disease-free survival, local recurrence, and nipple–areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015;22:3241–9.
Wu ZY, Kim HJ, Lee JW, Chung IY, Kim JS, Lee SB, et al. Breast cancer recurrence in the nipple-areola complex after nipple-sparing mastectomy with immediate breast reconstruction for invasive breast cancer. JAMA Surg. 2019;154(11):1030–7.
Jadeja P, Ha R, Rohde C, Ascherman J, Grant R, Chin C, et al. Expanding the criteria for nipple-sparing mastectomy in patients with poor prognostic features. Clin Breast Can. 2018;18(3):229–33.
Yoon-Flannery K, DeStefano LM, De La Cruz LM, et al. Quality of life and sexual well-being after nipple sparing mastectomy: a matched comparison of patients using the breast Q. J Surg Oncol. 2018;118:238–42.
Satteson ES, Brown BJ, Nahabedian MY. Nipple-areolar complex reconstruction and patient satisfaction: a systematic review and meta-analysis. Gland Surg. 2017;6(1):4–13.
Peled AW, Duralde E, Foster RD, et al. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg. 2014;72:S48–52.
Chirappapha P, Pongsakorn Srichan P, Lertsithichai P, et al. Nipple-areola complex sensation after nipple-sparing mastectomy. PRS Global Open. 2018;6(4):1–6.
Braun SE, Dreicer M, Butterworth JA, Larson KE. Do nipple necrosis rates differ in prepectoral versus submuscular implant-based reconstruction after nipple-sparing mastectomy? Ann Surg Oncol. 2020; Online ahead of print.
Galimberti V, Morigi C, Bagnardi V, Corso G, Vicini E, Fontana SKR, et al. Oncological outcomes of nipple-sparing mastectomy: a single-center experience of 1989 patients. Ann Surg Oncol. 2018;25(13):3849–57.
Lee CH, Cheng MH, Wu CW, Kuo WL, Yu CC, Huang JJ. Nipple-sparing mastectomy and immediate breast reconstruction after recurrence from previous breast conservation therapy. Ann Plast Surg. 2019;82:S95–S102.
Margenthaler JA, Gan C, Yan Y, Cyr AE, Tenenbaum M, Hook D, et al. Oncologic safety and outcomes in patients undergoing nipple-sparing mastectomy. J Am Coll Surg. 2020;230(4):535–41.
Metere A, Fabiani E, Lonardo MT, Giannotti D, Pace D, Giacomelli L. Nipple-sparing mastectomy long-term outcomes: Early and late complications. Medicina (Kaunas). 2020;56(4):166.
Parvez E, Martel K, Morency, et al. Surgical and oncologic outcomes of nipple-sparing mastectomy for a cohort of breast cancer patients, including cases with high-risk features. Clin breast Cancer. 2020; Online ahead of print.
Radovanovic Z, Ranisavljevic M, Radovanovic D, Vicko F, Ivkovic-Kapicl T, Solajic N. Nipple sparing mastectomy with primary implant reconstruction: surgical and oncological outcome of 435 breast cancer patients. Breast Care (Basel). 2018;13(5):373–8.
Young WA, Degnim AC, Hoskin TL, Jakub JW, Nguyen MD, Tran NV, et al. Outcomes of > 1300 nipple-sparing mastectomies with immediate reconstruction: The impact of expanding indications on complications. Ann Surg Oncol. 2019;26(10):3115–23.
Alsharif E, Ryu JM, Choi JH, et al. Oncologic outcomes of nipple-sparing mastectomy with immediate breast reconstruction in patients with tumor-nipple distance less than 2.0cm. J Breast Cancer. 2019;22(4):613–23.
Frey JD, Salibian AA, Lee J, Harris K, Axelrod DM, Guth AA, et al. Oncologic trends, outcomes and risk factors for locoregional recurrence: an analysis of tumor-to-nipple distance in critical factors in therapeutic nipple-sparing mastectomy. Plast Reconstr Surg. 2019;143(6):1575–85.
Valero MG, Muhsen S, Moo TA, Zabor EC, Stempel M, Pusic A, et al. Increase in utilization of nipple-sparing mastectomy for breast cancer: indications, complications and oncologic outcomes. Ann Surg Oncol. 2020;27(2):344–51.
Wu ZY, Kim HJ, Lee J, Chung IY, Kim JS, Lee SB, et al. Recurrence outcomes after nipple-sparing mastectomy and immediate breast reconstruction in patients with pure ductal carcinoma in situ. Ann Surg Oncol. 2020;27(5):1627–35.
Wu ZY, Kim HJ, Lee JW, et al. Oncologic outcomes of nipple-sparing mastectomy and immediate reconstruction after neoadjuvant chemotherapy for breast cancer. Ann Surg. 2020; Online ahead of print.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Local-Regional Evaluation and Therapy
Rights and permissions
About this article
Cite this article
Ludwig, K.K. Oncologic Safety of Nipple-Sparing Mastectomy for Patients with Breast Cancer. Curr Breast Cancer Rep 13, 35–41 (2021). https://doi.org/10.1007/s12609-020-00399-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00399-4